Fernandez-Sanchez Et Al
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Crowdsourcing Analysis of Off-Label Intervention Usage in Amyotrophic Lateral Sclersosis
CROWDSOURCING ANALYSIS OF OFF-LABEL INTERVENTION USAGE IN AMYOTROPHIC LATERAL SCLERSOSIS A Thesis Presented to The Academic Faculty by Benjamin I. Mertens In Partial Fulfillment of the Requirements for the Degree B.S. in Biomedical Engineering with the Research Option in the Wallace H. Coulter School of Biomedical Engineering Georgia Institute of Technology Spring 2017 1 ACKNOWLEDGEMENTS I would like to thank my research advisor, Dr. Cassie Mitchell, first and foremost, for helping me through this long process of research, analysis, writing this thesis and the corresponding article to be submitted for peer-reviewed journal publication. There is no way I could have done this, or written it as eloquently without her. Next, I would like to acknowledge Grant Coan, Gloria Bowen, and Nathan Neuhart for all helping me on the road to writing this paper. Lastly, I would like to thank Dr. Lena Ting for her consultation as the faculty reader. 2 TABLE OF CONTENTS Page ACKNOWLEDGEMENTS 2 LIST OF TABLES 4 LIST OF FIGURES 5 LIST OF ABBREVIATIONS 6 SUMMARY 7 CHAPTERS 1 Philosophy 9 2 Crowdsourced Off-label Medications to Extend ALS Disease Duration 12 Introduction 12 Methodology 15 Results 18 Discussion 25 Tables 33 Figures 38 APPENDIX A: All Table 2 Appearance in Patients and Visits 44 APPENDIX B: All Table 3 Appearance in Patients and Visits 114 REFERENCES 129 3 LIST OF TABLES Page Table 1: Database Overview 33 Table 2: Ontology of Individual Medications 34 Table 3: Ontology of Intervention Groups 36 4 LIST OF FIGURES Page Figure 1: Relational circle -

Practice Questions of Backlog Examination - 20 Questions (2M Each) Select Correct Answer for the Following Multiple Choice Questions
Practice Questions of backlog examination - 20 Questions (2M each) Select correct answer for the following Multiple Choice Questions. Final Year B. Pharm. (Sem-VII) (CBSGS) Pharmaceutical Chemistry III 1. One of these is a HDAC inhibitor. a. Vorinostat b. Epalristat c. Imatinib d. Oxaliplatin 2. AZT, an antiviral agent is a a. Protease inhibitor b. Nonnucleoside RT inhibitor c. Nucleoside RT inhibitor d. Entry inhibitor 3. The sugar present in digitalis glycosides is a. Sucrose b. Glucose c. Digitoxose d. Galactose 4. The active metabolite of verapamil is a product of a. O-dealkylation b. C-dealkylation c. N-dealkylation d. Reduction 5. The epimer of Qunidine has the following activity a. Anti-diabetic b. Anti-malarial c. Analgesic d. Antihypertensive 6. N-(5-Sulfamoyl-1,3,4-thiadiazol-2-yl) acetamide is the IUPAC name of a. Furosemide b. Acetazolamide c. Methazolamide d. Thiazoleamide 7. Enalapril and captopril are a. ACE inhibitors b. Prodrugs c. Used in diarrhoea d. Used as a prodrug Practice Questions of backlog examination - 20 Questions (2M each) Select correct answer for the following Multiple Choice Questions. 8. The Phase -2 metabolite of one of these drugs is active a. Esmolol b. Prazocin c. Minoxidil d. Timolol 9. Which of following is anthranilic acid derivative? (a) Furosemide (b) Bumetanide (c) Ethacrynic acid (d) None 10. Aspirin is chemically a. A reverse ester of salicylic acid b. An amide of salicylic acid c. An ester of salicylic acid d. An imide of salicylic acid 11. The structure of 5-Fluorouracil, an anticancer agent has a. Purine nucleus b. -

Breaking Barriers to Novel Analgesic Drug Development
REVIEWS Breaking barriers to novel analgesic drug development Ajay S. Yekkirala1–3, David P. Roberson1–3, Bruce P. Bean1 and Clifford J. Woolf1,2 Abstract | Acute and chronic pain complaints, although common, are generally poorly served by existing therapies. This unmet clinical need reflects a failure to develop novel classes of analgesics with superior efficacy, diminished adverse effects and a lower abuse liability than those currently available. Reasons for this include the heterogeneity of clinical pain conditions, the complexity and diversity of underlying pathophysiological mechanisms, and the unreliability of some preclinical pain models. However, recent advances in our understanding of the neurobiology of pain are beginning to offer opportunities for developing novel therapeutic strategies and revisiting existing targets, including modulating ion channels, enzymes and G-protein-coupled receptors. Pain is the primary reason why people seek medical blockbuster model of one treatment for all pain condi- Analgesics 12 Pharmacological agents or care: more than 40% of the US population is affected tions is not tenable . The poor predictability of preclin- 1 ligands that produce analgesia. by chronic pain . In the United States alone in 2013, the ical ‘pain’ models can result in candidates being selected overall cost of treating certain chronic pain conditions that do not have activity in the conditions suffered by Tolerance amounted to more than US$130 billion2. Currently avail- patients13 (BOX 1). Conversely, difficulty in ensuring A state in which the drug no analgesics longer produces the same able — nonsteroidal anti-inflammatory drugs target engagement, lack of sensitivity of clinical trials effect and a higher dose is (NSAIDs), amine reuptake inhibitors, anti epileptic and distortions induced by placebos increase the risk therefore needed. -

Small Dose... Big Poison
Traps for the unwary George Braitberg Ed Oakley Small dose... Big poison All substances are poisons; Background There is none which is not a poison. It is not possible to identify all toxic substances in a single The right dose differentiates a poison from a remedy. journal article. However, there are some exposures that in Paracelsus (1493–1541)1 small doses are potentially fatal. Many of these exposures are particularly toxic to children. Using data from poison control centres, it is possible to recognise this group of Poisoning is a frequent occurrence with a low fatality rate. exposures. In 2008, almost 2.5 million human exposures were reported to the National Poison Data System (NPDS) in the United Objective States, of which only 1315 were thought to contribute This article provides information to assist the general to fatality.2 The most common poisons associated with practitioner to identify potential toxic substance exposures in children. fatalities are shown in Figure 1. Polypharmacy (the ingestion of more than one drug) is far more common. Discussion In this article the authors report the signs and symptoms Substances most frequently involved in human exposure are shown of toxic exposures and identify the time of onset. Where in Figure 2. In paediatric exposures there is an over-representation clear recommendations on the period of observation and of personal care products, cleaning solutions and other household known fatal dose are available, these are provided. We do not discuss management or disposition, and advise readers products, with ingestions peaking in the toddler age group. This to contact the Poison Information Service or a toxicologist reflects the acquisition of developmental milestones and subsequent for this advice. -

Therapeutic Approaches to Genetic Ion Channelopathies and Perspectives in Drug Discovery
fphar-07-00121 May 7, 2016 Time: 11:45 # 1 REVIEW published: 10 May 2016 doi: 10.3389/fphar.2016.00121 Therapeutic Approaches to Genetic Ion Channelopathies and Perspectives in Drug Discovery Paola Imbrici1*, Antonella Liantonio1, Giulia M. Camerino1, Michela De Bellis1, Claudia Camerino2, Antonietta Mele1, Arcangela Giustino3, Sabata Pierno1, Annamaria De Luca1, Domenico Tricarico1, Jean-Francois Desaphy3 and Diana Conte1 1 Department of Pharmacy – Drug Sciences, University of Bari “Aldo Moro”, Bari, Italy, 2 Department of Basic Medical Sciences, Neurosciences and Sense Organs, University of Bari “Aldo Moro”, Bari, Italy, 3 Department of Biomedical Sciences and Human Oncology, University of Bari “Aldo Moro”, Bari, Italy In the human genome more than 400 genes encode ion channels, which are transmembrane proteins mediating ion fluxes across membranes. Being expressed in all cell types, they are involved in almost all physiological processes, including sense perception, neurotransmission, muscle contraction, secretion, immune response, cell proliferation, and differentiation. Due to the widespread tissue distribution of ion channels and their physiological functions, mutations in genes encoding ion channel subunits, or their interacting proteins, are responsible for inherited ion channelopathies. These diseases can range from common to very rare disorders and their severity can be mild, Edited by: disabling, or life-threatening. In spite of this, ion channels are the primary target of only Maria Cristina D’Adamo, University of Perugia, Italy about 5% of the marketed drugs suggesting their potential in drug discovery. The current Reviewed by: review summarizes the therapeutic management of the principal ion channelopathies Mirko Baruscotti, of central and peripheral nervous system, heart, kidney, bone, skeletal muscle and University of Milano, Italy Adrien Moreau, pancreas, resulting from mutations in calcium, sodium, potassium, and chloride ion Institut Neuromyogene – École channels. -

Chapter 151 – Antidepressants
Crack Cast Show Notes – Skin and Soft Tissue Infections www.canadiem.org Chapter 151 – Antidepressants Key Concepts ❏ Although rarely used for depression, MAOIs are used in the treatment of Parkinson’s disease ❏ Because serious symptoms can occur after a lengthy latent period, patients with reported MAOI overdose should be admitted for 24 hours, regardless of symptoms. Symptoms are characterized by tachycardia, hypertension, and CNS changes, and later cardiovascular collapse. ❏ The primary manifestations of TCA toxicity are seizures, tachycardia, and intraventricular conduction delay. IV sodium bicarbonate should be administered for QRS prolongation. ❏ DO NOT USE PHYSOSTIGMINE IN TCA OVERDOSE ❏ SSRIs are comparatively benign in overdose. ❏ SNRI ingestions can result in seizures, tachycardia, and occasionally intraventricular conduction delay. ❏ The hallmark feature of serotonin syndrome is lower extremity rigidity (spasticity) with spontaneous or inducible clonus, especially at the ankles. ❏ Serotonin syndrome is primarily treated with supportive care, including discontinuation of the offending agent, and benzodiazepines. Sign Post 1) List 7 pharmacodynamic effects of cyclic antidepressants and describe the physiologic result 2) What are the ECG findings associated with TCA toxicity and what are their implications 3) Describe the management of TCA toxicity 4) What are the diagnostic criteria for Serotonin Syndrome? 5) How can you discern between NMS and Serotonin Syndrome? 6) What are the common meds causing Serotonin Syndrome? 7) Describe the management of Serotonin Syndrome 8) What is the primary risk of toxicity in Bupropion? 9) What are the 3 mechanisms by which MAOI toxicity can occur? And what is the clinical syndrome? 10) List 5 foods and 5 classes of meds that can interact to cause MAOI toxicity 11) Describe the management of MAOI toxicity. -
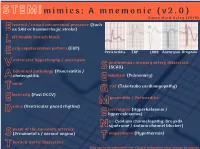
STEMI Mimics V2
S T E M I m i m i c s ; A m n e m o n i c ( v 2 . 0 ) S i m o n M a r k D a l e y ( 2 0 1 9 ) E levated / raised intracranial pressure (Such as SAH or haemorrhagic stroke) L eft bundle branch block arly repolarisation pattern (ERP) E Pericarditis ERP LBBB Aneurysm Brugada Ventricular hypertrophy / aneurysm S pontaneous coronary artery dissection (SCAD) Abdominal pathology (Pancreatitis / cholecystitis E mbolism (Pulmonary) T umor G rief (Takotsubo cardiomyopathy) E lectricity (Post DCCV) M yocarditis / Pericarditis Device (Ventricular paced rhythm) E lectrolytes (Hyperkalaemia / hypercalcaemia) N a+ (Sodium channelopathy; Brugada syndrome / sodium channel blocker) S pasm of the coronary arteries (Prinzmetal's / variant angina) T emperature (Hypothermia) T horacic aortic dissection May not be an exhaustive list; Clinical judgement must always be applied. Ventricular hypertrophy / aneurysm; Ventricular hypertrophy. Accounts for up to 25% of ED presentations with chest pain. The left ventricle hypertrophies in response to pressure secondary to conditions such as hypertension and aortic stenosis, as well as aortic regurgitation, mitral regurgitation, coarctation of the aorta, and hypertrophic cardiomyopathy. This leads to the following ECG features; Increased R wave amplitude in leads I, aVL and v4-v6. Increased S wave depth in leads III, aVR,v1-v3. The thickened LV wall leads to prolonged depolarisation, increased R wave peak time and delayed repolarisation (ST and T wave abnormalities) in the lateral leads. Diagnostic criteria (Sokolov-Lyon); S wave depth in v1 + tallest R wave height in v5-v6 >35mm. (Courtesy of LITFL) Ventricular hypertrophy / aneurysm; Ventricular aneurysm; Persistent ST segment elevation following an acute myocardial infarction. -

Nav1.7 As a Pain Target
ÔØ ÅÒÙ×Ö ÔØ NaV 1.7 as a pain target – from gene to pharmacology Irina Vetter, Jennifer R. Deuis, Alexander Mueller, Mathilde R. Israel, Hana Starobova, Alan Zhang, Lachlan Rash, Mehdi Mobli PII: S0163-7258(16)30241-8 DOI: doi:10.1016/j.pharmthera.2016.11.015 Reference: JPT 6999 To appear in: Pharmacology and Therapeutics Please cite this article as: Vetter, I., Deuis, J.R., Mueller, A., Israel, M.R., Starobova, H., Zhang, A., Rash, L. & Mobli, M., NaV 1.7 as a pain target – from gene to pharmacology, Pharmacology and Therapeutics (2016), doi:10.1016/j.pharmthera.2016.11.015 This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. ACCEPTED MANUSCRIPT P&T #23131 Na V1.7 as a pain target – from gene to pharmacology Irina Vetter* 1,2 , Jennifer R. Deuis 1, Alexander Mueller 1, Mathilde R. Israel 1, Hana Starobova 1, Alan Zhang 3, Lachlan Rash 1,4 , Mehdi Mobli 3 1 Institute for Molecular Bioscience, Centre for Pain Research, The University of Queensland, St Lucia, Qld 4072, Australia 2 School of Pharmacy, The University of Queensland, Woolloongabba, Qld 4102, Australia 3 Centre for Advanced Imaging, The University of Queensland, St Lucia, Qld 4072, Australia 4 School of Biomedical Sciences, The University of Queensland, St Lucia, Qld 4072, Australia * Corresponding author. -

Voltage-Gated Sodium Channels and Blockers: an Overview and Where Will They Go?*
Current Medical Science 39(6):863-873,2019 DOICurrent https://doi.org/10.1007/s11596-019-2117-0 Medical Science 39(6):2019 863 Voltage-gated Sodium Channels and Blockers: An Overview and Where Will They Go?* Zhi-mei LI1, Li-xia CHEN2#, Hua LI1# 1Hubei Key Laboratory of Natural Medicinal Chemistry and Resource Evaluation, School of Pharmacy, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430030, China 2Wuya College of Innovation, Key Laboratory of Structure-Based Drug Design & Discovery, Ministry of Education, Shenyang Pharmaceutical University, Shenyang 110016, China Huazhong University of Science and Technology 2019 Summary: Voltage-gated sodium (Nav) channels are critical players in the generation and propagation of action potentials by triggering membrane depolarization. Mutations in Nav channels are associated with a variety of channelopathies, which makes them relevant targets for pharmaceutical intervention. So far, the cryoelectron microscopic structure of the human Nav1.2, Nav1.4, and Nav1.7 has been reported, which sheds light on the molecular basis of functional mechanism of Nav channels and provides a path toward structure-based drug discovery. In this review, we focus on the recent advances in the structure, molecular mechanism and modulation of Nav channels, and state updated sodium channel blockers for the treatment of pathophysiology disorders and briefly discuss where the blockers may be developed in the future. Key words: voltage-gated sodium channels; blockers; Nav channel structures; channelopathies Life did not come into existence until living In this review, we focus on voltage-gated organisms were enclosed by one or more membranes sodium (Nav) channels, which selectively conduct which cut them off from the chaotic world at a sodium ions movement in response to variations of molecular level. -

A High Throughput Screen Identifies Nefopam As Targeting Cell Proliferation in B-Catenin Driven Neoplastic and Reactive Fibroproliferative Disorders
A High Throughput Screen Identifies Nefopam as Targeting Cell Proliferation in b-Catenin Driven Neoplastic and Reactive Fibroproliferative Disorders Raymond Poon1, Helen Hong1, Xin Wei2, James Pan3, Benjamin A. Alman1,4* 1 Program in Developmental and Stem Cell Biology, Hospital for Sick Children, Toronto, Ontario, Canada, 2 Campbell Family Institute for Breast Cancer Research, University Health Network, Toronto, Ontario, Canada, 3 Donnelly Centre for Cellular and Molecular Research and Banting and Best Institute for Medical Research, University of Toronto, Toronto, Ontario, Canada, 4 Division of Orthopaedics, Department of Surgery, University of Toronto, Toronto, Ontario, Canada Abstract Fibroproliferative disorders include neoplastic and reactive processes (e.g. desmoid tumor and hypertrophic scars). They are characterized by activation of b-catenin signaling, and effective pharmacologic approaches are lacking. Here we undertook a high throughput screen using human desmoid tumor cell cultures to identify agents that would inhibit cell viability in tumor cells but not normal fibroblasts. Agents were then tested in additional cell cultures for an effect on cell proliferation, apoptosis, and b-catenin protein level. Ultimately they were tested in Apc1638N mice, which develop desmoid tumors, as well as in wild type mice subjected to full thickness skin wounds. The screen identified Neofopam, as an agent that inhibited cell numbers to 42% of baseline in cell cultures from b-catenin driven fibroproliferative disorders. Nefopam decreased cell proliferation and b-catenin protein level to 50% of baseline in these same cell cultures. The half maximal effective concentration in-vitro was 0.5 uM and there was a plateau in the effect after 48 hours of treatment. -

Sodium Channel Na Channels;Na+ Channels
Sodium Channel Na channels;Na+ channels Sodium channels are integral membrane proteins that form ion channels, conducting sodium ions (Na +) through a cell's plasma membrane. They are classified according to the trigger that opens the channel for such ions, i.e. either a voltage-change (Voltage-gated, voltage-sensitive, or voltage-dependent sodium channel also called VGSCs or Nav channel) or a binding of a substance (a ligand) to the channel (ligand-gated sodium channels). In excitable cells such as neurons, myocytes, and certain types of glia, sodium channels are responsible for the rising phase of action potentials. Voltage-gated Na+ channels can exist in any of three distinct states: deactivated (closed), activated (open), or inactivated (closed). Ligand-gated sodium channels are activated by binding of a ligand instead of a change in membrane potential. www.MedChemExpress.com 1 Sodium Channel Inhibitors & Modulators (+)-Kavain (-)-Sparteine sulfate pentahydrate Cat. No.: HY-B1671 ((-)-Lupinidine (sulfate pentahydrate)) Cat. No.: HY-B1304 Bioactivity: (+)-Kavain, a main kavalactone extracted from Piper Bioactivity: (-)-Sparteine sulfate pentahydrate ((-)-Lupinidine sulfate methysticum, has anticonvulsive properties, attenuating pentahydrate) is a class 1a antiarrhythmic agent and a sodium vascular smooth muscle contraction through interactions with channel blocker. It is an alkaloid, can chelate the bivalents voltage-dependent Na + and Ca 2+ channels [1]. (+)-Kav… calcium and magnesium. Purity: 99.98% Purity: 98.0% Clinical Data: No Development Reported Clinical Data: Launched Size: 10mM x 1mL in DMSO, Size: 10mM x 1mL in DMSO, 5 mg, 10 mg 50 mg A-803467 Ajmaline Cat. No.: HY-11079 (Cardiorythmine; (+)-Ajmaline) Cat. No.: HY-B1167 Bioactivity: A 803467 is a selective Nav1.8 sodium channel blocker with an Bioactivity: Ajmaline is an alkaloid that is class Ia antiarrhythmic agent. -

Toxidrome-Based Approach to Common Poisonings
ASIA PACIFIC JOURNAL of MEDICAL TOXICOLOGY APJMT 3;1 http://apjmt.mums.ac.ir March 2014 REVIEW ARTICLE Toxidrome-based Approach to Common Poisonings BRUNO MÉGARBANE* Reanimation and Medical Toxicology Department, University Paris-Diderot, Paris, France Abstract Poisoning remains a major cause of hospital admission into the emergency department and intensive care unit. Proper diagnosis is the cornerstone for optimal management of poisoned patients. Since the definitive analytical confirmation of the nature of the toxicant involved in the poisoning cannot be rapidly obtained in the majority of healthcare facilities, diagnosis relies on the medical history and the rigorous clinical examination of the patients well as results of the routine biological tests and the electrocardiogram. Identification of the toxidromes addresses not only the correct diagnosis but also rules out other differential diagnoses. Despite no definitive predictive value, this clinical approach facilitates making decision on empirical treatments and emergent antidotes. Pharmacodynamic tests using specific antidotes including naloxone for opioids and flumazenil for benzodiazepines and its analogues are also helpful to assess the final diagnosis in comatose patients. The objective of this article is to review the toxidrome- based approach to common poisonings before toxicological analysis enables the confirmation of the initially suspected toxic etiology. Keywords: Anticholinergic Syndrome; Poisoning; Serotonin Syndrome; Substance Withdrawal Syndrome; Toxidrome How to cite this article: Mégarbane B. Toxidrome-based Approach to Common Poisonings. Asia Pac J Med Toxicol 2014;3:2-12. be individualized for each patient (4): INTRODUCTION 1) The patient has been exposed intentionally or Drug poisoning, either accidental or intentional, accounts accidentally to a toxic agent, but his/her clinical for one of the most common causes of admission to the examinations are normal.