Application of a Novel Osteotomy Instrumentation As a Substitute Tool in Total Hip Arthroplasty
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Metalwork & Woodwork Saws
HAMMERS - ANVILS - METALWORK & WOODWORK SAWS C HAMMERS BENCH PIN & ANVIL 77 CABLE TACKER GUN 76 DAVID USE PHOTO COPING SAWS 79 SD0010 FRETSAW BLADES 79 FRETSAW FRAMES 79 O HAMMER S & MALLETS 72 - 74 HACKSAWS 76 - 77 MINITURE ANVILS 74 MINITURE PINS 75 MALLET MITRE BOXES 82 PIERCING SAW BLADES 78 PIERCING SAW FRAMES 78 N DAVID USE PHOTO PIN PUSHERS 75 SD0010 RAZOR SAWS 81 SAW BLADE LUBRICANT 78 SAW KNIFE BLADES 81 STAPLE GUNS 75 - 76 V-BLOCK & CLAMPS 77 WEB STRETCHER 82 T ANVILS WOOD SAWS 80 - 81 X-ACTO RAZOR SAWS 81 DAVID USE PHOTO ZONA RAZOR SAWS 79 SD0010 E SAWS N DAVID USE PHOTO SD0010 T V BLOCK & CLAMP DAVID USE PHOTO SD0010 S Last Revised 04/07/2011 71 SQUIRES MODEL & CRAFT TOOLS HAMMERS & MALLETS MAGNETIC TACK HAMMER 6oz a specially designed hammer having one striking face magnetised for use when fitting small nails JEWELLERS MALLET a lightweight stainless steel mallet similar and upholstery tacks. The head features a claw for removing to those used by watchmakers and jewellers, with a solid head and tacks, the striking surface is a magnetic split pattern. The head is knurled shaft. hardened and pol- Length 145mm. ished. Fitted on a Weight 2½oz. hickory handle. Weight 6oz, length overall CODE TYPE PRICE 265mm. HA0025 Jewellers Mallet.................................................... £3.99 WATCHMAKERS MALLET a lightweight jewellers and watch- CODE TYPE PRICE makers mallet with a solid brass head. The handle is 260mm long 051-006 Magnetic Tack Hammer 6oz................................. £14.99 and has an increased diameter and is knurled for extra grip. -

A Woodworker's Wish List
A Woodworker’s Wish List Brighten the holidays with these great gifts By Joe Hurst-Wajszczuk Having a woodworker on and accessories we wish your gift list is both a blessing we had bought sooner. The and a curse. While there is result is a selection suitable no shortage of new tools for woodworkers of all skill and accessories, the trick is levels. So if you’ve got family selecting items that will get members or friends who are used, rather than sit on a shelf. woodworkers, skip the ties, For inspiration, we collected socks, scarves, and cologne. Give gift-giving advice from fellow some gifts that keep on giving, woodworkers and added our now and for years to come. own insights about the tools Photos: Larry Hamel-Lambert Dec/Jan 2016 woodcraftmagazine.com 43 Marking & Measuring Go to the Buyer’s Guide on p. 66 for prices and ordering informati on for featured items. Super-stable square $40 Compared to a combinati on square, the Veritas Sliding Square’s 3"-wide blade provides a more substanti al reference face for transferring measurements. With the collar removed, the accurately machined blade is also useful as a fl at square. Tighter tolerances $42 The Wixey Dual Display Caliper Make your mark $15 simultaneously displays decimal The name’s a curve ball, but the and fracti onal measurements benefi ts go straight to the heart (to the nearest 64th of an of precise layout. The Pica-Dry inch). Adding a WoodRiver Pen is a mechanical pencil that Depth Gauge ($20) turns works on most surfaces, including any caliper into a super- wet wood, glass, and ti le. -

LED-Reading Lamp Metal
111.264 LED-Reading lamp Metal Necessary tools: Metal drills ø2,5/3/4/6 mm Thread Tap M3mm 90°-Countersink Fretsaw with blade for metal File assortment Vice with jaw protectors Pencil Ruler Soldering iron Screwdriver Please Note The OPITEC range of projects is not primarily inten- ded as toys for young young children. It is for teaching, designing and making to ensure that puplis experience a range of tools and processes PARTS LIST Stückzahl Size (mm) Description Teile-Nr. Aluminium sheet 1 150x80x1 Housing 1 Aluminium rectangle 1 75x20x10 Housing 2 USB-LED-Lamp 1 Lighting 3 Micro slide switch 1 19x6 Switch 4 Alumnium wire 1 250x1,6 Clip 5 Machine screw 8 10x3 Lamp fixing 6 Machine screw 1 16x3 Lamp fixing 7 Nuts 2 M3 Switch fixing 8 Washers 6 M3 Fixing 9 Clips 1 3-7 Lamp fixing 10 Battery clip 1 Connection 11 Widerstand 220 Ohm 1 Vorwiderstand 12 D111264#1 1 INSTRUCTIONS General: For cutting the aluminium sheet use a fretsaw with a metal cutting blade 1. Cut the Aluminium-sheet (1) to the pattern (Page 3 ) with a fretsaw. Round the edges with a file and drill the holes ø3 + ø4 as shown in the pattern . Make the slot for the switch. To do this drill this make 3mm dia holes and then use a fretsaw File and clean up the edges, use a countersink to clean up any burr on the Top Bottom holes Note: For better drilling results, frstly bend the top and the bottom and then drill the 4mm dia holes togeher 2. -

The Carousel for Precision Grinding Wheels Mitsubishi Electric Europe B.V
The smart magazine for users Profile Issue 01 · October 2013 35 The carousel for precision grinding wheels Mitsubishi Electric Europe B.V. 38 Slashing machining time by 20 hours Eric Huyghe Formenbau 50 Almond crescents launch bespoke machine building Bott GmbH Contents Contents Contents 50 Almond crescents launch bespoke machine building 60 Moving up into the world league The flavour of success Injection moulds with up to 96 components Bott GmbH ERMO GROUP 56 Uncharted territory Exploring materials right at the machine Empa 06 We are all members of the Möderer family 30 Getting it right first time 75 years, 34 employees and a simple explanation Leaving nothing to chance Hans Möderer Werkzeug- & Formenbau GmbH Walter Pottiez GmbH 12 Intelligent clamping makes all the difference 35 The carousel for precision grinding wheels The key to success lies in good preparation Micrometre precision for the dressing of grinding wheels Aldrovandi AG Mitsubishi Electric Europe B.V. 18 Rust protection with water 38 Slashing machining time by 20 hours 04 Editorial 43 Profile magazine Banishing the risk of rust From 50 to 30 thanks to the MV2400R You’ve missed one of our issues? No problem! Chia-mo Srl Eric Huyghe Formenbau 05 Newsflash 65 Origami 24 Cutting diamonds with precision 44 Tooth for tooth – geared for success The art of mechanics and material Solutions for high-performance machining A Top 100 SME reports Lütticke GmbH Neugart GmbH 11 Competition 66 User horoscope 02 Profile 08.2013 Profile 08.2013 03 Editorial Latest developments HANS-JÜRGEN PELZERS Newsflash Editorial Only walking on air is better … Rapid relief for flood victims LED screens so large they can be measured Any customer who manages to cut machining time for a tool from 50 hours to in wingspans 30 will be walking on air (page 36). -

Hand & Power Tools
Hand & Power Tools Abrasives & Files 139 Hammers 140 Other Hand Tools 144 Clamps & Vices 141 Heat Guns 147 Plastic Forming 148 Cutters, Strippers & Pliers 136 Knives & Scalpels 138 Power Saws 147 Drill Bits 146 Lathes & Routers 147 Sanders 147 Drills & Drivers 146 Measuring Tools 142 Saws 140 Electronics Tool Kits 137 Miniature Power Tools 144 Screwdrivers 138 Full range of Hand & Power Tools available at: www.rapidonline.com 136 Hand & Power Tools Cutters, Strippers & Pliers Redline 110mm Mini Diagonal Side Wire Stripping Pliers Cutter with PVC Dipped Handles An economical plier- style wire stripper. This mini diagonal side cutter from Draper is • Drop forged ideal for use with cables • Fully polished micro and wires, and has been plating finish Electronics Side Cutters – Fine Point manufactured using • Heavy duty design Economy electronic hardened and tempered • Comfortable soft grip miniature side cutters carbon steel. Designed • Length: 150mm offering excellent value with cushion-grip PVC • Rolson type 21024 for money. Large contract dipped handles for comfortable use, plus captive double Type Order code 1+ purchases placed with leaf springs. Stripping pliers 86-0367 3.38 manufacturers enable us • Length: 110mm 178175 to offer these tools at a Red handles fraction of their normal cost elsewhere. • • Manufacturer’s part 68309 • Narrow blades for fine work in confined areas • Lap jointed Type Order code 1+ PVC handles Diagonal side cutter 91-7247 1.49 Automatic Wire Stripper • 560861 • Return spring An automatic, metal- • Overall length 125mm bodied wire stripper. Type Order code 1+ 10+ 20+ 40+ • Automatically 125mm fine cutters 85-0210 3.00 2.74 2.48 2.37 adjusts to size 060415 Tin Snips of wire Straight cut tin snips • Simple squeeze with hardened steel action Education blades and drop- • Powder-coated forged handles. -

Quick Start Book Contents
quick start book contents GETTING STARTED WITH DREMEL 3 MULTITOOL SYSTEM 4 MULTITOOL INFORMATION 5 MULTITOOL DIAGRAM 8 MULTITOOL ACCESSORIES 10 MULTITOOL ACCESSORIES INDEX 18 MULTITOOL ACCESSORY SETS 20 MULTITOOL ATTACHMENTS 21 OTHER TOOLS 26 HINTS AND TIPS 30 HOBBY LINE 33 PROJECTS 35 PROJECTS - OUTDOOR 36 PROJECTS - INDOOR 38 PROJECTS - CRAFTS & GIFTS 42 INDEX BY NUMBERS 46 2 GETTING STARTED WITH DREMEL® The Dremel ® Quick Start Book has been written to help you become familiar with the Dremel System of tools, accessories and attachments. The Quick Start Book will show you how to start using the tool in the right way by providing helpful information on the items typically packed with the tool. Next to that we will show inspiring projects. Beginners and experts alike will appreciate the “Projects section” which gives detailed instruction on projects that you can do with your Dremel. It includes indoor, outdoor and creative projects and will show how to improve and maintain your home and garden, as well as gift and craft projects. Go ahead and read this book. You will discover the world of Dremel: there is truly no limit to the amount of projects you can do with Dremel products. 3 MULTITOOL SYSTEM As the inventor of one of the most valued tools in the world, Dremel has worked hard to increase the value of its tool by making attachments and accessories that will easily adjust and vary its function. The Dremel high speed multitool is an entire system of functional options that centre around a core tool. This system makes the tool multi-functional, versatile and easy to use. -

Download the User Manual Here
safety 1 When you start working with tools, it’s important to make sure you do so in a safe manner. And always under supervision of an adult! 1 work area 1. Keep your work area clean and tidy. Make sure you have enough light, so you can see what you’re doing. 2. Make sure you work on a firm surface. The table you use should have a good height, so that you can work in a good position. tools 1. Tools are not toys. Use them carefully, so that you don’t injure yourself. Use them only for the purpose for which they were intended. 2. Always read first how a tool is supposed to be used, and always take note of the yellow triangles: Ask for help if you need it. Often not everything goes precisely as you’d like it to right away. That’s completely normal. The more often you’ve used a tool, the better you’ll be able to use it. © EDGE 2009 -1- 1 safety By observing certain safety measures, you can help ensure that nothing goes wrong What can you yourself do? When you start working with your tools, make 1. sure you’re calm, so that you can concentrate properly. 2. Think in advance about what tools you’ll be needing and how you’re going to start. 3. Put on clothes that won’t get in your way – ones without parts that hang loosely, such as long wide sleeves or the cord of a hood. If you have long hair put it in a ponytail. -

Tuke Saw™ System
Tuke Saw™ System Operating Manual Safe Navigation Through Soft Tissue Contents Section 1 | Introduction 3 Section 2 | Special features 4 Contents Section 3 | Operation 5 Section 4 | Use of blades and brushes 9 Section 5 | Care and maintenance 12 Section 6 | Tuke Saw™ and accessories 13 Section 7 | Tuke Saw™ blades and brushes 14 © MatOrtho Limited 2016. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording or any information storage and retrieval system. 2 | Tuke Saw™ System | Operating Manual Section 1 | 1 Introduction The Tuke Saw™ air-powered hand unit drives the blade or brush through a circular motion at frequencies of up to 20,000 cycles per minute. The circular motion of only 1.5mm vibrates soft tissues without cutting them. Introduction This safety feature allows the surgeon to guide the blade accurately by hand to delicate locations normally inaccessible to conventional power tools, or where saws are not normally used; for example, the posterior tibia cortex in TKR, or highly controlled mortice cutting for ankle replacement or arthrodesis. During resection the unique tooth-shape along with the circular motion promotes bone chip removal, making the cutting action clean and efficient. Blades with teeth on all sides will advance to penetrate a cut on the tip or on either side. The Tuke Saw™ System features the range of blades and brushes illustrated on page 14 of this brochure. These single-use attachments make the system extremely versatile especially in the field of orthopaedic surgery where shaping and shaving are often required. -

Cut Curves and Speed up Your Dovetails with This Simple Saw
TOOL TEST Coping Saws Cut curves and speed up your dovetails with this simple saw BY CHRIS GOCHNOUR VERSATILITY IN A SMALL PACKAGE With a coping saw, you can quickly get rid of the waste between dovetails (above). The saw’s narrow blade also makes it a great tool for cutting curves, like those on a bracket foot (right). And then there’s the job it’s named for, coping moldings, which it does better than any other tool (far right). 58 FINE WOODWORKING Photos: Matt Kenney COPYRIGHT 2011 by The Taunton Press, Inc. Copying and distribution of this article is not permitted. oping saws can be used to re- What to look for in a saw move waste in joinery, make Ccope cuts on molding, and EASY BLADE INSTALLATION saw tight curves of all kinds. Motor- With most saws, flex ized bandsaws and scrollsaws perform the frame to install the similar tasks, but require the workpiece blade. The blade has a to be brought to the tool, a task that pin on each end. The pins can be difficult, awkward, or even fit into sockets on the impossible. More often than not it’s frame (right), and prevent more convenient to take the tool to the it from slipping during workpiece. This makes the coping saw use. To install the blade, put the pin in the outside an indispensable tool in the woodshop, socket, then push down serving an essential and useful function on the handle to engage that cannot be matched by machine the pin in the inside tools. -
Practical Woodworking Presentation
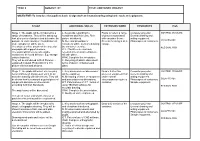
NATIONAL 4 AND 5 PRACTICAL WOODWORKING Resources in conjunction with Whitehill Secondary School NATIONAL 4 AND 5 PRACTICAL WOODWORKING COURSE AIMS • This course provides opportunities for you to gain a range of theoretical and practical woodworking skills relating to tools, equipment, processes and materials. You will also develop skills in reading and interpreting working drawings and related documents as well as an understanding of health and safety. • Through this, you will develop skills, knowledge and understanding of: • woodworking techniques • measuring and marking out timber sections and sheet materials • safe working practices in workshop environments • practical creativity and problem-solving skills • sustainability issues in a practical woodworking context READING DRAWINGS READING AND UNDERSTANDING DRAWINGS LEARNING INTENTIONS SUCCESS CRITERIA • To name the different types of drawing and their views • I can state the name of Some/Most/all of the various drawings • To understand scale • I can use scale to extract the correct dimensions from • To read, interpret and create cutting lists drawings • To understand the different line type found on drawings • I can extract information from cutting lists and create my • To read and extract information from working drawings: own linear, radial, angular and diametric dimensions • I can understand Some/Most/All of the different line type and know when and where they should be used • I can read and extract information from working drawings: linear, radial, angular and diametric dimensions • Working drawings are drawings used as a WORKING reference or guide in the manufacture of a product. This most often refers to engineering and architecture, DRAWINGS but working drawings are used in many different modes of construction. -
Container Project Objective
YEAR 8 SUBJECT: DT TITLE: CONTAINER PROJECT OBJECTIVE: To introduce the pupils to basic design work and manufacturing using basic tools and equipment. STAGE ADDITIONAL SKILLS EXTENSION WORK RESOURCES H&S Stage 1: The pupils will be introduced to a L. Keywords regarding the Pupils to collect a range Computer projector. CONTROL MEASURE range of containers. They will be asked top containers and their uses. Rich of pictures associated General drawing and look at a series of pictures and determine the picture introduced. with container theme. writing equipment. purpose of each container. No indication of N. Size and proportion of Present the images as a Photocopies of containers. CLEAPPS REF. scale / proportion will be given. containers will be mentioned during collage. The pictures will be shown on the projector the container exercise. RESIDUAL RISK and pupils will suggest answers. ICT. If facilities are available, The pupils will list every conceivable research into unusual containers container to be found at home. E.g. storage will take place. units to batteries. HWK. Complete the rich picture. They will be introduced to Rich Pictures - C. Recycling of plastic discussed I explained in detail. Production of a rich terms of plastic containers and picture with text and pictures. glass. Stage 2: The pupils will select six everyday L. Key words such as ‘dimensions’ Draw a further two Computer projector. CONTROL MEASURE items (stationery) and present each as an will be explained. pieces of equipment that General drawing and accurate drawing with dimensions. They will N. Measuring of items of equipment under normal writing equipment. -

Einhell Fretsaw Instruction Manual
TC-SS 405 E D Originalbetriebsanleitung SK Originálny návod na obsluhu Dekupiersäge Lupienková píla GB Original operating instructions NL Originele handleiding Fretsaw Decoupeerzaag F Instructions d’origine E Manual de instrucciones original Scie de découpage Sierra de marquetería I Istruzioni per l’uso originali FIN Alkuperäiskäyttöohje Sega a svolgere Kuviosaha DK/ Original betjeningsvejledning SLO Originalna navodila za uporabo N Dekupørsav Dekupirna žaga S Original-bruksanvisning H Eredeti használati utasítás Kontursåg Levágó fěrész CZ Originální návod k obsluze RO Instrucţiuni de utilizare originale Vykružovací pila Ferăstrău pentru decupat 9 Art.-Nr.: 43.090.40 I.-Nr.: 21050 AAnl_TC_SS_405_E_SPK9.indbnl_TC_SS_405_E_SPK9.indb 1 228.07.20208.07.2020 009:26:069:26:06 1a 19 12 11 10 13 15 18 2 5 23 8 1b 2 1 24 22 9 10 16 21 - 2 - AAnl_TC_SS_405_E_SPK9.indbnl_TC_SS_405_E_SPK9.indb 2 228.07.20208.07.2020 009:26:089:26:08 3 14 4 19 20 20 9 18 7 17 11 4 6 23 2 3 5 6a 14 13 15 18 8 16 6b 15 6c 18 8 13 15 - 3 - AAnl_TC_SS_405_E_SPK9.indbnl_TC_SS_405_E_SPK9.indb 3 228.07.20208.07.2020 009:26:119:26:11 7 8 7 17 5 6 - 4 - AAnl_TC_SS_405_E_SPK9.indbnl_TC_SS_405_E_SPK9.indb 4 228.07.20208.07.2020 009:26:189:26:18 D Gefahr! - Zur Verringerung des Verletzungsrisikos Bedienungsanleitung lesen Vorsicht! Tragen Sie einen Gehörschutz. Die Einwirkung von Lärm kann Gehörverlust bewirken. Vorsicht! Tragen Sie eine Staubschutzmaske. Beim Bearbeiten von Holz und anderer Materialien kann gesundheitsschädlicher Staub entstehen. Asbesthaltiges Material darf nicht bearbeitet werden! Vorsicht! Tragen Sie eine Schutzbrille.