Recurrent Inversion with Concomitant Deletion and Insertion Events in The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Roles and Mechanisms of Kinesin-6 KIF20A in Spindle Organization During Cell Division T ⁎ Wen-Da Wu, Kai-Wei Yu, Ning Zhong, Yu Xiao, Zhen-Yu She
European Journal of Cell Biology 98 (2019) 74–80 Contents lists available at ScienceDirect European Journal of Cell Biology journal homepage: www.elsevier.com/locate/ejcb Review Roles and mechanisms of Kinesin-6 KIF20A in spindle organization during cell division T ⁎ Wen-Da Wu, Kai-Wei Yu, Ning Zhong, Yu Xiao, Zhen-Yu She Department of Cell Biology and Genetics/Center for Cell and Developmental Biology, The School of Basic Medical Sciences, Fujian Medical University, Fuzhou, Fujian 350108, China ARTICLE INFO ABSTRACT Keywords: Mitotic kinesin is crucial for spindle assembly and chromosome segregation in cell division. KIF20A/MKlp2, a Kinesin-6 member of kinesin-6 subfamily, plays important roles in the central spindle organization at anaphase and cy- KIF20A tokinesis. In this review, we briefly introduce the discovery and classification of kinesin-6 motors in model Microtubule organisms, and summarize the biochemical features and mechanics of KIF20A proteins. We emphasize the Anaphase complicated interactions of KIF20A with partner proteins, including MKlp1, Plk1 and Rab6. Particularly, we Spindle assembly highlight the regulation of Cdk1 and chromosomal passenger complex on kinesin-6 KIF20A at late stage of Mitosis mitosis. We summarized the multiple functions of KIF20A in central spindle assembly and the formation of cleavage furrow in both mitosis and meiosis. In addition, we conclude the expression patterns of KIF20A in tumorigenesis and its applications in tumor therapy. 1. Introduction kinesin superfamily proteins (Miki et al., 2005). Kinesin-6 subfamily is comprised of KIF20A (Lawrence et al., 2004), KIF20B (MPP1) Kinesin superfamily proteins (KIFs) are molecular motors that (Kamimoto et al., 2001; Matsumoto-Taniura et al., 1996; Westendorf mediate the transport of various cargos, including the newly synthe- et al., 1994) and MKlp1 (Lawrence et al., 2004; Nislow et al., 1990; sized protein complexes, vesicles and mRNAs along the microtubule Sellitto and Kuriyama, 1988). -

Not Just Another Scaffolding Protein Family: the Multifaceted Mpps
molecules Review Not Just Another Scaffolding Protein Family: The Multifaceted MPPs 1, 1, 1 Agnieszka Chytła y , Weronika Gajdzik-Nowak y , Paulina Olszewska , Agnieszka Biernatowska 1 , Aleksander F. Sikorski 2 and Aleksander Czogalla 1,* 1 Department of Cytobiochemistry, Faculty of Biotechnology, University of Wroclaw, 50-383 Wroclaw, Poland; [email protected] (A.C.); [email protected] (W.G.-N.); [email protected] (P.O.); [email protected] (A.B.) 2 Research and Development Center, Regional Specialist Hospital, Kamie´nskiego73a, 51-154 Wroclaw, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-71375-6356 These authors contribute equally. y Academic Editor: Luís M.S. Loura Received: 16 September 2020; Accepted: 20 October 2020; Published: 26 October 2020 Abstract: Membrane palmitoylated proteins (MPPs) are a subfamily of a larger group of multidomain proteins, namely, membrane-associated guanylate kinases (MAGUKs). The ubiquitous expression and multidomain structure of MPPs provide the ability to form diverse protein complexes at the cell membranes, which are involved in a wide range of cellular processes, including establishing the proper cell structure, polarity and cell adhesion. The formation of MPP-dependent complexes in various cell types seems to be based on similar principles, but involves members of different protein groups, such as 4.1-ezrin-radixin-moesin (FERM) domain-containing proteins, polarity proteins or other MAGUKs, showing their multifaceted nature. In this review, we discuss the function of the MPP family in the formation of multiple protein complexes. Notably, we depict their significant role for cell physiology, as the loss of interactions between proteins involved in the complex has a variety of negative consequences. -

Cholesterol Interaction with the MAGUK Protein Family Member, MPP1, Via CRAC and CRAC-Like Motifs: an in Silico Docking Analysis
RESEARCH ARTICLE Cholesterol Interaction with the MAGUK Protein Family Member, MPP1, via CRAC and CRAC-Like Motifs: An In Silico Docking Analysis Marcin A. Listowski1, Jacek Leluk2, Sebastian Kraszewski3, Aleksander F. Sikorski1,2* 1 Department of Cytobiochemistry, Faculty of Biotechnology, University of Wrocław, Wrocław, Poland, 2 Department of Molecular Biology, University of Zielona Góra, Zielona Góra, Poland, 3 Department of Biomedical Engineering, Wrocław University of Technology, Wrocław, Poland * [email protected] Abstract OPEN ACCESS Cholesterol is essential for the proper organization of the biological membrane. Therefore, predicting which proteins can bind cholesterol is important in understanding how proteins Citation: Listowski MA, Leluk J, Kraszewski S, participate in lateral membrane organization. In this study, a simple bioinformatics approach Sikorski AF (2015) Cholesterol Interaction with the MAGUK Protein Family Member, MPP1, via CRAC was used to establish whether MPP1, a member of the MAGUK protein family, is capable of and CRAC-Like Motifs: An In Silico Docking Analysis. binding cholesterol. Modelled and experimentally-validated fragment structures were mined PLoS ONE 10(7): e0133141. doi:10.1371/journal. from online resources and searched for CRAC and CRAC-like motifs. Several of these pone.0133141 motifs were found in the primary structure of MPP1, and these were structurally visualized Editor: Robert J Deschenes, College of Medicine, to see whether they localized to the protein surface. Since all of the CRAC and CRAC-like University of South Florida, UNITED STATES motifs were found at the surface of MPP1 domains, in silico docking experiments were per- Received: December 18, 2014 formed to assess the possibility of interaction between CRAC motifs and cholesterol. -

MPP1-Based Mechanism of Resting State Raft Organization in the Plasma Membrane. Is It a General Or Specialized Mechanism in Erythroid Cells?
FOLIA HISTOCHEMICA REVIEW ET CYTOBIOLOGICA Vol. 57, No. 2, 2019 pp. 43–55 MPP1-based mechanism of resting state raft organization in the plasma membrane. Is it a general or specialized mechanism in erythroid cells? Magdalena Trybus, Lukasz Niemiec, Agnieszka Biernatowska, Anita Hryniewicz-Jankowska, Aleksander F. Sikorski Department of Cytobiochemistry, Faculty of Biotechnology, University of Wroclaw Abstract Biological membranes are organized in various microdomains, one of the best known being called membrane rafts. The major function of these is thought to organize signaling partners into functional complexes. An im- portant protein found in membrane raft microdomains of erythroid and other blood cells is MPP1 (membrane palmitoylated protein 1)/p55. MPP1 (p55) belongs to the MAGUK (membrane-associated guanylate kinase homolog) family and it is a major target of palmitoylation in the red blood cells (RBCs) membrane. The well- known function of this protein is to participate in formation of the junctional complex of the erythrocyte mem- brane skeleton. However, its function as a “raft organizer” is not well understood. In this review we focus on recent reports concerning MPP1 participation in membrane rafts organization in erythroid cells, including its role in signal transduction. Currently it is not known whether MPP1 could have a similar role in cell types other than erythroid lineage. We present also preliminary data regarding the expression level of MPP1 gene in several non-erythroid cell lines. (Folia Histochemica et Cytobiologica 2019, Vol. 57, No. 2, 43–55) Key words: membrane palmitoylated protein 1 (MPP1); resting state rafts; lateral membrane organization; raft-associated proteins Introduction maintaining erythrocyte membrane mechanical properties plays membrane skeleton, whose structure The red cell membrane comprises a lipid bilayer and function have been a subject of many studies and with integral membrane proteins embedded in it and reviews [1–3]. -

Anti-MPP1 Antibody (ARG58994)
Product datasheet [email protected] ARG58994 Package: 100 μl anti-MPP1 antibody Store at: -20°C Summary Product Description Rabbit Polyclonal antibody recognizes MPP1 Tested Reactivity Hu Tested Application FACS, IHC-P Host Rabbit Clonality Polyclonal Isotype IgG Target Name MPP1 Antigen Species Human Immunogen KLH-conjugated synthetic peptide corresponding to aa. 301-327 of Human MPP1. Conjugation Un-conjugated Alternate Names AAG12; PEMP; DXS552E; EMP55; Membrane protein, palmitoylated 1; p55; MRG1; 55 kDa erythrocyte membrane protein Application Instructions Application table Application Dilution FACS 1:10 - 1:50 IHC-P 1:50 - 1:100 Application Note * The dilutions indicate recommended starting dilutions and the optimal dilutions or concentrations should be determined by the scientist. Calculated Mw 52 kDa Properties Form Liquid Purification Purification with Protein A and immunogen peptide. Buffer PBS and 0.09% (W/V) Sodium azide. Preservative 0.09% (W/V) Sodium azide Storage instruction For continuous use, store undiluted antibody at 2-8°C for up to a week. For long-term storage, aliquot and store at -20°C or below. Storage in frost free freezers is not recommended. Avoid repeated freeze/thaw cycles. Suggest spin the vial prior to opening. The antibody solution should be gently mixed before use. Note For laboratory research only, not for drug, diagnostic or other use. www.arigobio.com 1/2 Bioinformation Gene Symbol MPP1 Gene Full Name membrane protein, palmitoylated 1, 55kDa Background This gene encodes the prototype of the membrane-associated guanylate kinase (MAGUK) family proteins. MAGUKs interact with the cytoskeleton and regulate cell proliferation, signaling pathways, and intercellular junctions. -

393LN V 393P 344SQ V 393P Probe Set Entrez Gene
393LN v 393P 344SQ v 393P Entrez fold fold probe set Gene Gene Symbol Gene cluster Gene Title p-value change p-value change chemokine (C-C motif) ligand 21b /// chemokine (C-C motif) ligand 21a /// chemokine (C-C motif) ligand 21c 1419426_s_at 18829 /// Ccl21b /// Ccl2 1 - up 393 LN only (leucine) 0.0047 9.199837 0.45212 6.847887 nuclear factor of activated T-cells, cytoplasmic, calcineurin- 1447085_s_at 18018 Nfatc1 1 - up 393 LN only dependent 1 0.009048 12.065 0.13718 4.81 RIKEN cDNA 1453647_at 78668 9530059J11Rik1 - up 393 LN only 9530059J11 gene 0.002208 5.482897 0.27642 3.45171 transient receptor potential cation channel, subfamily 1457164_at 277328 Trpa1 1 - up 393 LN only A, member 1 0.000111 9.180344 0.01771 3.048114 regulating synaptic membrane 1422809_at 116838 Rims2 1 - up 393 LN only exocytosis 2 0.001891 8.560424 0.13159 2.980501 glial cell line derived neurotrophic factor family receptor alpha 1433716_x_at 14586 Gfra2 1 - up 393 LN only 2 0.006868 30.88736 0.01066 2.811211 1446936_at --- --- 1 - up 393 LN only --- 0.007695 6.373955 0.11733 2.480287 zinc finger protein 1438742_at 320683 Zfp629 1 - up 393 LN only 629 0.002644 5.231855 0.38124 2.377016 phospholipase A2, 1426019_at 18786 Plaa 1 - up 393 LN only activating protein 0.008657 6.2364 0.12336 2.262117 1445314_at 14009 Etv1 1 - up 393 LN only ets variant gene 1 0.007224 3.643646 0.36434 2.01989 ciliary rootlet coiled- 1427338_at 230872 Crocc 1 - up 393 LN only coil, rootletin 0.002482 7.783242 0.49977 1.794171 expressed sequence 1436585_at 99463 BB182297 1 - up 393 -

Erythrocyte Scaffolding Protein P55/MPP1 Functions As an Essential Regulator of Neutrophil Polarity
Erythrocyte scaffolding protein p55/MPP1 functions as an essential regulator of neutrophil polarity Brendan J. Quinna, Emily J. Welcha, Anthony C. Kima, Mary A. Lokutab,1, Anna Huttenlocherb, Anwar A. Khana, Shafi M. Kuchaya, and Athar H. Chishtia,2 aDepartment of Pharmacology, University of Illinois College of Medicine, Chicago, IL 60612; and bDepartments of Pediatrics and Pharmacology, University of Wisconsin, Madison, WI 53706 Edited by Henry R. Bourne, University of California, San Francisco, CA, and approved September 16, 2009 (received for review June 23, 2009) As mediators of innate immunity, neutrophils respond to chemoat- p85/p110 in immunoprecipitates (7). Neutrophils treated with tractants by adopting a highly polarized morphology. Efficient che- the PI3K␥ inhibitors PIK-90 or -93, which inhibit the production motaxis requires the formation of one prominent pseudopod at the of PIP3, respond to chemoattractants by forming multiple pseu- cell front characterized by actin polymerization, while local inhibition dopods, whereas neutrophils treated with the class IA PI3K suppresses the formation of rear and lateral protrusions. This asym- inhibitors polarize normally (3). Furthermore, neutrophils from metric control of signaling pathways is required for directional mi- p110␥ knockout mice exhibit both defective chemotaxis in vitro gration along a chemotactic gradient. Here, we identify the MAGUK and reduced accumulation in the peritoneal cavity in response to protein p55/MPP1 as a mediator of the frontness signal required for inflammatory stimuli in vivo (8–11). This evidence indicates that neutrophil polarization. We developed a p55 knockout (p55؊/؊) stimulation of PI3K␥ causes a rapid increase in the accumulation ؊/؊ mouse model, and demonstrate that p55 neutrophils form multi- of PIP3, which in turn drives pseudopod formation, thus main- ple transient pseudopods upon chemotactic stimulation, and do not taining neutrophil polarity. -

Erythrocyte Scaffolding Protein P55/MPP1 Functions As an Essential Regulator of Neutrophil Polarity
Erythrocyte scaffolding protein p55/MPP1 functions as an essential regulator of neutrophil polarity Brendan J. Quinna, Emily J. Welcha, Anthony C. Kima, Mary A. Lokutab,1, Anna Huttenlocherb, Anwar A. Khana, Shafi M. Kuchaya, and Athar H. Chishtia,2 aDepartment of Pharmacology, University of Illinois College of Medicine, Chicago, IL 60612; and bDepartments of Pediatrics and Pharmacology, University of Wisconsin, Madison, WI 53706 Edited by Henry R. Bourne, University of California, San Francisco, CA, and approved September 16, 2009 (received for review June 23, 2009) As mediators of innate immunity, neutrophils respond to chemoat- p85/p110 in immunoprecipitates (7). Neutrophils treated with tractants by adopting a highly polarized morphology. Efficient che- the PI3K␥ inhibitors PIK-90 or -93, which inhibit the production motaxis requires the formation of one prominent pseudopod at the of PIP3, respond to chemoattractants by forming multiple pseu- cell front characterized by actin polymerization, while local inhibition dopods, whereas neutrophils treated with the class IA PI3K suppresses the formation of rear and lateral protrusions. This asym- inhibitors polarize normally (3). Furthermore, neutrophils from metric control of signaling pathways is required for directional mi- p110␥ knockout mice exhibit both defective chemotaxis in vitro gration along a chemotactic gradient. Here, we identify the MAGUK and reduced accumulation in the peritoneal cavity in response to protein p55/MPP1 as a mediator of the frontness signal required for inflammatory stimuli in vivo (8–11). This evidence indicates that neutrophil polarization. We developed a p55 knockout (p55؊/؊) stimulation of PI3K␥ causes a rapid increase in the accumulation ؊/؊ mouse model, and demonstrate that p55 neutrophils form multi- of PIP3, which in turn drives pseudopod formation, thus main- ple transient pseudopods upon chemotactic stimulation, and do not taining neutrophil polarity. -

Structures of the Human Pals1 PDZ Domain with and Without Ligand Suggest Gated Access of Crb to the PDZ Peptide-Binding Groove ISSN 1399-0047
research papers Structures of the human Pals1 PDZ domain with and without ligand suggest gated access of Crb to the PDZ peptide-binding groove ISSN 1399-0047 Marina E. Ivanova,a Georgina C. Fletcher,b Nicola O’Reilly,c Andrew G. Purkiss,a Barry J. Thompsonb and Neil Q. McDonalda,d* Received 9 October 2014 aStructural Biology Laboratories, Cancer Research UK, 44 Lincoln’s Inn Fields, London WC2A 3LY, England, bEpithelial Accepted 19 December 2014 Biology Laboratories, Cancer Research UK, 44 Lincoln’s Inn Fields, London WC2A 3LY, England, cPeptide Chemistry Laboratories, Cancer Research UK, 44 Lincoln’s Inn Fields, London WC2A 3LY, England, and dInstitute of Structural and Molecular Biology, Department of Biological Sciences, Birkbeck College, University of London, Malet Street, London WC1E 7HX, England. *Correspondence e-mail: [email protected] Keywords: PDZ domains; Crb; cell polarity; epithelia; stardust. Many components of epithelial polarity protein complexes possess PDZ PDB references: PDZ–peptide complex, 4uu5; domains that are required for protein interaction and recruitment to the apical ligand-free PDZ domain, 4uu6 plasma membrane. Apical localization of the Crumbs (Crb) transmembrane protein requires a PDZ-mediated interaction with Pals1 (protein-associated Supporting information: this article has with Lin7, Stardust, MPP5), a member of the p55 family of membrane- supporting information at journals.iucr.org/d associated guanylate kinases (MAGUKs). This study describes the molecular interaction between the Crb carboxy-terminal motif (ERLI), which is required for Drosophila cell polarity, and the Pals1 PDZ domain using crystallography and fluorescence polarization. Only the last four Crb residues contribute to Pals1 PDZ-domain binding affinity, with specificity contributed by conserved charged interactions. -
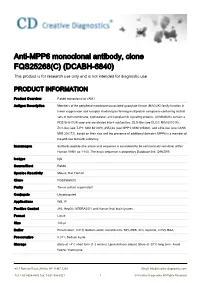
Anti-MPP6 Monoclonal Antibody, Clone FQS25268(C) (DCABH-6840) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-MPP6 monoclonal antibody, clone FQS25268(C) (DCABH-6840) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Rabbit monoclonal to VAM1 Antigen Description Members of the peripheral membrane-associated guanylate kinase (MAGUK) family function in tumor suppression and receptor clustering by forming multiprotein complexes containing distinct sets of transmembrane, cytoskeletal, and cytoplasmic signaling proteins. All MAGUKs contain a PDZ-SH3-GUK core and are divided into 4 subfamilies, DLG-like (see DLG1; MIM 601014), ZO1-like (see TJP1; MIM 601009), p55-like (see MPP1; MIM 305360), and LIN2-like (see CASK; MIM 300172), based on their size and the presence of additional domains. MPP6 is a member of the p55-like MAGUK subfamily Immunogen Synthetic peptide (the amino acid sequence is considered to be commercially sensitive) within Human VAM1 aa 1-100. The exact sequence is proprietary.Database link: Q9NZW5 Isotype IgG Source/Host Rabbit Species Reactivity Mouse, Rat, Human Clone FQS25268(C) Purity Tissue culture supernatant Conjugate Unconjugated Applications WB, IP Positive Control 293, HepG2, NTERA2/D1 and Human fetal brain lysates. Format Liquid Size 100 μl Buffer Preservative: 0.01% Sodium azide; Constituents: 59% PBS, 40% Glycerol, 0.05% BSA Preservative 0.01% Sodium Azide Storage Store at +4°C short term (1-2 weeks). Upon delivery aliquot. Store at -20°C long term. Avoid freeze / thaw cycle. 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Ship Shipped at 4°C. -
Integrated Functional Genomic Analyses of Klinefelter and Turner Syndromes Reveal Global Network Effects of Altered X Chromosome Dosage
Integrated functional genomic analyses of Klinefelter and Turner syndromes reveal global network effects of altered X chromosome dosage Xianglong Zhanga,b,1, David Honga,1,2, Shining Mac,d,1, Thomas Warda,b, Marcus Hoa,b, Reenal Pattnia,b, Zhana Durenc,d, Atanas Stankova, Sharon Bade Shresthaa, Joachim Hallmayera, Wing Hung Wongc,d,2, Allan L. Reissa,2, and Alexander E. Urbana,b,2 aDepartment of Psychiatry and Behavioral Sciences, Stanford University School of Medicine, Stanford, CA 94305; bDepartment of Genetics, Stanford University School of Medicine, Stanford, CA 94305; cDepartment of Statistics, Stanford University, Stanford, CA 94305; and dDepartment of Biomedical Data Science, Stanford University, Stanford, CA 94305 Contributed by Wing Hung Wong, January 16, 2020 (sent for review June 20, 2019; reviewed by Carolyn J. Brown and Joseph F. Cubells) In both Turner syndrome (TS) and Klinefelter syndrome (KS) copy with short stature in TS (4) and tall stature in KS (5). X-chromosome number aberrations of the X chromosome lead to various develop- inactivation (XCI) transcriptionally silences one X chromosome mental symptoms. We report a comparative analysis of TS vs. KS in female mammals; as such, most genes on the inactivated X regarding differences at the genomic network level measured in chromosome are silenced and inactive (hereinafter referred to as primary samples by analyzing gene expression, DNA methylation, inactive genes). However, some genes escape XCI (hereinafter and chromatin conformation. X-chromosome inactivation (XCI) referred to as escape genes) and have also been hypothesized to silences transcription from one X chromosome in female mammals, contribute to the phenotypes of SCAs (6, 7). -
Structure and Function of the Guanylate Kinase-Like Domain of the MAGUK Family Scaffold Proteins
Front. Biol. 2012, 7(5): 379–396 DOI 10.1007/s11515-012-1244-9 REVIEW Structure and function of the guanylate kinase-like domain of the MAGUK family scaffold proteins Jinwei ZHU1, Yuan SHANG1, Jia CHEN1, Mingjie ZHANG (✉)1,2 1 Division of Life Science, State Key Laboratory of Molecular Neuroscience, Hong Kong University of Science and Technology, Clear Water Bay, Kowloon, Hong Kong, China 2 Institute for Advanced Study, Hong Kong University of Science and Technology, Clear Water Bay, Kowloon, Hong Kong, China © Higher Education Press and Springer-Verlag Berlin Heidelberg 2012 Abstract Membrane associated guanylate kinases (MAGUKs) are a family of scaffold proteins that play essential roles in organ development, cell-cell communication, cell polarity establishment and maintenance, and cellular signal transduction. Every member of the MAGUK family contains a guanylate kinase-like (GK) domain, which has evolved from the enzyme catalyzing GMP to GDP conversion to become a protein–protein interaction module with no enzymatic activity. Mutations of MAGUKs are linked to a number of human diseases, including autism and hereditary deafness. In this review, we summarize the structural basis governing cellular function of various members of the MAGUKs. In particular, we focus on recent discoveries of MAGUK GKs as specific phospho-protein interaction modules, and discuss functional implications and connections to human diseases of such regulated MAGUK GK/target interactions. Keywords MAGUK, GK domain, phospho-protein interaction module, synapse, neuronal disease Introduction 2004; Funke et al., 2005; Zheng et al., 2011; Oliva et al., 2012); Zonula Occludens (ZO) subfamily proteins act as Membrane-associated guanylate kinases (MAGUKs) origin- molecular linkers between tight junction proteins and actin ally referred to a family of scaffold proteins highly cytoskeletons (González-Mariscal et al., 2000); calcium/ concentrated at the sites of cell-cell junctions (Woods and calmodulin-dependent protein kinase (CASK) mainly loca- Bryant, 1993; Anderson, 1996; Funke et al., 2005).