Systemically Administered Central Nervous System Drugs Induced Ocular Side Effects: a Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

World Journal of Pharmaceutical Research Mathur Et Al
World Journal of Pharmaceutical Research Mathur et al . World Journal of Pharmaceutical SJIF ResearchImpact Factor 8.074 Volume 7, Issue 16, 111-124. Review Article ISSN 2277– 7105 ADRS DUE TO ANTIPSYCHOTIC DRUGS: A REVIEW Prashant Mathur*1 and Waseem Yahya2 1,2Department of Pharmacy Practice Shri Guru Ram Rai Institute of Technology and Science, Patel Nagar (248001), Dehradun, Uttarakhand. INTRODUCTION Article Received on 28 June 2018, WHO defines an ADR as ―any response to a drug which is noxious and Revised on 18 July 2018, unintended, and which occurs at doses normally used in man for Accepted on 08 August 2018, DOI: 10.20959/wjpr201816-12706 prophylaxis, diagnosis, or therapy of disease, or for the modification of physiological function‖.[1] The antipsychotic drugs are chemically *Corresponding Author diverse but have the common property of alleviating the symptoms of [2] Prashant Mathur organic as well as functional psychosis. Antipsychotics are among Department of Pharmacy the most effective drugs used in psychiatry in the maintenance therapy Practice Shri Guru Ram Rai of schizophrenia, mania, or in acute psychotic reactions.[3] These drugs Institute of Technology and are also capable of causing a wide range of potential adverse drug Science, Patel Nagar (248001), Dehradun, reactions that can lead to non-compliance that can impair quality of Uttarakhand. life, may cause stigma and physical morbidity which may lead to discontinuation of medication and in extreme cases may be fatal.[4] Antipsychotic drugs have a high therapeutic -

Properties and Units in Clinical Pharmacology and Toxicology
Pure Appl. Chem., Vol. 72, No. 3, pp. 479–552, 2000. © 2000 IUPAC INTERNATIONAL FEDERATION OF CLINICAL CHEMISTRY AND LABORATORY MEDICINE SCIENTIFIC DIVISION COMMITTEE ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)# and INTERNATIONAL UNION OF PURE AND APPLIED CHEMISTRY CHEMISTRY AND HUMAN HEALTH DIVISION CLINICAL CHEMISTRY SECTION COMMISSION ON NOMENCLATURE, PROPERTIES, AND UNITS (C-NPU)§ PROPERTIES AND UNITS IN THE CLINICAL LABORATORY SCIENCES PART XII. PROPERTIES AND UNITS IN CLINICAL PHARMACOLOGY AND TOXICOLOGY (Technical Report) (IFCC–IUPAC 1999) Prepared for publication by HENRIK OLESEN1, DAVID COWAN2, RAFAEL DE LA TORRE3 , IVAN BRUUNSHUUS1, MORTEN ROHDE1, and DESMOND KENNY4 1Office of Laboratory Informatics, Copenhagen University Hospital (Rigshospitalet), Copenhagen, Denmark; 2Drug Control Centre, London University, King’s College, London, UK; 3IMIM, Dr. Aiguader 80, Barcelona, Spain; 4Dept. of Clinical Biochemistry, Our Lady’s Hospital for Sick Children, Crumlin, Dublin 12, Ireland #§The combined Memberships of the Committee and the Commission (C-NPU) during the preparation of this report (1994–1996) were as follows: Chairman: H. Olesen (Denmark, 1989–1995); D. Kenny (Ireland, 1996); Members: X. Fuentes-Arderiu (Spain, 1991–1997); J. G. Hill (Canada, 1987–1997); D. Kenny (Ireland, 1994–1997); H. Olesen (Denmark, 1985–1995); P. L. Storring (UK, 1989–1995); P. Soares de Araujo (Brazil, 1994–1997); R. Dybkær (Denmark, 1996–1997); C. McDonald (USA, 1996–1997). Please forward comments to: H. Olesen, Office of Laboratory Informatics 76-6-1, Copenhagen University Hospital (Rigshospitalet), 9 Blegdamsvej, DK-2100 Copenhagen, Denmark. E-mail: [email protected] Republication or reproduction of this report or its storage and/or dissemination by electronic means is permitted without the need for formal IUPAC permission on condition that an acknowledgment, with full reference to the source, along with use of the copyright symbol ©, the name IUPAC, and the year of publication, are prominently visible. -

The Effects of Antipsychotic Treatment on Metabolic Function: a Systematic Review and Network Meta-Analysis
The effects of antipsychotic treatment on metabolic function: a systematic review and network meta-analysis Toby Pillinger, Robert McCutcheon, Luke Vano, Katherine Beck, Guy Hindley, Atheeshaan Arumuham, Yuya Mizuno, Sridhar Natesan, Orestis Efthimiou, Andrea Cipriani, Oliver Howes ****PROTOCOL**** Review questions 1. What is the magnitude of metabolic dysregulation (defined as alterations in fasting glucose, total cholesterol, low density lipoprotein (LDL) cholesterol, high density lipoprotein (HDL) cholesterol, and triglyceride levels) and alterations in body weight and body mass index associated with short-term (‘acute’) antipsychotic treatment in individuals with schizophrenia? 2. Does baseline physiology (e.g. body weight) and demographics (e.g. age) of patients predict magnitude of antipsychotic-associated metabolic dysregulation? 3. Are alterations in metabolic parameters over time associated with alterations in degree of psychopathology? 1 Searches We plan to search EMBASE, PsycINFO, and MEDLINE from inception using the following terms: 1 (Acepromazine or Acetophenazine or Amisulpride or Aripiprazole or Asenapine or Benperidol or Blonanserin or Bromperidol or Butaperazine or Carpipramine or Chlorproethazine or Chlorpromazine or Chlorprothixene or Clocapramine or Clopenthixol or Clopentixol or Clothiapine or Clotiapine or Clozapine or Cyamemazine or Cyamepromazine or Dixyrazine or Droperidol or Fluanisone or Flupehenazine or Flupenthixol or Flupentixol or Fluphenazine or Fluspirilen or Fluspirilene or Haloperidol or Iloperidone -

Maternal Use of Psychiatric Medications During Pregnancy And
MATERNAL USE OF PSYCHIATRIC MEDICATIONS DURING PREGNANCY AND ADVERSE BIRTH OUTCOMES AND NEURODEVELOPMENTAL PROBLEMS IN OFFSPRING Ayesha C. Sujan Submitted to the faculty of the University Graduate School in partial fulfillment of the requirements for the degree Doctor of Philosophy in the Department of Psychological and Brain Sciences, Indiana University July 2021 ii Accepted by the Graduate Faculty, Indiana University, in partial fulfillment of the requirements for the degree of Doctor of Philosophy. Doctoral Committee _______________________________________________ Brian M. D’Onofrio, PhD _______________________________________________ Richard Viken, PhD _______________________________________________ Patrick D. Quinn, PhD _______________________________________________ Christina Ludema, PhD _______________________________________________ A. Sara Oberg, PhD, MD April 22nd, 2020 iii © 2021 Ayesha C. Sujan iv Ayesha Sujan MATERNAL USE OF PSYCHIATRIC MEDICATIONS DURING PREGNANCY AND ADVERSE BIRTH OUTCOMES AND NEURODEVELOPMENTAL PROBLEMS IN OFFSPRING Understanding consequences of prenatal exposure to psychiatric and analgesic medications is important because use of these medications among pregnant women is relatively common and increasing. Rodent experiments have shown effects of perinatal exposure to specific medications; however, these findings might not apply to humans. Human observational studies have been used to study prenatal exposure to psychiatric and analgesic medications rather than randomiZed control trials due to ethical concerns -

Supranuclear and Internuclear Ocular Motility Disorders
CHAPTER 19 Supranuclear and Internuclear Ocular Motility Disorders David S. Zee and David Newman-Toker OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN OCULAR MOTOR SYNDROMES CAUSED BY LESIONS OF THE MEDULLA THE SUPERIOR COLLICULUS Wallenberg’s Syndrome (Lateral Medullary Infarction) OCULAR MOTOR SYNDROMES CAUSED BY LESIONS OF Syndrome of the Anterior Inferior Cerebellar Artery THE THALAMUS Skew Deviation and the Ocular Tilt Reaction OCULAR MOTOR ABNORMALITIES AND DISEASES OF THE OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN BASAL GANGLIA THE CEREBELLUM Parkinson’s Disease Location of Lesions and Their Manifestations Huntington’s Disease Etiologies Other Diseases of Basal Ganglia OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN THE PONS THE CEREBRAL HEMISPHERES Lesions of the Internuclear System: Internuclear Acute Lesions Ophthalmoplegia Persistent Deficits Caused by Large Unilateral Lesions Lesions of the Abducens Nucleus Focal Lesions Lesions of the Paramedian Pontine Reticular Formation Ocular Motor Apraxia Combined Unilateral Conjugate Gaze Palsy and Internuclear Abnormal Eye Movements and Dementia Ophthalmoplegia (One-and-a-Half Syndrome) Ocular Motor Manifestations of Seizures Slow Saccades from Pontine Lesions Eye Movements in Stupor and Coma Saccadic Oscillations from Pontine Lesions OCULAR MOTOR DYSFUNCTION AND MULTIPLE OCULAR MOTOR SYNDROMES CAUSED BY LESIONS IN SCLEROSIS THE MESENCEPHALON OCULAR MOTOR MANIFESTATIONS OF SOME METABOLIC Sites and Manifestations of Lesions DISORDERS Neurologic Disorders that Primarily Affect the Mesencephalon EFFECTS OF DRUGS ON EYE MOVEMENTS In this chapter, we survey clinicopathologic correlations proach, although we also discuss certain metabolic, infec- for supranuclear ocular motor disorders. The presentation tious, degenerative, and inflammatory diseases in which su- follows the schema of the 1999 text by Leigh and Zee (1), pranuclear and internuclear disorders of eye movements are and the material in this chapter is intended to complement prominent. -

When Taking Medication May Be a Sin: Dietary Requirements and Food Laws
BJPsych Advances (2015), vol. 21, 425–432 doi: 10.1192/apt.bp.114.012534 When taking medication may be a ARTICLE sin: dietary requirements and food laws in psychotropic prescribing Waqqas A. Khokhar, Simon L. Dein, Mohammed S. Qureshi, Imran Hameed, Mohammed M. Ali, Yasir Abbasi, Hasan Aman & Ruchit Sood In psychiatric practice, it is not uncommon to Waqqas A. Khokhar is a SUMMARY come across patients who refuse any psychiatric consultant psychiatrist with Leicestershire Partnership NHS Religious laws do not usually forbid the use of intervention, placing their faith in a spiritual psychotropic medication, but many do forbid the Trust and an honorary lecturer in recovery enabled by their religious beliefs (Campion the Centre for Ageing and Mental consumption of animal-based derivatives of bovine 1997; Koenig 2001). Although religious laws do Health at Staffordshire University. and/or porcine origin (e.g. gelatin and stearic not usually restrict the taking of psychotropic Simon L. Dein is a senior lecturer acid) such as are found in many medications. at University College London, an Demonstrating awareness of this, combined with medication, many do forbid consumption of the Honorary Clinical Professor at a genuine concern about how it affects the patient, animal derivatives, particularly gelatin and stearic the University of Durham and a may strengthen the doctor–patient relationship acid, that many psychotropics contain. This has consultant psychiatrist with the and avoid non-adherence. In this article, we major implications, for example, for patients who North Essex Partnership University NHS Foundation Trust. Mohammed outline dietary requirements of key religions and follow Judaism, Islam, Hinduism, Buddhism and S. -

Eye Movement Disorders and Neurological Symptoms in Late-Onset Inborn Errors of Metabolism Koens, Lisette H.; Tijssen, Marina A
University of Groningen Eye movement disorders and neurological symptoms in late-onset inborn errors of metabolism Koens, Lisette H.; Tijssen, Marina A. J.; Lange, Fiete; Wolffenbuttel, Bruce H. R.; Rufa, Alessandra; Zee, David S.; de Koning, Tom J. Published in: Movement Disorders DOI: 10.1002/mds.27484 IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2018 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Koens, L. H., Tijssen, M. A. J., Lange, F., Wolffenbuttel, B. H. R., Rufa, A., Zee, D. S., & de Koning, T. J. (2018). Eye movement disorders and neurological symptoms in late-onset inborn errors of metabolism. Movement Disorders, 33(12), 1844-1856. https://doi.org/10.1002/mds.27484 Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. -
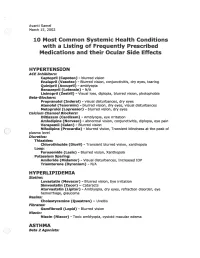
2002 Samel 10 Most Common Systemic Health Conditions with A
Avanti Samel / March 15, 2002 10 Most Common Systemic Health Conditions with a Listing of Frequently Prescribed Medications and their Ocular Side Effects HYPERTENSION ACE Inhibitors: Captopril (Capoten}- blurred vision Enalapril (Vasotec) - Blurred vision, conjunctivitis, dry eyes, tearing Quinipril (Accupril)- amblyopia Benazepril (Lotensin)- N/A Lisinopril (Zestril) - Visual loss, diplopia, blurred vision, photophobia Beta-Blockers: Propranolol (Inderal)- visual disturbances, dry eyes Atenolol (Tenormin)- blurred vision, dry eyes, visual disturbances Metoprolol (Lopressor) - blurred vision, dry eyes calcium Channel Blockers: Diltiazem (Cardizem)- Amblyopia, eye irritation Amlodipine (Norvasc)- abnormal vision, conjunctivitis, diplopia, eye pain Verapamil (Calan)- Blurred vision Nifedipine (Procardia) - blurred vision, Transient blindness at the peak of plasma level · Diuretics: Thiazides: Chlorothiazide (Diuril) - Transient blurred vision, xanthopsia Loop: Furosemide (Lasix) - Blurred vision, Xanthopsia Potassium Sparing: Amiloride (Midamor) - Visual disturbances, Increased lOP Triamterene (Dyrenium)- N/A HYPERLIPIDEMIA Statins: Lovastatin (Mevacor) - Blurred vision, Eye irritation Simvastatin (Zocor)- Cataracts Atorvastatin (Lipitor)- Amblyopia, dry eyes, refraction disorder, eye hemorrhage, glaucoma Resins: Cholestyramine (Questran)- Uveitis Fibrates: Gemfibrozil (Lopid)- Blurred vision Niacin: Niacin (Niacor) - Toxic amblyopia, cystoid macular edema ASTHMA ( ) Beta 2 Agonists: Albuterol (Proventil) - N/A ( Salmeterol (Serevent)- -

Neuro-Ophthalmologic Manifestations of Paraneoplastic Syndromes
STATE OF THE ART Neuro-Ophthalmologic Manifestations of Paraneoplastic Syndromes Melissa W. Ko, MD, Josep Dalmau, MD, PhD, and Steven L. Galetta, MD Abstract: Paraneoplastic syndromes with neuro- PARANEOPLASTIC CEREBELLAR ophthalmologic manifestations may involve the cen DEGENERATION tral nervous system, cranial nerves, neuromuscular Paraneoplastic cerebellar degeneration (PCD) is junction, optic nerve, uvea, or retina. Most of these a syndrome of subacute severe pancerebellar dysfunction disorders are related to immunologic mechanisms (Table 1). Initially, patients present with gait instability. presumably triggered by the neoplastic expression of Over several days to weeks, they develop truncal and limb neuronal proteins. Accurate recognition is essential to ataxia, dysarthria, and dysphagia. The cerebellar disease appropriate management. eventually stabilizes but leaves patients incapacitated. PCD is most commonly associated with cancers of (/Neuro-Ophthalmol 2008;28:58-68) the lung, ovary, and breast and with Hodgkin disease (7). Ocular motor manifestations include nystagmus, ocular dysmetria, saccadic pursuit, saccadic intrusions and he term "paraneoplastic neurologic syndrome" (PNS) oscillations, and skew deviation (8). Over the last 30 refers to dysfunction of the nervous system caused by T years, at least nine anti-neuronal antibodies have been a benign or malignant tumor via mechanisms other than associated with PCD. However, only about 50% of patients metastasis, coagulopathy, infection, or treatment side with suspected PCD test positive for anti-neuronal anti effects (1). Whereas reports of possible paraneoplastic bodies in serum or cerebrospinal fluid (CSF) (9). Anti-Yo neuropathies extend back to the 19th century, cerebellar syndromes associated with cancer were first described by and anti-Tr are the autoantibodies most commonly Brouwerin 1919 (2). -
GAZE and AUTONOMIC INNERVATION DISORDERS Eye64 (1)
GAZE AND AUTONOMIC INNERVATION DISORDERS Eye64 (1) Gaze and Autonomic Innervation Disorders Last updated: May 9, 2019 PUPILLARY SYNDROMES ......................................................................................................................... 1 ANISOCORIA .......................................................................................................................................... 1 Benign / Non-neurologic Anisocoria ............................................................................................... 1 Ocular Parasympathetic Syndrome, Preganglionic .......................................................................... 1 Ocular Parasympathetic Syndrome, Postganglionic ........................................................................ 2 Horner Syndrome ............................................................................................................................. 2 Etiology of Horner syndrome ................................................................................................ 2 Localizing Tests .................................................................................................................... 2 Diagnosis ............................................................................................................................... 3 Flow diagram for workup of anisocoria ........................................................................................... 3 LIGHT-NEAR DISSOCIATION ................................................................................................................. -

Psychotropic Drugs and Ocular Side Effects Psikotropik İlaçlar Ve Oküler Yan Etkileri
DOI: 10.4274/tjo.43.67944 Review / Derleme Psychotropic Drugs and Ocular Side Effects Psikotropik İlaçlar ve Oküler Yan Etkileri İpek Sönmez, Ümit Aykan* Near East University, Department of Psychiatry, Nicosia, TRNC, MD *Near East University, Department of Ophthalmology, Nicosia, TRNC Sum mary Nowadays the number of patients using the types of drugs in question here has significantly increased. A study carried out in relation with the long term use of psychotropic drugs shows that the consumption of this group of drugs has substantially increased in terms of variety and quantity. This compilation is arranged in accordance with the ocular complications of psychotropic drugs in long term treatment profile of numerous patients to the results of related literature review. If the doctor and the patients are informed about the eye problems related to the use of psychotropic drugs, potential ocular complications can be easily prevented, supervised and controlled and can even be reversed. (Turk J Ophthalmol 2013; 43: 270-7) Key Words: Psychotropic drugs, ocular, side effects, adverse effects Özet Günümüzde kronik ilaç kullanan hasta sayısı önemli derecede artmıştır. Uzun süreli psikotrop ilaç kullanımı açısından yapılan bir çalışma, hem çeşitlilik hem de miktar açısından bu grup ilaç tüketiminin önemli derecede arttığını göstermektedir. Bu derleme günümüzde çok sayıda hastanın uzun süreli tedavi profilinde yer alan psikotrop ilaçların oküler komplikasyonlarına ilişkin literatür taraması sonucu hazırlanmıştır. Hekim ve hastalar psikotrop ilaç kullanımına bağlı göz problemleri açısından bilgili oldukları takdirde potansiyel oküler komplikasyonlar kolayca önlenebilir, gözlem ve kontrol altına alınabilir ve hatta geriye döndürülebilirler. (Turk J Ophthalmol 2013; 43: 270-7) Anah tar Ke li me ler: Psikotropik ilaç, oküler, yan etki, ters etki Introduction human eye becoming sensitive to psychotropic treatments. -

Yo U Are P Ro H Ib Ited from M Aking Th Is P D F P U B Licly Availab Le. It Is
Focus on Women’s Mental Health It is illegal to post this copyrighted PDF on any website. CME Background Depression and Anxiety Articles are selected for credit designation based on an assessment of the educational needs of CME in the Postpartum Period participants, with the purpose of providing readers with a curriculum of CME articles on a variety of and Risk of Bipolar Disorder: topics throughout each volume. Activities are planned using a process that links identified needs A Danish Nationwide with desired results. Register-Based Cohort Study To obtain credit, read the article, correctly answer the questions in the Posttest, and complete the Xiaoqin Liu, PhDa,*; Esben Agerbo, DrMedSca,b,c; Evaluation. A $5 processing fee will apply. Jiong Li, PhDd; Samantha Meltzer-Brody, MPHe; Veerle Bergink, PhDa,f,‡; and Trine Munk-Olsen, PhDa,‡ CME Objective After studying this article, you should be able to: • Screen patients with postpartum depressive ABSTRACT symptoms for bipolarity Objective: The first-onset affective episode requiring inpatient treatment in the postpartum period can be a marker of bipolar disorder, but it is Accreditation Statement unknown whether milder postpartum affective episodes are also indicators of underlying bipolarity. Therefore, we aimed to study whether women with a The CME Institute of Physicians nonpsychotic postpartum affective episode treated with antidepressants have Postgraduate Press, Inc., is an increased risk of bipolar disorder. accredited by the Accreditation Council for Continuing Medical Methods: A register-based cohort study was conducted in Denmark of Education to provide continuing 122,622 parous women without psychiatric history who received a first-time medical education for physicians.