Up 3Rd Crm Report.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Environmental and Social Assessment with Management Plan Public Disclosure Authorized
SFG1690 V6 Environmental and Social Assessment with Management Plan Public Disclosure Authorized Sewerage Work at Bithoor Town, Kanpur Nagar (U.P.) Under National Ganga River Basin Authority (NGRBA) Public Disclosure Authorized Ministry of Water Resources, River Development & Ganga Rejuvenation, New Delhi Public Disclosure Authorized Clockwise from top: Valmiki Ashram, Brahmavart Ghat, Patthar Ghat, Dhruva Teela Public Disclosure Authorized Ganga Pollution Control Unit, Uttar Pradesh Jal Nigam June, 2015 ESAMP Report of Bithoor Sewerage Work under NGRBA Table of Contents TABLE OF CONTENTS .............................................................................................. I 1.0 EXECUTIVE SUMMARY ................................................................................. 1 1.1. Portfolio of Investments under NGRBA ............................................................................ 1 1.2. Sewerage Project for Bithoor Town of Kanpur ................................................................. 2 1.3. Policy, Legal and Administrative Framework ................................................................... 2 1.4. Requirement of Environmental Clearance as per EIA notification 14th September 2006: ......................................................................................................................................... 3 1.5. Baseline Environmental Condition ................................................................................... 3 1.6. Socio Economic Profile ................................................................................................... -

The Indian Jour of Agricultural Economics U
r"— .4,-7 • • ••••••- ••••• THE INDIAN JOUR OF AGRICULTURAL ECONOMICS U. S. DEPARTMENT' OF ht. (Organ of the Indian Society of Agricultural Economics) 1 Vol. XIV JANUARY—MARCH 1959 No. I CONTENTS ARTICLES Agricultural Economic Theory and Policy .R. Bellerby Recent Trends in the Yield of Rice and Wheat in India • • • • • • V; G. Panse Index of Cost of Cultivation .. S. D. Bokil A Statistical Study of the Rainfall Data at the four District Headquarter Stations of the former Bombay State during the period from D. S.Rangez Rao 1931-32 to 1955-56 • • V. N. Panditrao RESEARCH NOTES - Resource Earnings on Farms in Karchana Tehsil of Allahabad District, Estimated from Farm Survey Records _ • • A. Wycliffe Economic AsPects of Fertilization B. Vasanth Kumar Land Mortgage Banking in India • • C. B. Akkad GLEANINGS BOOK REVIEWS (see inside cover) R . 4.00 BOOK REVIEWS Page Bansil, P. C. India's Food Resources and V. M. Jakhade 85 Population Krishnaswamy, S Y. Food Production in India: b. A. Joshi 86 Principles and Problems Dube, S. C. , India's Changing Villages: Victor S. D'Souza 87 . .,••• .Human Factors in Comm- nity Development Desai, N. B. Report on the Administrative S. V. Ramanuirty 90 Survey of the Surat District EDITORIAL BOARD Prof. M. L. Dantwala Joint Editors Dr. M. B. Desai Shri V. M. Jakhade Shri G. B. Kulkarni Dr. G. D. Agrawal, The copyright and all rights of reproduction and translation of articles, book reviews and correspondence published in THE INDIAN JOURNAL OF AGRICULTURAL ECONOMICS are reserved by the Society. Application for permission to translate or reproduce any material contained in it should be made to the Honorary Secretary, The Indian Society of Agricultural Economics, 46-48, Esplanade Mansions, Mahatma Gandhi Road, Fort, Bombay-1. -

Itjjjjowtmcitts, Jfowf
Itjjjjowtmcitts, Jfowf, Cameron, Brigade-Surgn.-Lieut.-Col. A., Civil Surgn., on return from leave, to the .Benares district. Dobson, Surgn.-Major E. F. H., M.B., Civil Surgn., is posted to the Goalpara district with effect from the date of his return from leave. Anderson', Surgn.-Major J., Civil Surgn., Bareilly, to hold visiting medical charge of the Pilibhit district, in addition to his own duties, during the absence on leave of Surgn.- Major F. C. Chatterjee, or until further orders. Emerson, Surgn.-Major G. A., Civil Surgn., on return from leave, to the Fatelipur district. Henderson, Surgn.-Capt. S. H., Supernumerary Civil Surgn., Fatehpur, on relief by Surgn.-Major Gr. A. Emerson, to be attached for duty to the Central Prison, Bareilly, as a temporary measure. Chaytor-YVhite, Surgn.-Capt. J., Supernumerary Civil Surgn., Mirzapur, on relief by Surgn.-Major P. J. Freyer, is attached to the Allahabad district as a temporary measure. Buist-Sparks, Surgn.-Capt. A. W. T., is appointed to act as Civil Surgn. of Jalpaiguri, during the absence, on privi- lege leave, of Dr. J. L. Hendley, or until further orders. JD. Martin, Surgn.-Lieut.-Col. JN"., returned from the pri- vilege leave granted him by Order No. 7564, dated the 2Gth 128 INDIAN MEDICAL GAZETTE. [March 1895. October 1894. and resumed charge of the office of Civil PROMOTIONS. Surgn., Saugor. from Surgn.-Oapt. R. C. Macwatt on the To be Brigade-Surgeon-Lieutenant-Colonel. forenoon of the 6th instant. Smyth, Surgn.-Lieut.-Col. F. A., vice Bde.-Surgn.-Lieut.- Scotland, Surgn.-Oapt. D. W., Officiating Superintendent, Col. -

(13-05-2021) Second Dose (Vhdk Mrlo) District : Kanpur Nagar Name of Cold Name of Covid Capacity MOIC of Cold Chain Supervisor/MO Vaccination No
Covid-19 Vaccination Microplan Date - (13-05-2021) Second Dose (Vhdk mRlo) District : Kanpur Nagar Name of Cold Name of Covid Capacity MOIC of Cold Chain Supervisor/MO Vaccination No. of Chain Point/ Mob. No. Vaccine Dose Total Name of ANM Mobile No. Point/AEFI Duty Center/Session Site Walki Team AEFI Center Capacit Online CVC No. ng Center (CVC) y CVC CHC Kalyanpur CX Covaxin 2nd 120 0 0 1 Sarita 8318445314 45+ CVC CHC Kalyanpur CV Covishield 1st 200 200 0 1 Sumanlata 8707034561 18-44 CVC CHC Kalyanpur CV Covishield 2nd 120 0 120 1 Pushpa Gautam 8707067736 45+ CVC PHC Health Centre KNP UNIVERSITY CV Covishield 2nd 120 0 120 1 Vinodani harma 7839721796 DR AVINASH 1 Kalyanpur 9721788887 Dr Praveen Katiyar, 45+ YADAV 9415132492 CVC PHC Health Centre KNP UNIVERSITY CV 18- Covishield 1st 200 200 0 1 Smt Usha 9696461811 44 CVC PHC Panki CV 45+ Covishield 2nd 120 0 120 1 Premlata 9118718875 CVC PHC Bhauti CV 45+ Covishield 2nd 120 0 120 1 Manjali Mishra 6392899492 CVC PHC Bithoor CV 18- Covishield 1st 200 200 0 1 Kanchan Yadav 8318921399 44 CVC CHC Sarsaul CV 45+ Covishield 2nd 120 0 120 1 Neetu Singh 9621960962 CVC CHC Sarsaul CV 18- 2 Sarsaul DR S. L. VERMA 9956085896 Covishield 1st 100 100 0 1 Urmila Satyarthi 9335193780 44 CVC PHC Narwal CV 45+ Covishield 2nd 120 0 120 1 Deepmala 9473554340 CVC CHC Bidhnu CV 18- Covishield 1st 200 200 0 1 Priyanka Katiyar 8887721445 44 3 Bidhnu DR S. P. YADAV 9453229491 CVC CHC Bidhnu CV 45+ Covishield 2nd 120 0 120 1 Asha Verma 7839722214 CVC PHC Meharban Singh Covishield 2nd 120 0 120 1 Deep Mala 7839722217 Ka Purwa CV 45+ CVC CHC Bilhaur CV Covishield 1st 100 100 0 1 Abha Kumari 8303490430 18-44 DR ARVIND 4 Bilhaur 9897304629 CVC PHC Araul CV 45+ Covishield 2nd 120 0 120 1 Pragati katiyar 7007344273 BHUSAN CVC CHC Bilhaur CV 45+ Covishield 2nd 120 0 120 1 Smt. -

District Population Statistics, 22 Allahabad, Uttar Pradesh
.------·1 Census of India, 1951 I DISTRICT POPULATION STATISTICS UTTAR PRADESH 22-ALLAHABAD DISTRICT t I 315.42 ALLAHABAD: PluNnNG AND STATIONERY, UTTAR PRADESH, INDIA 1951 1953 ALL CPS Price, Re.1-S. FOREWORD THE Uttar Pradesh Government asked me in March, 1952, to supply them for the purposes of elections to local bodies population statistics with separation for scheduled castes (i) mohalla/ward -wise for urban areas, and (ii) village-wise for rural areas. The Census Tabulation Plan did not provide for sorting of scheduled castes population for areas smaller than a tehsil or urban tract and the request from the Uttar Pradesh Government came when the slip sorting had been finished and the Tabulation Offices closed. As the census slips are mixed up for the purposes of sorting in one lot for a tehsil or urban tract, collection of data regarding scheduled castes population by mohallas/wards and villages would have involved enormous labour and expense if sorting of the slips had been taken up afresh. Fortunately, however, a secondary census record, viz. the National Citizens' Register, in which each slip has been copied, was available. By singular foresight it had been pre pared mohalla/ward-wise for urban areas and village-wise for rural areas. The required information has, therefore, been extracted from this record. 2. In the above circumstances there is a slight difference in the figures of population as arrived at by an earlier sorting of the slips and as now determined by counting from the National Citizens' Register. This difference has been accen tuated by an order passed by me during the later count. -

(JIT) Report of National Horticulture Mission Scheme for Uttar Pradesh State State: Uttar Pradesh
Joint Inspection Team (JIT) Report of National Horticulture Mission Scheme For Uttar Pradesh State State: Uttar Pradesh 1 INDEX Sl.No Topic Page No. 1. General Observations 3 2. State:Uttar Pradesh -Introduction 4 3. Field Visits (i) Visit to Allahabad District 6 (ii) Visit to Kaushambi District 20 (iii) Visit to Varanasi District 39 (iv) Visit to Lucknow District 51 Dates of Visit:- 02.9.13 to 06.9.13 Team Members: 1. Dr. H.V.L Bathla, Chief Consultant (NHM), MoA, GoI, New Delhi. 2. Dr. A.K. Dubey, Professor CSAUA&T Kanpur. 3. Dr. Bhagwan Deen, Associate Professor NDUA&T Faizabad, 2 General Observations: There is delay in supply of planting material particularly tissue culture banana saplings to the farmers. Timely supply of planting material need to be ensured to the farmers because delayed planting of banana adversely affects the productivity as younger plants are more susceptible to frost. The infrastructure facilities like laboratories, equipments, net houses, poly houses etc created with the support of NHM at Banaras Hindu University and Horticulture Department of the State Government should be used for the benefit of the farmers also. Field visits and interaction of JIT with farmers revealed that farmers have not been advised properly by grass root level technical staffs accountable for execution of NHM. Rather than area expansion, emphasis should be given on rejuvenation of senile orchards, post harvest management, mechanization, establishment of processing units and plant nurseries. There is an immediate need to intensify the guava canopy management programme in Banaras and Allahabad districts. The benefits have been repeated either to the same farmers or to the members of same family. -

ALLAHABAD Address: 38, M.G
CGST & CENTRAL EXCISE COMMISSIONERATE, ALLAHABAD Address: 38, M.G. Marg, Civil Lines, Allahabad-211 001 Phone: 0532-2407455 E mail:[email protected] Jurisdiction The territorial jurisdiction of CGST and Central Excise Commissionerate Allahabad, extends to Districts of Allahabad, Banda, Chitrakoot, Kaushambi, Jaunpur, SantRavidas Nagar, Pratapgarh, Raebareli, Fatehpur, Amethi, Faizabad, Ambedkarnagar, Basti &Sultanpurof the state of Uttar Pradesh. The CGST & Central Excise Commissionerate Allahabad comprises of following Divisions headed by Deputy/ Assistant Commissioners: 1. Division: Allahabad-I 2. Division: Allahabad-II 3. Division: Jaunpur 4. Division: Raebareli 5. Division: Faizabad Jurisdiction of Divisions & Ranges: NAME OF JURISDICTION NAME OF RANGE JURISDICTION OF RANGE DIVISION Naini-I/ Division Naini Industrial Area of Allahabad office District, Meja and Koraon tehsil. Entire portion of Naini and Karchhana Area covering Naini-II/Division Tehsil of Allahabad District, Rewa Road, Ranges Naini-I, office Ghoorpur, Iradatganj& Bara tehsil of Allahabad-I at Naini-II, Phulpur Allahabad District. Hdqrs Office and Districts Jhunsi, Sahson, Soraon, Hanumanganj, Phulpur/Division Banda and Saidabad, Handia, Phaphamau, Soraon, Office Chitrakoot Sewait, Mauaima, Phoolpur Banda/Banda Entire areas of District of Banda Chitrakoot/Chitrako Entire areas of District Chitrakoot. ot South part of Allahabad city lying south of Railway line uptoChauphatka and Area covering Range-I/Division Subedarganj, T.P. Nagar, Dhoomanganj, Ranges Range-I, Allahabad-II at office Dondipur, Lukerganj, Nakhaskohna& Range-II, Range- Hdqrs Office GTB Nagar, Kareli and Bamrauli and III, Range-IV and areas around GT Road. Kaushambidistrict Range-II/Division Areas of Katra, Colonelganj, Allenganj, office University Area, Mumfordganj, Tagoretown, Georgetown, Allahpur, Daraganj, Alopibagh. Areas of Chowk, Mutthiganj, Kydganj, Range-III/Division Bairahna, Rambagh, North Malaka, office South Malaka, BadshahiMandi, Unchamandi. -
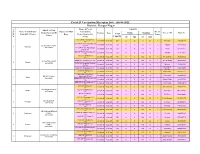
Covid-19 Vaccination Microplan Date - (06-08-2021) District : Kanpur Nagar Name of Covid Capacity MOIC of Cold Name of Cold Chain Supervisor/MO Vaccination No
Covid-19 Vaccination Microplan Date - (06-08-2021) District : Kanpur Nagar Name of Covid Capacity MOIC of Cold Name of Cold Chain Supervisor/MO Vaccination No. of Chain Point/ AEFI Vaccine Dose Online Walking Name of ANM Mobile No. Point/AEFI Center Duty Center/Session Site Total Team Center CVC No.CVC (CVC) Capacity 1st 2nd 1st 2nd CVC UPHC Kalyanpur CV Covishield 1st & 2nd 200 75 25 75 25 1 Moni Devi 7985632779 18+ KLY WP Pri Sch Baikunthpur 1st Covishield 1st & 2nd 150 0 0 140 10 1 Padma 8787075969 DR AVINASH YADAV CV 18+ 1 Kalyanpur 9721788887 KLY WP Pri Sch Baikunthpur Covishield 1st & 2nd 150 0 0 140 10 1 Hema 6387422915 2nd CV 18+ KLY WP Pri Sch Bharatpur CV Covishield 1st & 2nd 150 0 0 140 10 1 Premlata 9118718875 18+ CVC CHC Sarsaul CV Covishield 1st & 2nd 150 0 0 100 50 1 Neetu Singh 9621960962 18+ SARS WP Purwameer CV 18+ Covishield 1st & 2nd 150 0 0 140 10 1 Meena Singh 9889539889 Dr RAMESH KUMAR 2 Sarsaul 9410497490 SARS WP Naugawan Gautam Covishield 1st & 2nd 150 0 0 140 10 1 Mithlesh 9936577749 CV 18+ Shashikiran SARS WP Shikathiya CV 18+ Covishield 1st & 2nd 150 0 0 140 10 1 7080199608 Sachan CVC PHC Kathara CV Covishield 1st & 2nd 150 0 0 100 50 1 Asha Verma 7839722214 18+ BIDH WP Aanganwadi Covishield 1st & 2nd 150 0 0 140 10 1 Laxmi Devi 6386094073 DR S. P. YADAV Katheruaa CV 18+ 3 Bidhnu 9453229491 BIDH WP Pri Sch Katheruaa CV Covishield 1st & 2nd 150 0 0 140 10 1 Beena Singh 8429463299 18+ BIDH WP Pri Sch Hadhaha CV Covishield 1st & 2nd 150 0 0 140 10 1 Mala Singh 9935619510 18+ CVC CHC Bilhaur CV Covishield 1st & -

Impact of Urban Activity on Ganges Water Quality and Ecology: Case Study Kanpur
INTERUNIVERSITY PROGRAMME ADVANCED MASTER OF SCIENCE IN ‘TECHNOLOGY FOR INTEGRATED WATER MANAGEMENT’ Impact of urban activity on Ganges water quality and ecology: case study Kanpur Matthias Troch Stamnummer: 01205240 Promotor: Prof. dr. Ludo Diels Promotor: Prof. dr. Colin Janssen Master's dissertation submitted in partial fulfilment of the requirements for the degree of Master of Science in ‘Technology for Integrated Water Management’ Academic Year: 2017 - 2018 Acknowledgements Before reading my master dissertation, I would like to seize the opportunity to thank some people who helped and supported me during this study. First of all, I would like to thank my promotor, Prof. Dr. Ludo Diels. You gave me the opportunity to study the astonishing Ganges river. I greatly appreciate your support and readiness to answer my questions. I am very thankful for all your advice and the constructive discussions we had. For this, I am very grateful for having you as a promotor. I would also like to thank Prof. Dr. Vinod Tare, head of the Civil Engineering Department of IIT Kanpur. I greatly appreciate your hospitality and support during the preparation of the Ganges survey. I would like to express my gratitude to Steven Joosen. I am grateful for your help during the preparation of the Ganges survey and for providing the necessary lab equipment. I would like to thank the entire staff of the Civil Engineering Department of IIT Kanpur, especially Arvind Ashish and Rakesh Mishra. Without them, the practical realisation of the Ganges survey would be impossible. They put a lot of effort and time in helping me organising the presented field study. -

Impact Assessment
HEALTH CHECK UP CAMP UNDER CSR INITIATIVE OF ALIMCO IMPACT ASSESSMENT IMPLEMENTED BY HLL LIFECARE LIMITED IMPACT ASSESSMENT STUDY FOR HEALTH CHECK UP CAMPS CONDUCTED ON BEHALF OF ALIMCO APRIL 2017 – A REPORT BY DR. NISHI PRAKASH, Head of Department of Sociology, Associate Professor SN SEN BV PG College, Kanpur, Uttar Pradesh Origin of Inquiry: HLL Lifecare Limited Date of Inquiry: April 17, 2017 FOR HLL LIFECARE LIMITED This Impact Assessment study was initiated at the request of HLL Lifecare Limited, (A Govt. of India Enterprise) under administrative control of Ministry of Health and Family Welfare on April 17, 2017. This project was conducted as part of Corporate Social Responsibility (CSR) initiative of Artificial Limbs and Manufacturing Corporation of India, (A Govt. of India Undertaking) under administrative control of Ministry of Social Justice and Empowerment. The content of this report is to analyse the Health check-up camps conducted by HLL Lifecare Limited at Five locations at Kanpur, Nagar dated, from April 12, 2017 to April 16, 2017 at the following locations: 1. Chandrakeshwar Mandir, Berry Village, Naramau, Kanpur. 2. Maharana Institute of Professional Studies, Bithoor Road, Ishwari Ganj, Bithoor, Kanpur. 3. Royal Castle Guest House, Naya Shivli Road, Kalyanpur, Kanpur. 4. Shivrajpur Block Office, Shivrajpur, Kanpur. 5. Sanskrit Pathshala, Behlolpur, Mandhana, Kanpur. DR. NISHI PRAKASH Head of Department of Sociology Associate Professor SN SEN BV PG College Kanpur, Uttar Pradesh IMPACT OF THE PROJECT: PROS: After taking feedback from the Gram Pradhans / Parshad / Block Pramukh like Sanjay Batham ji, Rishi Dubey ji, Rajesh Kori ji it has been found that the initiative taken by ALIMCO was useful for them because most of the villagers were not aware of a healthy living and they don’t visit a doctor unless there is a need for them as a result, some of them were unknowingly carrier of diseases like Diabetes, High Blood pressure, Cardiology etc. -
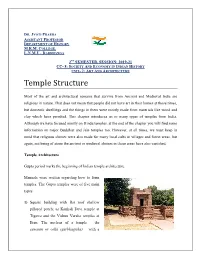
Temple Structure
DR. JYOTI PRABHA ASSISTANT PROFESSOR DEPARTMENT OF HISTORY M.R.M. COLLEGE, L.N.M.U., DARBHANGA 2ND SEMESTER, SESSION: 2019-21 CC- 8: SOCIETY AND ECONOMY IN INDIAN HISTORY UNIT- 2: ART AND ARCHITECTURE Temple Structure Most of the art and architectural remains that survive from Ancient and Medieval India are religious in nature. That does not mean that people did not have art in their homes at those times, but domestic dwellings and the things in them were mostly made from materials like wood and clay which have perished. This chapter introduces us to many types of temples from India. Although we have focused mostly on Hindu temples, at the end of the chapter you will find some information on major Buddhist and Jain temples too. However, at all times, we must keep in mind that religious shrines were also made for many local cults in villages and forest areas, but again, not being of stone the ancient or medieval shrines in those areas have also vanished. Temple Architecture Gupta period marks the beginning of Indian temple architecture. Manuals were written regarding how to form temples. The Gupta temples were of five main types: 1) Square building with flat roof shallow pillared porch; as Kankali Devi temple at Tigawa and the Vishnu Varaha temples at Eran. The nucleus of a temple – the sanctum or cella (garbhagriha) – with a single entrance and apporch (Mandapa) appears for the first time here. 2) An elaboration of the first type with the addition of an ambulatory (paradakshina) around the sanctum sometimes a second storey; examples the Shiva temple at Bhumara(M.P.) and the lad-khan at Aihole. -

Study of the Comparative Physico-Chemical Analysis of Potable and Polluted Ganga River Water at Kanpur in Reference to the Tannery Effluents Discharged in the River
J. Exp. Zool. India Vol. 14, No. 2, pp. 403-409, 2011 ISSN 0972-0030 STUDY OF THE COMPARATIVE PHYSICO-CHEMICAL ANALYSIS OF POTABLE AND POLLUTED GANGA RIVER WATER AT KANPUR IN REFERENCE TO THE TANNERY EFFLUENTS DISCHARGED IN THE RIVER Reeta Johri, Manjusha Dey and P. K. Johri Department of Zoology, D.A.V. College, Kanpur - 208 001, India. e mail : [email protected] (Accepted 18 February 2011) ABSTRACT – In Kanpur, river Ganga takes entry at Bithoor and passing along several ghats and lakes it exist at Jajmau covering a distance about 22 Km. The fish fauna in different region of river Ganga at Kanpur is of different categories according to a degree of pollution at various ghats. Therefore, for a study purpose a stretch of about 24 Km. of river Ganga is selected for the upper stream near Bithoor, middle stream to the Permat region and to the down stream at Kanpur near Jajmau up to new Jajmau bridge. The physico-chemical analysis of the water samples collected from upper, middle, and down streams of river Ganga from tannery area to Jajmau automobile transport bridge revealed that almost all the major characteristics were little beyond permissible limits. The water as such could not be used both for drinking and bathing purposes. It could only be used for irrigation in fields but after treatment. The low values of dissolved oxygen (8.993±8.50, 6.2±2.0 and 3.40±0.360) affected potability of water and caused mortality of fish and other aquatic animals in Bithoor, Permat and Jajmau, respectively.