Identification of UBAP1 Mutations in Juvenile Hereditary Spastic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
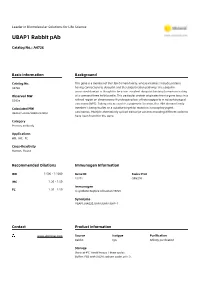
UBAP1 Rabbit Pab
Leader in Biomolecular Solutions for Life Science UBAP1 Rabbit pAb Catalog No.: A4726 Basic Information Background Catalog No. This gene is a member of the UBA domain family, whose members include proteins A4726 having connections to ubiquitin and the ubiquitination pathway. The ubiquitin associated domain is thought to be a non-covalent ubiquitin binding domain consisting Observed MW of a compact three helix bundle. This particular protein originates from a gene locus in a 55kDa refined region on chromosome 9 undergoing loss of heterozygosity in nasopharyngeal carcinoma (NPC). Taking into account its cytogenetic location, this UBA domain family Calculated MW member is being studies as a putative target for mutation in nasopharyngeal 48kDa/55kDa/58kDa/61kDa carcinomas. Multiple alternatively spliced transcript variants encoding different isoforms have been found for this gene. Category Primary antibody Applications WB, IHC, FC Cross-Reactivity Human, Mouse Recommended Dilutions Immunogen Information WB 1:500 - 1:1000 Gene ID Swiss Prot 51271 Q9NZ09 IHC 1:20 - 1:50 Immunogen 1:20 - 1:50 FC A synthetic Peptide of human UBAP1 Synonyms UBAP1;NAG20;UAP;UBAP;UBAP-1 Contact Product Information www.abclonal.com Source Isotype Purification Rabbit IgG Affinity purification Storage Store at 4℃. Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide, pH7.3. Validation Data Western blot analysis of extracts of mouse liver, using UBAP1 antibody (A4726). Secondary antibody: HRP Goat Anti-Rabbit IgG (H+L) (AS014) at 1:10000 dilution. Lysates/proteins: 25ug per lane. Blocking buffer: 3% nonfat dry milk in TBST. Antibody | Protein | ELISA Kits | Enzyme | NGS | Service For research use only. -

Genetic Analysis of Over One Million People Identifies 535 New Loci Associated with Blood 2 Pressure Traits
1 Genetic analysis of over one million people identifies 535 new loci associated with blood 2 pressure traits. 3 4 Table of Contents 5 SUPPLEMENTARY TABLES LEGENDS……………………………………………………………………………….…….3 6 SUPPLEMENTARY FIGURES LEGENDS ........................................................................................ 6 7 SUPPLEMENTARY METHODS ................................................................................................... 10 8 1. UK Biobank data .................................................................................................................................... 10 9 2. UKB Quality Control ............................................................................................................................... 10 10 3. Phenotypic data ..................................................................................................................................... 11 11 4. UKB analysis ........................................................................................................................................... 11 12 5. Genomic inflation and confounding ....................................................................................................... 12 13 6. International Consortium for Blood Pressure (ICBP) GWAS .................................................................... 12 14 7. Meta-analyses of discovery datasets ..................................................................................................... 13 15 8. Linkage Disequilibrium calculations ...................................................................................................... -

UBAP1 Antibody
Product Datasheet UBAP1 Antibody Catalog No: #40173 Orders: [email protected] Description Support: [email protected] Product Name UBAP1 Antibody Host Species Rabbit Clonality Polyclonal Purification Antigen affinity purification. Applications IHC Species Reactivity Hu Specificity The antibody detects endogenous levels of total UBAP1 protein. Immunogen Type Protein Immunogen Description Fusion protein of human ubiquitin associated protein 1 Target Name UBAP1 Other Names UAP; UBAP; NAG20; UBAP-1 Accession No. Swiss-Prot:Q9NZ09Gene Accssion:BC098141 Concentration 1.1mg/ml Formulation Rabbit IgG in pH7.4 PBS, 0.05% NaN3, 40% Glycerol. Storage Store at -20°C Application Details Immunohistochemistry:1:25-1:100 Images Immunohistochemical analysis of paraffin-embedded Human liver cancer tissue using #40173 at dilution 1/20. Background This gene is a member of the UBA domain family, whose members include proteins having connections to ubiquitin and the ubiquitination pathway. The ubiquitin associated domain is thought to be a non-covalent ubiquitin binding domain consisting of a compact three helix bundle. This particular protein originates from a gene locus in a refined region on chromosome 9 undergoing loss of heterozygosity in nasopharyngeal carcinoma (NPC). Taking into account its cytogenetic location, this UBA domain family member is being studies as a putative target for mutation in nasopharyngeal carcinomas. Multiple alternatively spliced transcript variants encoding different isoforms have been found for this gene. Address: 8400 Baltimore Ave., Suite 302, College Park, MD 20740, USA http://www.sabbiotech.com 1 Note: This product is for in vitro research use only and is not intended for use in humans or animals. Address: 8400 Baltimore Ave., Suite 302, College Park, MD 20740, USA http://www.sabbiotech.com 2. -

Jhaldeman Dissertation
Creation of Versatile Cloning Platforms for Transgene Expression and Epigenome Editing and Their Application to Pancreatic Islet Biology by Jonathan Mark Haldeman Department of Pharmacology and Cancer Biology Duke University Date:_______________________ Approved: ___________________________ Christopher Newgard, Supervisor ___________________________ Deborah Muoio ___________________________ Donald McDonnell ___________________________ Qi-Jing Li ___________________________ Praveen Sethupathy Dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of Pharmacology and Cancer Biology in the Graduate School of Duke University 2018 i v ABSTRACT Creation of Versatile Cloning Platforms for Transgene Expression and Epigenome Editing and Their Application to Pancreatic Islet Biology by Jonathan Mark Haldeman Department of Pharmacology and Cancer Biology Duke University Date:_______________________ Approved: ___________________________ Christopher Newgard, Supervisor ___________________________ Deborah Muoio ___________________________ Donald McDonnell ___________________________ Qi-Jing Li ___________________________ Praveen Sethupathy An abstract of a dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of Pharmacology and Cancer Biology in the Graduate School of Duke University 2018 Copyright by Jonathan Mark Haldeman 2018 Abstract Insulin secreting β-cells within the pancreatic islets of Langerhans are vital to maintaining glycemic control. β-cell functional mass is lost during the progression to both Type 1 and Type 2 diabetes mellitus, resulting in hyperglycemia. Therefore, a major goal of diabetes research is to uncover pathways that can be exploited to induce β-cell replication while simultaneously maintaining β-cell function. We previously reported that adenovirus-mediated overexpression of the transcription factor PDX1 is sufficient to induce β-cell replication, but underlying mechanisms remain to be resolved. -

Systemic Investigation of Promoter-Wide Methylome and Genome Variations in Gout
International Journal of Molecular Sciences Article Systemic Investigation of Promoter-wide Methylome and Genome Variations in Gout Chia-Chun Tseng 1,2, Man Chun Wong 3, Wei-Ting Liao 3,4,*, Chung-Jen Chen 5, Su-Chen Lee 6, Jeng-Hsien Yen 1,2,7,8 and Shun-Jen Chang 9,* 1 Graduate Institute of Clinical Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung 80708, Taiwan; [email protected] (C.-C.T.); [email protected] (J.-H.Y.) 2 Division of Rheumatology, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung 80756, Taiwan 3 Department of Biotechnology, College of Life Science, Kaohsiung Medical University, Kaohsiung 80708, Taiwan; [email protected] 4 Department of Medical Research, Kaohsiung Medical University Hospital, Kaohsiung 80756, Taiwan 5 Department of Internal Medicine, Kaohsiung Municipal Ta-Tung Hospital, Kaohsiung 80145, Taiwan; [email protected] 6 Laboratory Diagnosis of Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung 80708, Taiwan; [email protected] 7 Institute of Biomedical Sciences, National Sun Yat-Sen University, Kaohsiung 80424, Taiwan 8 Department of Biological Science and Technology, National Chiao-Tung University, Hsinchu 30010, Taiwan 9 Department of Kinesiology, Health and Leisure Studies, National University of Kaohsiung, Kaohsiung 81148, Taiwan * Correspondence: [email protected] (W.-T.L.); [email protected] (S.-J.C.); Tel.: +886-7-3121101 (W.-T.L.); +886-7-5916679 (S.-J.C.); Fax: +886-7-3125339 (W.-T.L.); +886-7-5919264 (S.-J.C.) Received: 19 May 2020; Accepted: 29 June 2020; Published: 1 July 2020 Abstract: Current knowledge of gout centers on hyperuricemia. -

Hereditary Spastic Paraplegia: from Genes, Cells and Networks to Novel Pathways for Drug Discovery
brain sciences Review Hereditary Spastic Paraplegia: From Genes, Cells and Networks to Novel Pathways for Drug Discovery Alan Mackay-Sim Griffith Institute for Drug Discovery, Griffith University, Brisbane, QLD 4111, Australia; a.mackay-sim@griffith.edu.au Abstract: Hereditary spastic paraplegia (HSP) is a diverse group of Mendelian genetic disorders affect- ing the upper motor neurons, specifically degeneration of their distal axons in the corticospinal tract. Currently, there are 80 genes or genomic loci (genomic regions for which the causative gene has not been identified) associated with HSP diagnosis. HSP is therefore genetically very heterogeneous. Finding treatments for the HSPs is a daunting task: a rare disease made rarer by so many causative genes and many potential mutations in those genes in individual patients. Personalized medicine through genetic correction may be possible, but impractical as a generalized treatment strategy. The ideal treatments would be small molecules that are effective for people with different causative mutations. This requires identification of disease-associated cell dysfunctions shared across geno- types despite the large number of HSP genes that suggest a wide diversity of molecular and cellular mechanisms. This review highlights the shared dysfunctional phenotypes in patient-derived cells from patients with different causative mutations and uses bioinformatic analyses of the HSP genes to identify novel cell functions as potential targets for future drug treatments for multiple genotypes. Keywords: neurodegeneration; motor neuron disease; spastic paraplegia; endoplasmic reticulum; Citation: Mackay-Sim, A. Hereditary protein-protein interaction network Spastic Paraplegia: From Genes, Cells and Networks to Novel Pathways for Drug Discovery. Brain Sci. 2021, 11, 403. -

Human Social Genomics in the Multi-Ethnic Study of Atherosclerosis
Getting “Under the Skin”: Human Social Genomics in the Multi-Ethnic Study of Atherosclerosis by Kristen Monét Brown A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Epidemiological Science) in the University of Michigan 2017 Doctoral Committee: Professor Ana V. Diez-Roux, Co-Chair, Drexel University Professor Sharon R. Kardia, Co-Chair Professor Bhramar Mukherjee Assistant Professor Belinda Needham Assistant Professor Jennifer A. Smith © Kristen Monét Brown, 2017 [email protected] ORCID iD: 0000-0002-9955-0568 Dedication I dedicate this dissertation to my grandmother, Gertrude Delores Hampton. Nanny, no one wanted to see me become “Dr. Brown” more than you. I know that you are standing over the bannister of heaven smiling and beaming with pride. I love you more than my words could ever fully express. ii Acknowledgements First, I give honor to God, who is the head of my life. Truly, without Him, none of this would be possible. Countless times throughout this doctoral journey I have relied my favorite scripture, “And we know that all things work together for good, to them that love God, to them who are called according to His purpose (Romans 8:28).” Secondly, I acknowledge my parents, James and Marilyn Brown. From an early age, you two instilled in me the value of education and have been my biggest cheerleaders throughout my entire life. I thank you for your unconditional love, encouragement, sacrifices, and support. I would not be here today without you. I truly thank God that out of the all of the people in the world that He could have chosen to be my parents, that He chose the two of you. -

UBAP1 (NM 016525) Human Recombinant Protein Product Data
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for TP301858 UBAP1 (NM_016525) Human Recombinant Protein Product data: Product Type: Recombinant Proteins Description: Recombinant protein of human ubiquitin associated protein 1 (UBAP1) Species: Human Expression Host: HEK293T Tag: C-Myc/DDK Predicted MW: 54.9 kDa Concentration: >50 ug/mL as determined by microplate BCA method Purity: > 80% as determined by SDS-PAGE and Coomassie blue staining Buffer: 25 mM Tris.HCl, pH 7.3, 100 mM glycine, 10% glycerol Preparation: Recombinant protein was captured through anti-DDK affinity column followed by conventional chromatography steps. Storage: Store at -80°C. Stability: Stable for 12 months from the date of receipt of the product under proper storage and handling conditions. Avoid repeated freeze-thaw cycles. RefSeq: NP_057609 Locus ID: 51271 UniProt ID: Q9NZ09 RefSeq Size: 2743 Cytogenetics: 9p13.3 RefSeq ORF: 1506 Synonyms: NAG20; SPG80; UAP; UBAP; UBAP-1 This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 2 UBAP1 (NM_016525) Human Recombinant Protein – TP301858 Summary: This gene is a member of the UBA domain family, whose members include proteins having connections to ubiquitin and the ubiquitination pathway. The ubiquitin associated domain is thought to be a non-covalent ubiquitin binding domain consisting of a compact three helix bundle. This particular protein originates from a gene locus in a refined region on chromosome 9 undergoing loss of heterozygosity in nasopharyngeal carcinoma (NPC). -

A Genome-Wide Scan of Cleft Lip Triads Identifies Parent
F1000Research 2019, 8:960 Last updated: 03 AUG 2021 RESEARCH ARTICLE A genome-wide scan of cleft lip triads identifies parent- of-origin interaction effects between ANK3 and maternal smoking, and between ARHGEF10 and alcohol consumption [version 2; peer review: 2 approved] Øystein Ariansen Haaland 1, Julia Romanowska1,2, Miriam Gjerdevik1,3, Rolv Terje Lie1,4, Håkon Kristian Gjessing 1,4, Astanand Jugessur1,3,4 1Department of Global Public Health and Primary Care, University of Bergen, Bergen, N-5020, Norway 2Computational Biology Unit, University of Bergen, Bergen, N-5020, Norway 3Department of Genetics and Bioinformatics, Norwegian Institute of Public Health, Skøyen, Oslo, Skøyen, N-0213, Norway 4Centre for Fertility and Health (CeFH), Norwegian Institute of Public Health, Skøyen, Oslo, N-0213, Norway v2 First published: 24 Jun 2019, 8:960 Open Peer Review https://doi.org/10.12688/f1000research.19571.1 Latest published: 19 Jul 2019, 8:960 https://doi.org/10.12688/f1000research.19571.2 Reviewer Status Invited Reviewers Abstract Background: Although both genetic and environmental factors have 1 2 been reported to influence the risk of isolated cleft lip with or without cleft palate (CL/P), the exact mechanisms behind CL/P are still largely version 2 unaccounted for. We recently developed new methods to identify (revision) report parent-of-origin (PoO) interactions with environmental exposures 19 Jul 2019 (PoOxE) and now apply them to data from a genome-wide association study (GWAS) of families with children born with isolated CL/P. version 1 Methods: Genotypes from 1594 complete triads and 314 dyads (1908 24 Jun 2019 report report nuclear families in total) with CL/P were available for the current analyses. -

Mouse Ubap1 Conditional Knockout Project (CRISPR/Cas9)
https://www.alphaknockout.com Mouse Ubap1 Conditional Knockout Project (CRISPR/Cas9) Objective: To create a Ubap1 conditional knockout Mouse model (C57BL/6J) by CRISPR/Cas-mediated genome engineering. Strategy summary: The Ubap1 gene (NCBI Reference Sequence: NM_023305 ; Ensembl: ENSMUSG00000028437 ) is located on Mouse chromosome 4. 7 exons are identified, with the ATG start codon in exon 2 and the TGA stop codon in exon 7 (Transcript: ENSMUST00000072866). Exon 3 will be selected as conditional knockout region (cKO region). Deletion of this region should result in the loss of function of the Mouse Ubap1 gene. To engineer the targeting vector, homologous arms and cKO region will be generated by PCR using BAC clone RP23-324H18 as template. Cas9, gRNA and targeting vector will be co-injected into fertilized eggs for cKO Mouse production. The pups will be genotyped by PCR followed by sequencing analysis. Note: Exon 3 starts from about 2.32% of the coding region. The knockout of Exon 3 will result in frameshift of the gene. The size of intron 2 for 5'-loxP site insertion: 4794 bp, and the size of intron 3 for 3'-loxP site insertion: 7097 bp. The size of effective cKO region: ~625 bp. The cKO region does not have any other known gene. Page 1 of 7 https://www.alphaknockout.com Overview of the Targeting Strategy Wildtype allele gRNA region 5' gRNA region 3' 1 3 7 Targeting vector Targeted allele Constitutive KO allele (After Cre recombination) Legends Exon of mouse Ubap1 Homology arm cKO region loxP site Page 2 of 7 https://www.alphaknockout.com Overview of the Dot Plot Window size: 10 bp Forward Reverse Complement Sequence 12 Note: The sequence of homologous arms and cKO region is aligned with itself to determine if there are tandem repeats. -
The Novel ALG-2 Target Protein CDIP1 Promotes Cell Death by Interacting with ESCRT-I and VAPA/B
International Journal of Molecular Sciences Article The Novel ALG-2 Target Protein CDIP1 Promotes Cell Death by Interacting with ESCRT-I and VAPA/B Ryuta Inukai 1, Kanako Mori 1, Keiko Kuwata 2, Chihiro Suzuki 1, Masatoshi Maki 1, Terunao Takahara 1 and Hideki Shibata 1,* 1 Department of Applied Biosciences, Graduate School of Bioagricultural Sciences, Nagoya University, Furo-cho, Chikusa-ku, Nagoya 464-8601, Japan; [email protected] (R.I.); [email protected] (K.M.); [email protected] (C.S.); [email protected] (M.M.); [email protected] (T.T.) 2 Institute of Transformative Bio-Molecules (WPI-ITbM), Nagoya University, Furo-cho, Chikusa-ku, Nagoya 464-8601, Japan; [email protected] * Correspondence: [email protected] Abstract: Apoptosis-linked gene 2 (ALG-2, also known as PDCD6) is a member of the penta-EF-hand (PEF) family of Ca2+-binding proteins. The murine gene encoding ALG-2 was originally reported to be an essential gene for apoptosis. However, the role of ALG-2 in cell death pathways has remained elusive. In the present study, we found that cell death-inducing p53 target protein 1 (CDIP1), a pro-apoptotic protein, interacts with ALG-2 in a Ca2+-dependent manner. Co-immunoprecipitation analysis of GFP-fused CDIP1 (GFP-CDIP1) revealed that GFP-CDIP1 associates with tumor suscep- tibility gene 101 (TSG101), a known target of ALG-2 and a subunit of endosomal sorting complex required for transport-I (ESCRT-I). ESCRT-I is a heterotetrameric complex composed of TSG101, VPS28, VPS37 and MVB12/UBAP1. -

UBAP1 Is a Component of an Endosome-Specific ESCRT
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Current Biology 21, 1245–1250, July 26, 2011 ª2011 Elsevier Ltd All rights reserved DOI 10.1016/j.cub.2011.06.028 Report UBAP1 Is a Component of an Endosome-Specific ESCRT-I Complex that Is Essential for MVB Sorting Flavia Stefani,1 Ling Zhang,1 Sandra Taylor,1 degeneration (FTLD) [15]. All clones contained a central region Johanna Donovan,1,3 Sara Rollinson,2 Aurelie Doyotte,1 (aa 159–308) of UBAP1. Directed yeast two-hybrid analysis Kim Brownhill,1 Janis Bennion,2 Stuart Pickering-Brown,2 showed that full-length UBAP1 interacted with the Bro-V and Philip Woodman1,* region of HDPTP, but not Alix, and with full-length HDPTP (Fig- 1Faculty of Life Sciences ure 1B; see also Figure S1A available online). 2Faculty of Human and Medical Sciences The UBAP1 binding region is confined to the putative V University of Manchester, Manchester M13 9PT, UK domain of HDPTP (Figure 1B; Figure S1A). Alix V domain contains a conserved pocket that binds a YPXnL motif within the late domain of HIV [3, 13]. One amino acid that is essential Summary for viral binding is F676, and a corresponding residue, F678, is found in HDPTP. A F678D mutation abolished HDPTP binding Endosomal sorting complexes required for transport to UBAP1 (Figure 1B; Figure S1A), but not to other interactors (ESCRTs) regulate several events involving membrane (data not shown). To assess the importance of F678 for HDPTP invagination, including multivesicular body (MVB) biogen- function, we treated cells with small interfering RNA (siRNA) esis, viral budding, and cytokinesis [1].