Respiratory Humidification: Basics What Is Respiratory Humidification?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Infections of the Respiratory Tract
F70954-07.qxd 12/10/02 7:36 AM Page 71 Infections of the respiratory 7 tract the nasal hairs and by inertial impaction with mucus- 7.1 Pathogenesis 71 covered surfaces in the posterior nasopharynx (Fig. 11). 7.2 Diagnosis 72 The epiglottis, its closure reflex and the cough reflex all reduce the risk of microorganisms reaching the lower 7.3 Management 72 respiratory tract. Particles small enough to reach the tra- 7.4 Diseases and syndromes 73 chea and bronchi stick to the respiratory mucus lining their walls and are propelled towards the oropharynx 7.5 Organisms 79 by the action of cilia (the ‘mucociliary escalator’). Self-assessment: questions 80 Antimicrobial factors present in respiratory secretions further disable inhaled microorganisms. They include Self-assessment: answers 83 lysozyme, lactoferrin and secretory IgA. Particles in the size range 5–10 µm may penetrate further into the lungs and even reach the alveolar air Overview spaces. Here, alveolar macrophages are available to phagocytose potential pathogens, and if these are overwhelmed neutrophils can be recruited via the This chapter deals with infections of structures that constitute inflammatory response. The defences of the respira- the upper and lower respiratory tract. The general population tory tract are a reflection of its vulnerability to micro- commonly experiences upper respiratory tract infections, bial attack. Acquisition of microbial pathogens is which are often seen in general practice. Lower respiratory tract infections are less common but are more likely to cause serious illness and death. Diagnosis and specific chemotherapy of respiratory tract infections present a particular challenge to both the clinician and the laboratory staff. -

Maximum Expiratory Flow Rates in Induced Bronchoconstriction in Man
Maximum expiratory flow rates in induced bronchoconstriction in man A. Bouhuys, … , B. M. Kim, A. Zapletal J Clin Invest. 1969;48(6):1159-1168. https://doi.org/10.1172/JCI106073. Research Article We evaluated changes of maximum expiratory flow-volume (MEFV) curves and of partial expiratory flow-volume (PEFV) curves caused by bronchoconstrictor drugs and dust, and compared these to the reverse changes induced by a bronchodilator drug in previously bronchoconstricted subjects. Measurements of maximum flow at constant lung inflation (i.e. liters thoracic gas volume) showed larger changes, both after constriction and after dilation, than measurements of peak expiratory flow rate, 1 sec forced expiratory volume and the slope of the effort-independent portion of MEFV curves. Changes of flow rates on PEFV curves (made after inspiration to mid-vital capacity) were usually larger than those of flow rates on MEFV curves (made after inspiration to total lung capacity). The decreased maximum flow rates after constrictor agents are not caused by changes in lung static recoil force and are attributed to narrowing of small airways, i.e., airways which are uncompressed during forced expirations. Changes of maximum expiratory flow rates at constant lung inflation (e.g. 60% of the control total lung capacity) provide an objective and sensitive measurement of changes in airway caliber which remains valid if total lung capacity is altered during treatment. Find the latest version: https://jci.me/106073/pdf Maximum Expiratory Flow Rates in Induced Bronchoconstriction in Man A. Bouiuys, V. R. HuNTr, B. M. Kim, and A. ZAPLETAL From the John B. Pierce Foundation Laboratory and the Yale University School of Medicine, New Haven, Connecticut 06510 A B S T R A C T We evaluated changes of maximum ex- rates are best studied as a function of lung volume. -

Peak Flow Measure: an Index of Respiratory Function?
International Journal of Health Sciences and Research www.ijhsr.org ISSN: 2249-9571 Original Research Article Peak Flow Measure: An Index of Respiratory Function? D. Devadiga, Aiswarya Liz Varghese, J. Bhat, P. Baliga, J. Pahwa Department of Audiology and Speech Language Pathology, Kasturba Medical College (A Unit of Manipal University), Mangalore -575001 Corresponding Author: Aiswarya Liz Varghese Received: 06/12/2014 Revised: 26/12/2014 Accepted: 05/01/2015 ABSTRACT Aerodynamic analysis is interpreted as a reflection of the valving activity of the larynx. It involves measuring changes in air volume, flow and pressure which indicate respiratory function. These measures help in determining the important aspects of lung function. Peak expiratory flow rate is a widely used respiratory measure and is an effective measure of effort dependent airflow. Aim: The aim of the current study was to study the peak flow as an aerodynamic measure in healthy normal individuals Method: The study group was divided into two groups with n= 60(30 males and 30 females) in the age range of 18-22 years. The peak flow was measured using Aerophone II (Voice Function Analyser). The anthropometric measurements such as height, weight and Body Mass Index was calculated for all the participants. Results: The peak airflow was higher in females as compared to that of males. It was also observed that the peak air flow rate was correlating well with height and weight in males. Conclusions: Speech language pathologist should consider peak expiratory airflow, a short sharp exhalation rate as a part of routine aerodynamic evaluation which is easier as compared to the otherwise commonly used measure, the vital capacity. -

Introduction to Airway Resistance Measurements
Introduction to airway resistance measurements Dr. David Kaminsky Department of Medicine The University of Vermont VT 05405 Burlington UNITED STATES OF AMERICA [email protected] AIMS Review physiology of airway resistance Survey measures of airway resistance Provide examples of clinical applications Highlight research applications SUMMARY Airway resistance (Raw) is one of the fundamental features of the mechanics of the respiratory system. While the flow-volume loop offers insight into the volume and flow of air, it is limited in terms of specific information regarding lung mechanics. Airway resistance is the ratio of driving pressure divided by flow through the airways. It specifies the pressure required to achieve a flow of air with a velocity of 1L/sec. If the airway is represented by a simple, rigid tube, with laminar flow of air through it, the airway resistance Raw = (8 x L x )/ r4, where L = length of the tube, = viscosity of the gas, and r = radius of the tube. It is important to note that the r4 relationship demonstrates how sensitive resistance is to the size of the tube, varying inversely with the 4th power of the radius. The inner diameter of the airway is itself determined by many factors, including airway smooth muscle contractile state, airway wall thickness (related to inflammation, edema and remodeling), airway wall buckling and formation of mucosal folds, the interdependence, or linkage, of airway and surrounding lung parenchyma, and the intrinsic elastic recoil of the lung parenchyma, which serves as a load on the airway and variably resists bronchoconstriction. Of course, the airways are not rigid tubes, and in fact flow is a complex process involving both laminar and turbulent conditions, so this calculation of Raw is an approximation only. -
Spirometry Basics
SPIROMETRY BASICS ROSEMARY STINSON MSN, CRNP THE CHILDREN’S HOSPITAL OF PHILADELPHIA DIVISION OF ALLERGY AND IMMUNOLOGY PORTABLE COMPUTERIZED SPIROMETRY WITH BUILT IN INCENTIVES WHAT IS SPIROMETRY? Use to obtain objective measures of lung function Physiological test that measures how an individual inhales or exhales volume of air Primary signal measured–volume or flow Essentially measures airflow into and out of the lungs Invaluable screening tool for respiratory health compared to BP screening CV health Gold standard for diagnosing and measuring airway obstruction. ATS, 2005 SPIROMETRY AND ASTHMA At initial assessment After treatment initiated and symptoms and PEF have stabilized During periods of progressive or prolonged asthma control At least every 1-2 years: more frequently depending on response to therapy WHY NECESSARY? o To evaluate symptoms, signs or abnormal laboratory tests o To measure the effect of disease on pulmonary function o To screen individuals at risk of having pulmonary disease o To assess pre-operative risk o To assess prognosis o To assess health status before beginning strenuous physical activity programs ATS, 2005 SPIROMETRY VERSUS PEAK FLOW Recommended over peak flow meter measurements in clinician’s office. Variability in predicted PEF reference values. Many different brands PEF meters. Peak Flow is NOT a diagnostic tool. Helpful for monitoring control. EPR 3, 2007 WHY MEASURE? o Some patients are “poor perceivers.” o Perception of obstruction variable and spirometry reveals obstruction more severe. o Family members “underestimate” severity of symptoms. o Objective assessment of degree of airflow obstruction. o Pulmonary function measures don’t always correlate with symptoms. o Comprehensive assessment of asthma. -
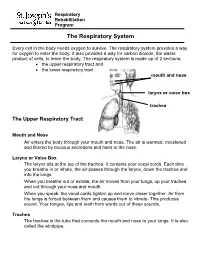
The Respiratory System
Respiratory Rehabilitation Program The Respiratory System Every cell in the body needs oxygen to survive. The respiratory system provides a way for oxygen to enter the body. It also provides a way for carbon dioxide, the waste product of cells, to leave the body. The respiratory system is made up of 2 sections: the upper respiratory tract and the lower respiratory tract mouth and nose larynx or voice box trachea The Upper Respiratory Tract Mouth and Nose Air enters the body through your mouth and nose. The air is warmed, moistened and filtered by mucous secretions and hairs in the nose. Larynx or Voice Box The larynx sits at the top of the trachea. It contains your vocal cords. Each time you breathe in or inhale, the air passes through the larynx, down the trachea and into the lungs. When you breathe out or exhale, the air moves from your lungs, up your trachea and out through your nose and mouth. When you speak, the vocal cords tighten up and move closer together. Air from the lungs is forced between them and causes them to vibrate. This produces sound. Your tongue, lips and teeth form words out of these sounds. Trachea The trachea is the tube that connects the mouth and nose to your lungs. It is also called the windpipe. The Lower Respiratory Tract Inside Lungs Outside Lungs bronchial tubes alveoli diaphragm (muscle) Bronchial Tubes The trachea splits into 2 bronchial tubes in your lungs. These are called the left bronchus and right bronchus. The bronchus tubes keep branching off into smaller and smaller tubes called bronchi. -

RESPIRATORY TRACT INFECTIONS Peter Zajac, DO, FACOFP, Author Amy J
OFP PATIENT EDUCATION HANDOUT RESPIRATORY TRACT INFECTIONS Peter Zajac, DO, FACOFP, Author Amy J. Keenum, DO, PharmD, Editor • Ronald Januchowski, DO, FACOFP, Health Literacy Editor HOME MANAGEMENT INCLUDES: • Drinking plenty of clear fuids and rest. Vitamin-C may help boost your immune system. Over-the-counter pain relievers such as acetaminophen and ibuprofen can be helpful for fevers and to ease any aches. Saline (salt) nose drops, lozenges, and vapor rubs can also help symptoms when used as directed by your physician. • A cool mist humidifer can make breathing easier by thinning mucus. • If you smoke, you should try to stop smoking for good! Avoid second-hand smoking also. • In most cases, antibiotics are not recommended because they are only effective if bacteria caused the infection. • Other treatments, that your Osteopathic Family Physician may prescribe, include Osteopathic Manipulative Therapy (OMT). OMT can help clear mucus, Respiratory tract infections are any relieve congestion, improve breathing and enhance comfort, relaxation, and infection that affect the nose, sinuses, immune function. and throat (i.e. the upper respiratory tract) or airways and lungs (i.e. the • Generally, the symptoms of a respiratory tract infection usually pass within lower respiratory tract). Viruses are one to two weeks. the main cause of the infections, but • To prevent spreading infections, sneeze into the arm of your shirt or in a tissue. bacteria can cause some. You can Also, practice good hygiene such as regularly washing your hands with soap and spread the infection to others through warm water. Wipe down common surfaces, such as door knobs and faucet handles, the air when you sneeze or cough. -

Role of the Allergist-Immunologist and Upper Airway Allergy in Sleep-Disordered Breathing
AAAAI Work Group Report Role of the Allergist-Immunologist and Upper Airway Allergy in Sleep-Disordered Breathing Dennis Shusterman, MD, MPHa, Fuad M. Baroody, MDb, Timothy Craig, DOc, Samuel Friedlander, MDd, Talal Nsouli, MDe, and Bernard Silverman, MD, MPHf; on behalf of the American Academy of Allergy, Asthma & Immunology’s Rhinitis, Rhinosinusitis and Ocular Allergy Committee Work Group on Rhinitis and Sleep-disordered Breathing San Francisco, Calif; Chicago, Ill; Hershey, Pa; Solon, Ohio; Washington, DC; and Brooklyn, NY BACKGROUND: Sleep-disordered breathing in general and RESULTS: Survey results were returned by 339 of 4881 active obstructive sleep apnea in particular are commonly encountered members (7%). More than two-third of respondents routinely conditions in allergy practice. Physiologically, nasal (or asked about sleep problems, believed that sleep-disordered nasopharyngeal) obstruction from rhinitis, nasal polyposis, or breathing was a problem for at least a “substantial minority” adenotonsillar hypertrophy are credible contributors to snoring (10%-30%) of their adult patients, and believed that medical and nocturnal respiratory obstructive events. Nevertheless, therapy for upper airway inflammatory conditions could existing practice parameters largely relegate the role of the potentially help ameliorate sleep-related complaints. Literature allergist to adjunctive treatment in cases of continuous positive review supported the connection between high-grade nasal airway pressure intolerance. congestion/adenotonsillar hypertrophy and obstructive sleep OBJECTIVES: To survey active American Academy of Allergy, apnea, and at least in the case of pediatric patients, supported the Asthma & Immunology members regarding their perceptions use of anti-inflammatory medication in the initial management and practices concerning sleep-disordered breathing in adult and of obstructive sleep apnea of mild-to-moderate severity. -

Respiratory Tract Infections in the Tropics
9.1 CHAPTER 9 Respiratory Tract Infections in the Tropics Tim J.J. Inglis 9.1 INTRODUCTION Acute respiratory infections are the single most common infective cause of death worldwide. This is also the case in the tropics, where they are a major cause of death in children under five. Bacterial pneumonia is particularly common in children in the tropics, and is more often lethal. Pulmonary tuberculosis is the single most common fatal infection and is more prevalent in many parts of the tropics due to a combination of endemic HIV infection and widespread poverty. A lack of diagnostic tests, limited access to effective treatment and some traditional healing practices exacerbate the impact of respiratory infection in tropical communities. The rapid urbanisation of populations in the tropics has increased the risk of transmitting respiratory pathogens. A combination of poverty and overcrowding in the peri- urban zones of rapidly expanding tropical cities promotes the epidemic spread of acute respiratory infection. PART A. INFECTIONS OF THE LOWER RESPIRATORY TRACT 9.2 PNEUMONIA 9.2.1 Frequency Over four million people die from acute respiratory infection per annum, mostly in developing countries. There is considerable overlap between these respiratory deaths and deaths due to tuberculosis, the single commonest fatal infection. The frequency of acute respiratory infection differs with location due to host, pathogen and environmental factors. Detailed figures are difficult to find and often need to be interpreted carefully, even for tuberculosis where data collection is more consistent. But in urban settings the enormity of respiratory infection is clearly evident. Up to half the patients attending hospital outpatient departments in developing countries have an acute respiratory infection. -

NIOSH), Centers for Disease Control and Prevention (CDC)
Technical Report Filtering Facepiece Respirators with an Exhalation Valve: Measurements of Filtration Efficiency to Evaluate Their Potential for Source Control Centers for Disease Control and Prevention National Institute for Occupational Safety and Health Technical Report Filtering Facepiece Respirators with an Exhalation Valve: Measurements of Filtration Efficiency to Evaluate Their Potential for Source Control DEPARTMENT OF HEALTH AND HUMAN SERVICES Centers for Disease Control and Prevention National Institute for Occupational Safety and Health National Personal Protective Technology Laboratory This document is in the public domain and may be freely copied or reprinted. Disclaimer Mention of any company or product does not constitute endorsement by the National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention (CDC). In addition, citations to websites external to NIOSH do not constitute NIOSH endorsement of the sponsoring organizations or their programs or products. Furthermore, NIOSH is not responsible for the content of these websites. All web addresses referenced in this document were accessible as of the publication date. Get More Information Find NIOSH products and get answers to workplace safety and health questions: 1-800-CDC-INFO (1-800-232-4636) | TTY: 1-888-232-6348 CDC/NIOSH INFO: cdc.gov/info | cdc.gov/niosh Monthly NIOSH eNews: cdc.gov/niosh/eNews Suggested Citation NIOSH [2020]. Filtering facepiece respirators with an exhalation valve: measurements of filtration efficiency to evaluate their potential for source control. By Portnoff L, Schall J, Brannen J, Suhon N, Strickland K, Meyers J. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. -

Physical and Geometric Constraints Shape the Labyrinth-Like Nasal Cavity
Physical and geometric constraints shape the labyrinth-like nasal cavity David Zwickera,b,1, Rodolfo Ostilla-Monico´ a,b, Daniel E. Liebermanc, and Michael P. Brennera,b aJohn A. Paulson School of Engineering and Applied Sciences, Harvard University, Cambridge, MA 02138; bKavli Institute for Bionano Science and Technology, Harvard University, Cambridge, MA 02138; and cDepartment of Human Evolutionary Biology, Harvard University, Cambridge, MA 02138 Edited by Leslie Greengard, New York University, New York, NY, and approved January 26, 2018 (received for review August 29, 2017) The nasal cavity is a vital component of the respiratory system take into account geometric constraints imposed by the shape that heats and humidifies inhaled air in all vertebrates. Despite of the head that determine the length of the nasal cavity, its this common function, the shapes of nasal cavities vary widely cross-sectional area, and, generally, the shape of the space that it across animals. To understand this variability, we here connect occupies. To tackle this complex problem, we first show that, nasal geometry to its function by theoretically studying the air- without geometric constraints, optimal shapes have slender flow and the associated scalar exchange that describes heating cross-sections. We then demonstrate that these shapes can be and humidification. We find that optimal geometries, which have compacted into the typical labyrinth-like shapes without much minimal resistance for a given exchange efficiency, have a con- loss in performance. stant gap width between their side walls, while their overall shape can adhere to the geometric constraints imposed by the Results head. Our theory explains the geometric variations of natural The Flow in the Nasal Cavity Is Laminar. -

Dynamic Mechanics of the Lung Answer to the Last Class’S Question
Dynamic mechanics of the lung Answer to the Last class’s question Resistive (Frictional Forces) Opposing Lung Inflation Frictional opposition occurs only when the system is in motion. Frictional opposition to ventilation has the two components: 1. tissue viscous resistance 2. airway resistance. Tissue Viscous Resistance: the impedance of motion (opposition to flow) caused by displacement of tissues during ventilation that includes the lungs, rib cage, diaphragm, and abdominal organs. The frictional resistance is generated by the movement of each organ surface sliding against the other (e.g., the lung lobes sliding against each other and against the chest wall). Tissue resistance accounts for only approximately 20% of the total resistance to lung inflation. In conditions : obesity, pleural fibrosis, and ascites, the tissue viscous resistance increases the total impedance to ventilation. Airway Resistance (flow resistance) - Resistance to ventilation by the movement of gas through the airways. • accounts for approximately 80% of the frictional resistance to ventilation. • -is usually expressed in units of cm H2O/L/sec: R= ∆P/ ∆V • Airway resistance in healthy adults ranges from approximately 0.5 to 2.5 cm H2O/L/sec. • To cause gas to flow into or out of the lungs at 1 L/sec, a healthy person needs to lower his alveolar pressure 0.5 to 2.5 cm H2O below atmospheric pressure. Measurement of Airway Resistance • Airway resistance is the pressure difference between the alveoli and the mouth divided by a flow rate. Mouth pressure is easily measured with a manometer. Alveolar pressure can be deduced from measurements made in a body plethysmograph.