ECG Manifestations: the Poisoned Patient Christopher P
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Interactions of Some Commonly Used Drugs in Dermatology
Table Drug interactions of some commonly used drugs in dermatology M. J. Cyriac Department of Dermatology and Venereology, Medical College, Kottayam, India. Address for correspondence: Dr. M. J. Cyriac, Professor and Head, Department of Dermatology and Venereology, Medical College, Kottayam, India. E-mail: [email protected] Drug interactions leading to serious adverse effects are alternative medicines or food should also be borne in to be cautiously watched for when multiple drugs are mind.2 Increased risk of drug induced toxicity or used simultaneously.1 It is important for the physician therapeutic failure can occur when a new drug is added to be aware of these interactions. Although in many to a treatment regimen. It is impossible to remember instances the adverse interaction does not reach a all possible drug interactions. A ready to refer checklist magnitude of recognizable clinical expression, rarely is useful as a handy reference. it can result in a serious adverse outcome. Some of the commonly used drugs in dermatology and Adverse drug interactions may lead to increased their interactions, resultant clinical effect and possible toxicity, decreased efficacy or both. The possibility of underlying mechanisms are given in Table 1. Table 2 lists interaction with non-prescription drugs, herbal or the drugs with their relative risk for inducing interactions. Table 1: Drug interactions of some commonly used drugs Drug Interacting drug Adverse effect Remarks Erythromycin/Clarithromycin Theophylline Theophylline toxicity Precipitates -

The Pharmacology of Amiodarone and Digoxin As Antiarrhythmic Agents
Part I Anaesthesia Refresher Course – 2017 University of Cape Town The Pharmacology of Amiodarone and Digoxin as Antiarrhythmic Agents Dr Adri Vorster UCT Department of Anaesthesia & Perioperative Medicine The heart contains pacemaker, conduction and contractile tissue. Cardiac arrhythmias are caused by either enhancement or depression of cardiac action potential generation by pacemaker cells, or by abnormal conduction of the action potential. The pharmacological treatment of arrhythmias aims to achieve restoration of a normal rhythm and rate. The resting membrane potential of myocytes is around -90 mV, with the inside of the membrane more negative than the outside. The main extracellular ions are Na+ and Cl−, with K+ the main intracellular ion. The cardiac action potential involves a change in voltage across the cell membrane of myocytes, caused by movement of charged ions across the membrane. This voltage change is triggered by pacemaker cells. The action potential is divided into 5 phases (figure 1). Phase 0: Rapid depolarisation Duration < 2ms Threshold potential must be reached (-70 mV) for propagation to occur Rapid positive charge achieved as a result of increased Na+ conductance through voltage-gated Na+ channels in the cell membrane Phase 1: Partial repolarisation Closure of Na+ channels K+ channels open and close, resulting in brief outflow of K+ and a more negative membrane potential Phase 2: Plateau Duration up to 150 ms Absolute refractory period – prevents further depolarisation and myocardial tetany Result of Ca++ influx -

Dabigatran Amoxicillin Clavulanate IV Treatment in the Community
BEST PRACTICE 38 SEPTEMBER 2011 Dabigatran Amoxicillin clavulanate bpac nz IV treatment in the community better medicin e Editor-in-chief We would like to acknowledge the following people for Professor Murray Tilyard their guidance and expertise in developing this edition: Professor Carl Burgess, Wellington Editor Dr Gerry Devlin, Hamilton Rebecca Harris Dr John Fink, Christchurch Dr Lisa Houghton, Dunedin Programme Development Dr Rosemary Ikram, Christchurch Mark Caswell Dr Sisira Jayathissa, Wellington Rachael Clarke Kate Laidlow, Rotorua Peter Ellison Dr Hywel Lloyd, GP Reviewer, Dunedin Julie Knight Associate Professor Stewart Mann, Wellington Noni Richards Dr Richard Medlicott, Wellington Dr AnneMarie Tangney Dr Alan Panting, Nelson Dr Sharyn Willis Dr Helen Patterson, Dunedin Dave Woods David Rankin, Wellington Report Development Dr Ralph Stewart, Auckland Justine Broadley Dr Neil Whittaker, GP Reviewer, Nelson Tim Powell Dr Howard Wilson, Akaroa Design Michael Crawford Best Practice Journal (BPJ) ISSN 1177-5645 Web BPJ, Issue 38, September 2011 Gordon Smith BPJ is published and owned by bpacnz Ltd Management and Administration Level 8, 10 George Street, Dunedin, New Zealand. Jaala Baldwin Bpacnz Ltd is an independent organisation that promotes health Kaye Baldwin care interventions which meet patients’ needs and are evidence Tony Fraser based, cost effective and suitable for the New Zealand context. Kyla Letman We develop and distribute evidence based resources which describe, facilitate and help overcome the barriers to best Clinical Advisory Group practice. Clive Cannons nz Michele Cray Bpac Ltd is currently funded through contracts with PHARMAC and DHBNZ. Margaret Gibbs nz Dr Rosemary Ikram Bpac Ltd has five shareholders: Procare Health, South Link Health, General Practice NZ, the University of Otago and Pegasus Dr Cam Kyle Health. -

DRI® Digoxin Assay
DRI® Digoxin Assay For In Vitro Diagnostic Use 1669 (25 mL, 8 mL Kit) 1669-A (25 mL, 8 mL Kit) Intended Use Reagent Preparation and Storage The DRI® Digoxin Assay is intended for the quantitative determination of digoxin in human The reagents are ready for use. No reagent preparation is required. All assay components, serum or plasma. when stored properly at 2-8°C, are stable until the expiration date indicated on the label. Summary and Explanation of the Test Specimen Collection and Handling Digitalis is known to have the ability to increase the force and velocity of myocardial Pharmacokinetic factors, such as dosage form, mode of administration, concomitant drug therapy contraction.1 Digoxin is one of the most commonly used forms of digitalis in the treatment as well as the patient’s clinical condition may influence the correct time of sample collection.2,3 For of congestive heart failure and arrhythmia such as atrial fibrillation and atrial flutter. The reliable interpretation of results, a serum specimen should be collected 6 to 8 hours following therapeutic range of digoxin is narrow. Futhermore, individual differences in drug absorption, the last oral dose of digoxin. Either serum or heparin and EDTA treated plasma samples can distribution, metabolism, and excretion as well as factors such as concurrent use of other drugs be used with the assay. Samples may be stored refrigerated at 2-8°C for up to 7 days or frozen and illness can also alter the serum concentration in response to a given dosage. Monitoring (-20°C) for up to 6 months. -

Crowdsourcing Analysis of Off-Label Intervention Usage in Amyotrophic Lateral Sclersosis
CROWDSOURCING ANALYSIS OF OFF-LABEL INTERVENTION USAGE IN AMYOTROPHIC LATERAL SCLERSOSIS A Thesis Presented to The Academic Faculty by Benjamin I. Mertens In Partial Fulfillment of the Requirements for the Degree B.S. in Biomedical Engineering with the Research Option in the Wallace H. Coulter School of Biomedical Engineering Georgia Institute of Technology Spring 2017 1 ACKNOWLEDGEMENTS I would like to thank my research advisor, Dr. Cassie Mitchell, first and foremost, for helping me through this long process of research, analysis, writing this thesis and the corresponding article to be submitted for peer-reviewed journal publication. There is no way I could have done this, or written it as eloquently without her. Next, I would like to acknowledge Grant Coan, Gloria Bowen, and Nathan Neuhart for all helping me on the road to writing this paper. Lastly, I would like to thank Dr. Lena Ting for her consultation as the faculty reader. 2 TABLE OF CONTENTS Page ACKNOWLEDGEMENTS 2 LIST OF TABLES 4 LIST OF FIGURES 5 LIST OF ABBREVIATIONS 6 SUMMARY 7 CHAPTERS 1 Philosophy 9 2 Crowdsourced Off-label Medications to Extend ALS Disease Duration 12 Introduction 12 Methodology 15 Results 18 Discussion 25 Tables 33 Figures 38 APPENDIX A: All Table 2 Appearance in Patients and Visits 44 APPENDIX B: All Table 3 Appearance in Patients and Visits 114 REFERENCES 129 3 LIST OF TABLES Page Table 1: Database Overview 33 Table 2: Ontology of Individual Medications 34 Table 3: Ontology of Intervention Groups 36 4 LIST OF FIGURES Page Figure 1: Relational circle -
The ECG Made Very Easy Indeed: a Beginner’S Guide
Part 1 The ECG made very easy indeed: a beginner’s guide The ECG made very easy indeed 1 What is an ECG? 1 The heart is a pump driven by intrinsic electrical When do you need an ECG? 1 impulses which make the heart beat. An ECG is a paper recording of that electrical activity. The ECG records where How to record an ECG 2 electrical impulses start and how they flow through the How to interpret an ECG: the basics 2 heart. It does not measure how well the heart is pumping. The electrical activity of the heart starts in the ‘inter- The ECG waves and what they mean 2 nal pacemaker’, which is called the sinoatrial node. This Interpretation starts here! 4 is in the right atrium. The normal rhythm is called ‘sinus rhythm’ (properly it should be called sinoatrial rhythm, Rhythms you must be able to recognize 8 but it isn’t). The way electrical impulses flow through the Patterns you must be able to recognize 10 heart is called conduction. Abnormalities in the electrical activity of the heart can The normal ECG and its variants 13 result in abnormal conduction or rhythms where the heart ECG red flags 14 may go too quickly, too slowly, or beat irregularly. Changes to the normal flow of electricity through the heart can be shown on an ECG and may indicate damaged This guide has been written for those who are just starting heart muscle. Heart muscle can be damaged by many to use ECGs in their clinical practice. -
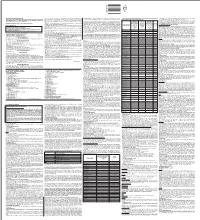
Full Prescribing Information Warning: Suicidal Thoughts
tablets (SR) BUPROPION hydrochloride extended-release HIGHLIGHTS OF PRESCRIBING INFORMATION anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide. Observe hydrochloride extended-release tablets (SR) was reported. However, the symptoms persisted in some Table 3. Adverse Reactions Reported by at Least 1% of Subjects on Active Treatment and at a tablets (SR) may be necessary when coadministered with ritonavir, lopinavir, or efavirenz [see Clinical These highlights do not include all the information needed to use bupropion hydrochloride patients attempting to quit smoking with Bupropion hydrochloride extended-release tablets, USP cases; therefore, ongoing monitoring and supportive care should be provided until symptoms resolve. Greater Frequency than Placebo in the Comparator Trial Pharmacology (12.3)] but should not exceed the maximum recommended dose. extended-release tablets (SR) safely and effectively. See full prescribing information for (SR) for the occurrence of such symptoms and instruct them to discontinue Bupropion hydrochloride Carbamazepine, Phenobarbital, Phenytoin: While not systematically studied, these drugs extended-release tablets, USP (SR) and contact a healthcare provider if they experience such adverse The neuropsychiatric safety of Bupropion hydrochloride extended-release tablets (SR) was evaluated in Bupropion Bupropion may induce the metabolism of bupropion and may decrease bupropion exposure [see Clinical bupropion hydrochloride extended-release tablets (SR). Nicotine events. (5.2) a randomized, double-blind, active-and placebo-controlled study that included patients without a history Hydrochloride Hydrochloride Pharmacology (12.3)]. If bupropion is used concomitantly with a CYP inducer, it may be necessary Transdermal BUPROPION hydrochloride extended-release tablets (SR), for oral use • Seizure risk: The risk is dose-related. -

Effect of Amlodipine and Indomethacin in Electrical and Picrotoxin Induced Convulsions in Mice
DOI: 10.5958/2319-5886.2014.00402.0 International Journal of Medical Research & Health Sciences www.ijmrhs.com Volume 3 Issue 3 Coden: IJMRHS Copyright @2014 ISSN: 2319-5886 Received: 9th Apr 2014 Revised: 3rd Jun 2014 Accepted: 14th Jun 2014 Research Article EFFECT OF AMLODIPINE AND INDOMETHACIN IN ELECTRICAL AND PICROTOXIN INDUCED CONVULSIONS IN MICE *Jagathi Devi N1, Prasanna V2 1Assistant Professor, 2Professor and Head, Department of Pharmacology, Osmania Medical College, Hyderabad *Corresponding author email: [email protected] ABSTRACT Background and Objectives: Antiepileptic drugs (AEDs) are the drugs used in the treatment of epilepsy. Many AEDs have been developed, but the ideal AED which can not only prevent but also abolish seizures by correcting the underlying pathophysiology is still not in sight. Calcium channel blockers (CCBs) may form such a group, as the initiation of epileptogenic activity in the neuron is connected with a phenomenon known as “intrinsic burst firing” which is activated by inward calcium current. In this study, Amlodipine, a CCB of the dihydropyridine class was evaluated for its anticonvulsant activity in mice. It was compared with Phenytoin sodium, one of the oldest anti epileptic drugs. Amlodipine was also combined with Indomethacin, a conventional NSAID, to look for any potentiating effect of this prostaglandin-synthesis inhibitor. Materials and Methods: A total of 48 adult Swiss albino mice of either sex weighing 20-30 G were used for this study; 48 were divided into 8 groups, each group containing 6 mice. Group 1-4 MES (50 m Amp for 0.1 secs) induced convulsion method, Group 5-8 evaluated by using the chemo-convulsant, picrotoxin (0.7 mg / kg). -

Neurochemical Mechanisms Underlying Alcohol Withdrawal
Neurochemical Mechanisms Underlying Alcohol Withdrawal John Littleton, MD, Ph.D. More than 50 years ago, C.K. Himmelsbach first suggested that physiological mechanisms responsible for maintaining a stable state of equilibrium (i.e., homeostasis) in the patient’s body and brain are responsible for drug tolerance and the drug withdrawal syndrome. In the latter case, he suggested that the absence of the drug leaves these same homeostatic mechanisms exposed, leading to the withdrawal syndrome. This theory provides the framework for a majority of neurochemical investigations of the adaptations that occur in alcohol dependence and how these adaptations may precipitate withdrawal. This article examines the Himmelsbach theory and its application to alcohol withdrawal; reviews the animal models being used to study withdrawal; and looks at the postulated neuroadaptations in three systems—the gamma-aminobutyric acid (GABA) neurotransmitter system, the glutamate neurotransmitter system, and the calcium channel system that regulates various processes inside neurons. The role of these neuroadaptations in withdrawal and the clinical implications of this research also are considered. KEY WORDS: AOD withdrawal syndrome; neurochemistry; biochemical mechanism; AOD tolerance; brain; homeostasis; biological AOD dependence; biological AOD use; disorder theory; biological adaptation; animal model; GABA receptors; glutamate receptors; calcium channel; proteins; detoxification; brain damage; disease severity; AODD (alcohol and other drug dependence) relapse; literature review uring the past 25 years research- science models used to study with- of the reasons why advances in basic ers have made rapid progress drawal neurochemistry as well as a research have not yet been translated Din understanding the chemi- reluctance on the part of clinicians to into therapeutic gains and suggests cal activities that occur in the nervous consider new treatments. -

Practice Questions of Backlog Examination - 20 Questions (2M Each) Select Correct Answer for the Following Multiple Choice Questions
Practice Questions of backlog examination - 20 Questions (2M each) Select correct answer for the following Multiple Choice Questions. Final Year B. Pharm. (Sem-VII) (CBSGS) Pharmaceutical Chemistry III 1. One of these is a HDAC inhibitor. a. Vorinostat b. Epalristat c. Imatinib d. Oxaliplatin 2. AZT, an antiviral agent is a a. Protease inhibitor b. Nonnucleoside RT inhibitor c. Nucleoside RT inhibitor d. Entry inhibitor 3. The sugar present in digitalis glycosides is a. Sucrose b. Glucose c. Digitoxose d. Galactose 4. The active metabolite of verapamil is a product of a. O-dealkylation b. C-dealkylation c. N-dealkylation d. Reduction 5. The epimer of Qunidine has the following activity a. Anti-diabetic b. Anti-malarial c. Analgesic d. Antihypertensive 6. N-(5-Sulfamoyl-1,3,4-thiadiazol-2-yl) acetamide is the IUPAC name of a. Furosemide b. Acetazolamide c. Methazolamide d. Thiazoleamide 7. Enalapril and captopril are a. ACE inhibitors b. Prodrugs c. Used in diarrhoea d. Used as a prodrug Practice Questions of backlog examination - 20 Questions (2M each) Select correct answer for the following Multiple Choice Questions. 8. The Phase -2 metabolite of one of these drugs is active a. Esmolol b. Prazocin c. Minoxidil d. Timolol 9. Which of following is anthranilic acid derivative? (a) Furosemide (b) Bumetanide (c) Ethacrynic acid (d) None 10. Aspirin is chemically a. A reverse ester of salicylic acid b. An amide of salicylic acid c. An ester of salicylic acid d. An imide of salicylic acid 11. The structure of 5-Fluorouracil, an anticancer agent has a. Purine nucleus b. -

Calcium Current Block by (-)-Pentobarbital, Phenobarbital
The Journal of Neuroscience, August 1993, 13(E): 321 l-3221 Calcium Current Block by (-)-Pentobarbital, Phenobarbital, and CHEB but not (+)-Pentobarbital in Acutely Isolated Hippocampal CA1 Neurons: Comparison with Effects on GABA-activated Cl- Current Jarlath M. H. ffrench-Mullen,’ Jeffery L. Barker,* and Michael A. Rogawski3 ‘Department of Pharmacology, Zeneca Pharmaceuticals Group, Zeneca Inc., Wilmington, Delaware 19897 and *Laboratory of Neurophysiology, and 3Neuronal Excitability Section, Epilepsy Research Branch, National Institute of Neurological Disorders and Stroke, National Institutes of Health, Bethesda, Maryland 20892 Block of a voltage-activated Ca*+ channel current by pheno- Ca*+ current, whereas the sedative effects that occur at high- barbital (PHB), 5-(2-cyclohexylideneethyl)-5-ethyl barbituric er concentrations could reflect stronger Ca2+ current block- acid (CHEB), and the optical R(-)- and S(+)-enantiomers of ade. The powerful sedative-hypnotic action of (-)-PB may pentobarbital (PB) was examined in freshly dissociated adult reflect greater maximal enhancement of GABA responses guinea pig hippocampal CA1 neurons; the effects of the in conjunction with strong inhibition of Ca2+ current. The barbiturates on GABA-activated Cl- current were also char- convulsant action of CHEB is unlikely to be related to its acterized in the same preparation. (-)-PB, PHB, and CHEB effects on the Ca*+ current. produced a reversible, concentration-dependent block of the [Key words: calcium channel, GABA receptor, (-)-pen- peak Ca*+ channel current (3 mM Ba2+ as the charge carrier) tobarbital, (+)-pentobarbital, phenobarbital, CHEB [S-(2-cy- evoked by depolarization from -80 to - 10 mV (I&,, values, clohexylideneethyl)-S-ethyl barbituric acid], CA 1 hippocam- 3.5, 72, and 118 PM, respectively). -

Basic Rhythm Recognition
Electrocardiographic Interpretation Basic Rhythm Recognition William Brady, MD Department of Emergency Medicine Cardiac Rhythms Anatomy of a Rhythm Strip A Review of the Electrical System Intrinsic Pacemakers Cells These cells have property known as “Automaticity”— means they can spontaneously depolarize. Sinus Node Primary pacemaker Fires at a rate of 60-100 bpm AV Junction Fires at a rate of 40-60 bpm Ventricular (Purkinje Fibers) Less than 40 bpm What’s Normal P Wave Atrial Depolarization PR Interval (Normal 0.12-0.20) Beginning of the P to onset of QRS QRS Ventricular Depolarization QRS Interval (Normal <0.10) Period (or length of time) it takes for the ventricles to depolarize The Key to Success… …A systematic approach! Rate Rhythm P Waves PR Interval P and QRS Correlation QRS Rate Pacemaker A rather ill patient……… Very apparent inferolateral STEMI……with less apparent complete heart block RATE . Fast vs Slow . QRS Width Narrow QRS Wide QRS Narrow QRS Wide QRS Tachycardia Tachycardia Bradycardia Bradycardia Regular Irregular Regular Irregular Sinus Brady Idioventricular A-Fib / Flutter Bradycardia w/ BBB Sinus Tach A-Fib VT PVT Junctional 2 AVB / II PSVT A-Flutter SVT aberrant A-Fib 1 AVB 3 AVB A-Flutter MAT 2 AVB / I or II PAT PAT 3 AVB ST PAC / PVC Stability Hypotension / hypoperfusion Altered mental status Chest pain – Coronary ischemic Dyspnea – Pulmonary edema Sinus Rhythm Sinus Rhythm P Wave PR Interval QRS Rate Rhythm Pacemaker Comment . Before . Constant, . Rate 60-100 . Regular . SA Node Upright in each QRS regular . Interval =/< leads I, II, . Look . Interval .12- .10 & III alike .20 Conduction Image reference: Cardionetics/ http://www.cardionetics.com/docs/healthcr/ecg/arrhy/0100_bd.htm Sinus Pause A delay of activation within the atria for a period between 1.7 and 3 seconds A palpitation is likely to be felt by the patient as the sinus beat following the pause may be a heavy beat.