Cockerham Blackwell Companion to Mediacal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
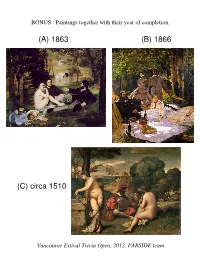
1866 (C) Circa 1510 (A) 1863
BONUS : Paintings together with their year of completion. (A) 1863 (B) 1866 (C) circa 1510 Vancouver Estival Trivia Open, 2012, FARSIDE team BONUS : Federal cabinet ministers, 1940 to 1990 (A) (B) (C) (D) Norman Rogers James Ralston Ernest Lapointe Joseph-Enoil Michaud James Ralston Mackenzie King James Ilsley Louis St. Laurent 1940s Andrew McNaughton 1940s Douglas Abbott Louis St. Laurent James Ilsley Louis St. Laurent Brooke Claxton Douglas Abbott Lester Pearson Stuart Garson 1950s 1950s Ralph Campney Walter Harris John Diefenbaker George Pearkes Sidney Smith Davie Fulton Donald Fleming Douglas Harkness Howard Green Donald Fleming George Nowlan Gordon Churchill Lionel Chevrier Guy Favreau Walter Gordon 1960s Paul Hellyer 1960s Paul Martin Lucien Cardin Mitchell Sharp Pierre Trudeau Leo Cadieux John Turner Edgar Benson Donald Macdonald Mitchell Sharp Edgar Benson Otto Lang John Turner James Richardson 1970s Allan MacEachen 1970s Ron Basford Donald Macdonald Don Jamieson Barney Danson Otto Lang Jean Chretien Allan McKinnon Flora MacDonald JacquesMarc Lalonde Flynn John Crosbie Gilles Lamontagne Mark MacGuigan Jean Chretien Allan MacEachen JeanJacques Blais Allan MacEachen Mark MacGuigan Marc Lalonde Robert Coates Jean Chretien Donald Johnston 1980s Erik Nielsen John Crosbie 1980s Perrin Beatty Joe Clark Ray Hnatyshyn Michael Wilson Bill McKnight Doug Lewis BONUS : Name these plays by Oscar Wilde, for 10 points each. You have 30 seconds. (A) THE PAGE OF HERODIAS: Look at the moon! How strange the moon seems! She is like a woman rising from a tomb. She is like a dead woman. You would fancy she was looking for dead things. THE YOUNG SYRIAN: She has a strange look. -

PERIOD 1 (CHONG): Trial of the Pms Schedule June 2006
Trials of the PMs Schedule Date Trial CHARGE Prosecution Prosecution Defence Defence Witnesses Judge PM Name Witnesses Mon Jan 10 Robert Decision to institute the Wartime Abdullah Karen (Wilfrid Laurier) Naeem Sukhpreet (Nelly Victor Mr. N Borden Elections Act McClung) Causing division by forcing Samuel Byron (Henri Bourassa) Krunal Garry (Sir Sam Hughes) conscription on the country Internment of Enemy Aliens Brandon Justin (Stefan Galant) Kayne Edward L.(William Otter) Tues Jan 11 Mackenzie Racial Discrimination in turning Peter Brianna (Captain Gustav Edward L. Kayne (Frederick Blair) Abdullah Samuel King away the SS St. Louis Schroeder) Ineffective leadership in the Byron Luxman (James Ralston) Sherry Nelson (Andrew policy of Conscription in WWII McNaughton) Unjust Internment of Japanese Garry Krunal (David Suzuki) Sharon Jason (John Hart) Canadians Wed Jan 12 John Unjustified in cancelling the Nelson Edward F. (Crawford Justin Brandon (General Guy Jayna Mr. N. Diefenbaker Avro Arrow Gordon Jr.) Simonds) Failure to act decisively during Mihai Kayne (John F. Kennedy) Jason Sharon (Howard Green) Cuban Missile Crisis Failed to secure Canada by not Mihai Sherry (Douglass Luxman Victor (Howard Green) arming Bomarc Missiles with Harkness) nuclear warheads Thurs Jan 13 Pierre Unjustified invoking of the War Stefani Sherry (Tommy Douglas) Victor Luxman (Robert Brianna Mr. N. Trudeau Measures Act in October Crisis Bourassa) Ineffective policy of the 1980 Keara Kayne (Peter Lougheed) Edward F. Abdullah (Marc Lalonde) National Energy Program Failure to get Quebec to sign the Jayna Byron (Rene Levesque) Maggie Jenise (Bill Davis) Constitution Act in 1982 Fri Jan 14 Brian Weakened Canada’s economy Brianna Jayna (Paul Martin) Annie Stefani (Michael Wilson) Kayne Mr. -

Un Plan De Developpement Pour La Gaspesie Et Le Bas-Saint-Laurent
ol. 4, numero 5, mai 1983 MON1-3011 C S 4404 - PECH UN PLAN DE DEVELOPPEMENT POUR LA GASPESIE ET LE BAS-SAINT-LAURENT Le gouvernement canadien a annonce au debut de mai un programme special de developpement de la Gaspesie et du Bas-Saint-Laurent de 224,5 millions $, repartis sur 5 ans, dont 71 millions $ pour le secteur des peches. Cette annonce a ete faite a Matane devant les organismes regionaux par les ministres Pierre De Bane, Marc Lalonde et Herb Gray, accom- pagnes des deputes de la region. AU SOMMAIRE D'autres ameliorations au havre de Matane 7 224,5 millions $ pour la region du Un centre de recherche a Mont-Joli 8 Bas-Saint-Laurent/Gaspesie 2 71 millions $ pour le developpement Un nouveau havre de !Ache a Cap-Chat 9 des 'Aches en Gaspesie 3 Six nouveaux projets de developpement La formation en p8che: un choix de carrieres 10 4 dans le comte de Gaspe Lancement de la phase II du programme PERIO : ants travaux a Gascons, federal de developpement economique SH defroi et Bonaventure 6 des Iles-de-la-Madeleine 12 223 E57 224,5 MILLIONS $ POUR LA REGION DU BAS-SAINT-LAURENT/GASPESIE Le gouvernement canadien a initiatives issues du milieu ainsi Un connite executif regroupant les annonce au debut de mai un pro- que les frais d'administration du differents ministeres sera tree sous gramme special de developpement Plan. la presidence du coordonnateur de la Gaspesie et du Bas-Saint- federal du developpement econo- Le gouvernement favorisera les Laurent de 224,5 millions $ repartis mique pour le Quebec, M. -

Trudeau, Constitutionalism, and Family Allowances Raymond Blake
Document generated on 09/26/2021 5:01 p.m. Journal of the Canadian Historical Association Revue de la Société historique du Canada Intergovernmental Relations Trumps Social Policy Change: Trudeau, Constitutionalism, and Family Allowances Raymond Blake Volume 18, Number 1, 2007 Article abstract Family allowances were one of the few programs shared by all Canadian URI: https://id.erudit.org/iderudit/018260ar families from 1945 to 1992, and one of the few means of building social DOI: https://doi.org/10.7202/018260ar cohesion across Canada. Family allowances became embroiled in the minefield of Canadian intergovernmental relations and the political crisis created by the See table of contents growing demands from Quebec for greater autonomy from the federal government in the early 1970s. Ottawa initially dismissed Quebec’s demands for control over social programs generally and family allowance in particular. Publisher(s) However, Prime Minister Pierre Trudeau offered family allowance reforms as a means of enticing Quebec Premier Robert Bourassa to amend the British The Canadian Historical Association/La Société historique du Canada North America Act. The government’s priority was constitutional reform, and it used social policy as a bargaining chip to achieve its policy objectives in that ISSN area. This study shows that public policy decisions made with regard to the family allowance program were not motivated by the pressing desire to make 0847-4478 (print) more effective policies for children and families. 1712-6274 (digital) Explore this journal Cite this article Blake, R. (2007). Intergovernmental Relations Trumps Social Policy Change: Trudeau, Constitutionalism, and Family Allowances. Journal of the Canadian Historical Association / Revue de la Société historique du Canada, 18(1), 207–239. -

The Mulroney-Schreiber Affair - Our Case for a Full Public Inquiry
HOUSE OF COMMONS CANADA THE MULRONEY-SCHREIBER AFFAIR - OUR CASE FOR A FULL PUBLIC INQUIRY Report of the Standing Committee on Access to Information, Privacy and Ethics Paul Szabo, MP Chair APRIL, 2008 39th PARLIAMENT, 2nd SESSION The Speaker of the House hereby grants permission to reproduce this document, in whole or in part for use in schools and for other purposes such as private study, research, criticism, review or newspaper summary. Any commercial or other use or reproduction of this publication requires the express prior written authorization of the Speaker of the House of Commons. If this document contains excerpts or the full text of briefs presented to the Committee, permission to reproduce these briefs, in whole or in part, must be obtained from their authors. Also available on the Parliamentary Internet Parlementaire: http://www.parl.gc.ca Available from Communication Canada — Publishing, Ottawa, Canada K1A 0S9 THE MULRONEY-SCHREIBER AFFAIR - OUR CASE FOR A FULL PUBLIC INQUIRY Report of the Standing Committee on Access to Information, Privacy and Ethics Paul Szabo, MP Chair APRIL, 2008 39th PARLIAMENT, 2nd SESSION STANDING COMMITTEE ON ACCESS TO INFORMATION, PRIVACY AND ETHICS Paul Szabo Pat Martin Chair David Tilson Liberal Vice-Chair Vice-Chair New Democratic Conservative Dean Del Mastro Sukh Dhaliwal Russ Hiebert Conservative Liberal Conservative Hon. Charles Hubbard Carole Lavallée Richard Nadeau Liberal Bloc québécois Bloc québécois Glen Douglas Pearson David Van Kesteren Mike Wallace Liberal Conservative Conservative iii OTHER MEMBERS OF PARLIAMENT WHO PARTICIPATED Bill Casey John Maloney Joe Comartin Hon. Diane Marleau Patricia Davidson Alexa McDonough Hon. Ken Dryden Serge Ménard Hon. -

A New Perspective on Public Health
This is Public Health: A Canadian History A New Perspective on Public Health A New Perspective on Public Health . .8 .1 After .22 .years .of .expansion .in .Canada’s .health . services, .the .1970s .began .with .a .period .of . Environmental Concerns . 8 .3 consolidation, .rationalization .and .reduced . federal .funding .for .health .care . .Industrialized . Motor Vehicle Safety . 8 .4 countries .began .to .recognize .that .the .substantial . Physical Activity . 8 .4 declines .in .mortality .achieved .over .the .last .100 . years .were .largely .due .to .improvements .in .living . People with Disabilities . 8 .6 standards .rather .than .medical .advancements . This .brought .a .rethinking .of .health .systems . Chronic Disease . .8 .7 in .the .1970s .and .1980s, .initiating .a .period . A Stronger Stand . .8 .7 of .Canadian .innovation .and .leadership .in . new .approaches .to .health .promotion .with .an . The Lalonde Report . 8 .8 impact .both .at .home .and .abroad . .Concerns . about .the .environment, .chronic .diseases, .and . Expanding Interests . 8 .10 the .heavy .toll .of .motor .vehicle .collisions .were . growing, .as .were .new .marketing .approaches .to . Tobacco . 8 .12 deliver .the .“ounce .of .prevention” .message .to . Infectious Diseases . 8 .14 the .public . .Researchers .developed .systematic . methodologies .to .reduce .risk .factors .and .applied . A New Strain of Swine Flu . 8 .16 an .epidemiological .approach .to .health .promotion . by .defining .goals .and .specific .objectives .1 Sexually Transmitted Infections (STIs) . 8 .17 At .the .beginning .of .the .1970s, .federal .and . Global Issues . 8 .19 provincial .governments .were still. .analyzing .the . Primary Health Care— 348 .recommendations of. .the .two-year .National . Task .Force .on .the .Cost .of .Health .Services, . Health for All by 2000 . -

The Rise and Fall of the Widely Held Firm: a History of Corporate Ownership in Canada
This PDF is a selection from a published volume from the National Bureau of Economic Research Volume Title: A History of Corporate Governance around the World: Family Business Groups to Professional Managers Volume Author/Editor: Randall K. Morck, editor Volume Publisher: University of Chicago Press Volume ISBN: 0-226-53680-7 Volume URL: http://www.nber.org/books/morc05-1 Conference Date: June 21-22, 2003 Publication Date: November 2005 Title: The Rise and Fall of the Widely Held Firm: A History of Corporate Ownership in Canada Author: Randall Morck, Michael Percy, Gloria Tian, Bernard Yeung URL: http://www.nber.org/chapters/c10268 1 The Rise and Fall of the Widely Held Firm A History of Corporate Ownership in Canada Randall K. Morck, Michael Percy, Gloria Y. Tian, and Bernard Yeung 1.1 Introduction At the beginning of the twentieth century, large pyramidal corporate groups, controlled by wealthy families or individuals, dominated Canada’s large corporate sector, as in modern continental European countries. Over several decades, a large stock market, high taxes on inherited income, a sound institutional environment, and capital account openness accompa- nied the rise of widely held firms. At mid-century, the Canadian large cor- porate sector was primarily freestanding widely held firms, as in the mod- ern large corporate sectors of the United States and United Kingdom. Then, in the last third of the century, a series of institutional changes took place. These included a more bank-based financial system, a sharp abate- Randall K. Morck is Stephen A. Jarislowsky Distinguished Professor of Finance at the University of Alberta School of Business and a research associate of the National Bureau of Economic Research. -

Printable List of Laureates
Laureates of the Canadian Medical Hall of Fame A E Maude Abbott MD* (1994) Connie J. Eaves PhD (2019) Albert Aguayo MD(2011) John Evans MD* (2000) Oswald Avery MD (2004) F B Ray Farquharson MD* (1998) Elizabeth Bagshaw MD* (2007) Hon. Sylvia Fedoruk MA* (2009) Sir Frederick Banting MD* (1994) William Feindel MD PhD* (2003) Henry Barnett MD* (1995) B. Brett Finlay PhD (2018) Murray Barr MD* (1998) C. Miller Fisher MD* (1998) Charles Beer PhD* (1997) James FitzGerald MD PhD* (2004) Bernard Belleau PhD* (2000) Claude Fortier MD* (1998) Philip B. Berger MD (2018) Terry Fox* (2012) Michel G. Bergeron MD (2017) Armand Frappier MD* (2012) Alan Bernstein PhD (2015) Clarke Fraser MD PhD* (2012) Charles H. Best MD PhD* (1994) Henry Friesen MD (2001) Norman Bethune MD* (1998) John Bienenstock MD (2011) G Wilfred G. Bigelow MD* (1997) William Gallie MD* (2001) Michael Bliss PhD* (2016) Jacques Genest MD* (1994) Roberta Bondar MD PhD (1998) Gustave Gingras MD* (1998) John Bradley MD* (2001) Phil Gold MD PhD (2010) Henri Breault MD* (1997) Richard G. Goldbloom MD (2017) G. Malcolm Brown PhD* (2000) Jean Gray MD (2020) John Symonds Lyon Browne MD PhD* (1994) Wilfred Grenfell MD* (1997) Alan Burton PhD* (2010) Gordon Guyatt MD (2016) C H G. Brock Chisholm MD (2019) Vladimir Hachinski MD (2018) Harvey Max Chochnov, MD PhD (2020) Antoine Hakim MD PhD (2013) Bruce Chown MD* (1995) Justice Emmett Hall* (2017) Michel Chrétien MD (2017) Judith G. Hall MD (2015) William A. Cochrane MD* (2010) Michael R. Hayden MD PhD (2017) May Cohen MD (2016) Donald O. -

The Health of Canadians – the Federal Role Volume One – the Story So Far
The Standing Senate Committee on Social Affairs, Science and Technology Interim Report on the state of health care system in Canada The Health of Canadians – The Federal Role Volume One – The Story So Far Chair The Honourable Michael J. L. Kirby Deputy Chair The Honourable Marjory LeBreton MARCH 2001 TABLE OF CONTENTS ORDER OF REFERENCE............................................................................................iii MEMBERSHIP.................................................................................................................iv FOREWORD......................................................................................................................v INTRODUCTION............................................................................................................1 CHAPTER ONE: ............................................................................................................. 5 Historical Background on Public Health Care Insurance and the Role of the Federal Government in Financing Health Care ............................................................................. 5 1.1 Federal Role in Health and Health Care..................................................................... 5 1.2 Cost-Sharing Arrangements ...................................................................................... 7 1.3 Functioning of the EPF Block Funding..................................................................... 11 1.4 The CHST......................................................................................................... -

The Liberal Third Option
The Liberal Third Option: A Study of Policy Development A Thesis Submitted to the Faculty of Graduate Studies and Research in Partial Fuliiment of the Requirements for the Degree of Master of Arts in Political Science University of Regina by Guy Marsden Regina, Saskatchewan September, 1997 Copyright 1997: G. W. Marsden 395 Wellington Street 395, rue Wellington Ottawa ON KI A ON4 Ottawa ON KIA ON4 Canada Canada Your hie Votre rdtérence Our ME Notre référence The author has granted a non- L'auteur a accordé une licence non exclusive licence allowing the exclusive permettant à la National Library of Canada to Bibliothèque nationale du Canada de reproduce, loan, distibute or sell reproduire, prêter, distribuer ou copies of this thesis in microform, vendre des copies de cette thèse sous paper or electronic formats. la forme de microfiche/nlm, de reproduction sur papier ou sur format électronique. The author retains ownership of the L'auteur conserve la propriété du copyright in this thesis. Neither the droit d'auteur qui protège cette thèse. thesis nor substanîial extracts fiom it Ni la thèse ni des extraits substantiels may be printed or otherwise de celle-ci ne doivent être imprimés reproduced without the author's ou autrement reproduits sans son permission. autorisation. This study presents an analysis of the nationalist econornic policies enacted by the federal Liberal government during the 1970s and early 1980s. The Canada Development Corporation(CDC), the Foreign Investment Review Agency(FIRA), Petro- Canada(PetroCan) and the National Energy Prograrn(NEP), coliectively referred to as "The Third Option," aimed to reduce Canada's dependency on the United States. -

Paradigm Freeze Why It Is So Hard to Reform Health-Care Policy in Canada
Paradigm Freeze WHY IT IS SO HARD TO REFORM HEALTHCARE POLICY IN CANADA Edited by Harvey Lazar John N. Lavis, Pierre-Gerlier Forest, and John Church Institute of Intergovernmental Relations The Institute of Intergovernmental Relations The Institute is the only academic organization in Canada whose mandate is solely to pro- mote research and communication on the challenges facing the federal system. Current research interests include fiscal federalism, health policy, the reform of federal political institutions and the machinery of federal-provincial relations, Canadian federalism and the global economy, and comparative federalism. The Institute pursues these objectives through research conducted by its own associates and other scholars, through its publication program, and through seminars and conferences. The Institute links academics and practitioners of federalism in federal and provincial govern ments and the private sector. The Institute of Intergovernmental Relations receives ongoing financial support from the J.A. Corry Memorial Endowment Fund, the Royal Bank of Canada Endowment Fund, the Government of Canada, and the governments of Manitoba and Ontario. We are grateful for this support, which enables the Institute to sustain its program of research, publication, and related activities. L’Institut des relations intergouvernementales L’Institut est le seul organisme universitaire canadien à se consacrer exclusivement à la recherche et aux échanges sur les enjeux du fédéralisme. Les priorités de recherche de l’Institut portent présentement sur le fédéralisme fiscal, la santé, la modification des institutions politiques fédérales, les mécanismes des relations fédérales-provinciales, le fédéralisme canadien dans l’économie mondiale et le fédéralisme comparatif. L’Institut réalise ses objectifs par le biais de recherches effectuées par ses chercheurs et par des chercheurs de l’Université Queen’s et d’ailleurs, de même que par des congrès et des colloques. -

Defined by Spirituality?" the Iddeh N Pierre Elliott Rt Udeau: the Aithf Behind the Politics
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Sacred Heart University: DigitalCommons@SHU Sacred Heart University DigitalCommons@SHU Mission and Catholic Identity Publications Office of Mission and Catholic Identity 2004 Defined yb Spirituality? Michael W. Higgins Sacred Heart University Follow this and additional works at: https://digitalcommons.sacredheart.edu/mission_pub Part of the Catholic Studies Commons, and the Political Science Commons Recommended Citation Higgins, Michael W. "Defined by Spirituality?" The iddeH n Pierre Elliott rT udeau: The aithF Behind the Politics. Ed. John English, Richard Gwyn, and P. Whitney Lackenbauer. Ottawa: Novalis, 2004. ISBN 9782895075509 This Book Chapter is brought to you for free and open access by the Office of Mission and Catholic Identity at DigitalCommons@SHU. It has been accepted for inclusion in Mission and Catholic Identity Publications by an authorized administrator of DigitalCommons@SHU. For more information, please contact [email protected], [email protected]. Defined by Spirituality? Michael W. Higgins Before we set out on our journey to discover something about the spiritual pilgrimage of Rerre Elliott Trudeau, it is helpful to set the context. In Canada, unlike the United States and the United Kingdom, we do not like to talk about religion and public life. It makes us uncomfortable. A perfect illustration of this unhappy truism can be seen in the^ recent portrait tl^at appeared in The Globe and Mail by Doug Saunders on the life and leadership of Prime Minister Tony Blair.' In this otheiwise informative and ipsightful piece on Prime Minister Blair, Mr.