Efficacy of a Novel Thoracopelvic Orthosis in Reducing Lumbar Spine Loading and Muscle Fatigue in Flexion: a Study with Weighted Garments
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

UC Santa Cruz Other Recent Work
UC Santa Cruz Other Recent Work Title Teaching is New Every Day: An Oral History of Science Illustration Teacher-Administrators Jenny Keller and Ann Caudle Permalink https://escholarship.org/uc/item/47v1f16m Authors Reti, Irene H. Keller, Jenny Caudle, Ann Publication Date 2018-01-17 eScholarship.org Powered by the California Digital Library University of California Teaching Is New Every Day: An Oral History of Science Illustration Teacher-Administrators Jenny Keller and Ann Caudle Interviewed by Sarah Rabkin Edited by Sarah Rabkin and Irene Reti Santa Cruz University of California, Santa Cruz University Library 2018 This oral history is covered by copyright agreements between Jennifer Keller dated December 1, 2017; and Ann Caudle, dated December 5, 2017, and the Regents of the University of California. Under “fair use” standards, excerpts of up to six hundred words (per interview) may be quoted without the University Library’s permission as long as the materials are properly cited. Quotations of more than six hundred words require the written permission of the Head of Special Collections and Archives and a proper citation and may also require a fee. Under certain circumstances, not-for-profit users may be granted a waiver of the fee. For permission contact: Irene Reti [email protected] or Regional History Project, McHenry Library, UC Santa Cruz, 1156 High Street, Santa Cruz, CA, 95064. Phone: 831-459-2847. Jenny Keller (R) with Science Illustration students Natalie Renier (L) and Lindsey Kernodle (R). Courtesy: Science Illustration Program. -

Stargate | Oddity Central - Collecting Oddities
Stargate | Oddity Central - Collecting Oddities http://www.odditycentral.com/tag/stargate Home About Advertise Contact Contribute Disclaimer Privacy policy Search for: Pics News Videos Travel Tech Animals Funny Foods Auto Art Events WTF Architecture Home Father And Son Build Awesome Backyard Stargate By Spooky onJune 16th, 2010 Category: Pics , Tech Comments Off Back in 2005, when Stargate was the coolest sci-fi series around, sg1archive user ‘mango’ teamed up with his father to build a sweet replica of the stargate . 2 The project began in AUTOCAD, where the first blueprints were drawn. Since they didn’t have access to a plotter, plans had to be printed on A4 paper and stuck together, in a circle. The small details of the gate had to Tweet be drawn up from scratch, using photos and video footage. The skeleton of the gate is made up of 18 X-shaped pieces, and the spinning part is made from small planks. 89 The intricate stargate symbols had to be painstakingly carved, from wood, and chevrons first had to be carved from Styrofoam. The back of the stargate, though painted in gray, is totally fake, but the front looks realistic enough, with chevrons locking and everything. Thanks to an inner track, it even spins. Mango wasn’t too satisfied with the paint-job, but all in all this is a geeky masterpiece, just like the Stargate Share home-cinema . Be sure to check the video Mango made, at the bottom of the post. .. Subscribe via Rss Via Email Follow our Tweets on Twitter! 1 of 3 7/11/2012 9:54 PM Stargate | Oddity Central - Collecting Oddities http://www.odditycentral.com/tag/stargate Oddity Central on Facebook Like 8,667 people like Oddity Central . -
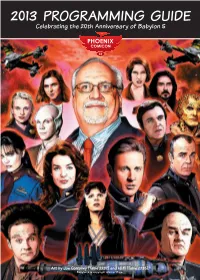
2013 PROGRAMMING GUIDE Celebrating the 20Th Anniversary of Babylon 5
2013 PROGRAMMING GUIDE Celebrating the 20th Anniversary of Babylon 5 Art by Joe Corroney (Table 2237) and Hi Fi (Table 2235). Babylon 5 is copyright Warner Bros. 2 PHOENIX COMICON 2013 • PROGRAMMING GUIDE • PHOENIXCOMICON.COM PHOENIX COMICON 2013 • PROGRAMMING GUIDE • PHOENIXCOMICON.COM 3 TABLE OF CONTENTS Hyatt Regency Map .....................................................6 Renaissance Map ...........................................................7 Exhibitor Hall Map .................................................. 8–9 Programming Rooms ........................................... 10–11 Phoenix Comicon Convention Policies .............12 Exhibitor & Artist Alley Locations .............14-15 Welcome to Phoenix Comicon, Guest Locations...........................................................16 Guest Bios .............................................................. 18–22 the signature pop-culture event of Programming Schedule ................................. 24–35 the southwest! Gaming Schedule ..............................................36–42 If you are new to us, or have never been to a “comicon” before, we welcome you. Programming Descriptions.........................44–70 This weekend is the culmination of efforts by over seven hundred volunteers over the past twelve months all with a singular vision of putting on the most fun convention you’ll attend. Festivities kick off Thursday afternoon and continue throughout the weekend. Spend the day checking out the exhibitor hall, meeting actors and writers, buying that hard to -

Major Samantha Carter
Richard Dean Anderson A1 Autograph Card as Colonel Jack O'Neill C3 Costume Card Major Samantha Carter Teal'c I SketchaFEX Stargate SG-1 season 4 Teal'c II SketchaFEX Stargate SG-1 season 4 Michael Shanks and DA1 Autograph Card Amanda Tapping Relic Card of 60's Style R9 Relic Card Poster from "1969" G2 Kneel Before Your God Apophis A67 Autograph Card Claudia Black as Vala A70 Autograph Card Richard Dean Anderson A73 Autograph Card Isaac Hayes as Tolok Dan Castellaneta as Joe A76 Autograph Card Spencer Christopher Judge as DA2 Autograph Card Teal'c and Tony Amendola as Bra'tac Claudia Black as Vala and DA3 Autograph Card Michael Shanks as Dr. Daniel Jackson Ben Browder as Lt. Col. A85 Autograph Card Cameron Mitchell Michael Shanks and Ben DA4 Autograph Card Browder PC1 Stargate Patch Cards Colonel Jack O'Neill PC2 Stargate Patch Cards Dr. Daniel Jackson Lt. Colonel Samantha PC4 Stargate Patch Cards Carter Claudia Black as Vala A108 Autograph Card Mal Doran A96 Autograph Card Rene Auberjonois as Alar Amanda Tapping as Autograph Card Samantha Christopher Judge as Autograph Card Teal'c C56 Costume Card President Landry Beau Bridges as Major A86 Autograph Card General Hank Landry David Hewlett as Dr. Autograph Card Rodney McKay David Hewlett as Dr. Autograph Card Rodney McKay Amanda Tapping as Autograph Card Major Carter Jason Momoa as Ronon Autograph Card Dex Vala Mal Dual Costume Card Stargate Heroes Doran Samantha Dual Costume Card Stargate Heroes Carter Michael Shanks as Dr. Jackson - Autographed Costume Card Beau Bridges as Major General Hank Landry - Autographed Costume Card Amanda Tapping as Major Carter - Autographed Costume Card Richard Dean Anderson - Autographed Costume Card R75 Bug Prop Card Stargate SG-1 Season 5 SketchaFEX Checklist 3. -

2016 Abstracts 05-19-16 Pk
MID-AMERICA ORTHOPAEDIC ASSOCIATION 34th Annual Meeting April 13-17, 2016 Hyatt Regency Coconut Point Resort Bonita Springs, FL Podium and Poster Abstracts NOTE: Disclosure information is listed at the end of this document. *Denotes presenter MAOA FIRST PLENARY SESSION April 14, 2016 Liposomal Bupivacaine vs. Femoral Nerve Block in Managing Pain After Anterior Cruciate Ligament Reconstruction Abstract ID: Paper 001 ____________________________________________________________________________ Kelechi R. Okoroha, M.D. Robert A. Keller, M.D. Edward Jung, M.D. Nima Mehran, M.D., M.S. *Eric T. Owashi, M.D. Vasilios Moutzouros, M.D. Detroit, MI INTRODUCTION: Adequate postoperative pain management following arthroscopic anterior cruciate ligament (ACL) reconstruction is essential to hasten rehabilitation and improve patient satisfaction. Currently, the gold standard for pain management after knee surgery is femoral nerve block (FNB); however, recent trials have demonstrated reasonable postoperative pain control with locally infiltrated Liposomal Bupivacaine. No clinical studies have examined the effectiveness of Liposomal Bupivacaine at pain control following ACL reconstructions. The aim of this study was to compare the effectiveness of Liposomal Bupivacaine to FNB in controlling post-ACL reconstruction pain. METHODS: This study was a prospective, randomized clinical trial. One hundred patients surgically treated for primary ACL tears were consented for participation. Patients were randomized to receive either intraoperative local infiltration of Liposomal Bupivacaine (20 cc Bupivacaine/10 cc saline) using a standardized injection protocol or preoperative FNB. Following surgery, patient’s pain and opioid consumption was recorded using a Visual Analog Scale (VAS) and IV morphine equivalents for four days. The primary outcome of interest was postoperative pain levels. -

Stargate Atlantis Season 5 Watch Onl
Stargate atlantis season 5 watch onl Continue Go to the main content - (192)IMDb 8.02008X-Ray 01 January 200844minAudio Languages01 January 200844minAudio Languages01 January 200843minAudio Languages 4. Variations of Daedalus 01 January 200844minAudio Languages 5. Ghost in the Machine 01 January 200844minAudio Languages01 January 200844minAudio Languages01 January 200844minAudio Languages01 January 200844minAu dio languages 01 January 200844minAudio Languages01 January 200843minAudio Languages01 January 200844minAudio Languages01 January 200844minAudio Languages0 1 January 200843minAudio Languages01 January 200843minAudio Languages01 January 200844minAudio Languages01 January 200844minAudio Languages01 January 2000844minAudio Languages01 January 200844minAudio Languages01 January 200844minAudio Languages01 January 200843minAudio Languages M Moderate Topics, Moderate Violence, Infrequent moderate rough languageAtlantis race on time to rescue team members trapped in the collapsed compound, and rescue pregnant Teyla from Michael's clutches. M Moderate Themes, Moderate Violence, Rare Moderate Rough LanguageWhy a mysterious alien organism takes Dr. Keller as host, Beckett and the team are desperately looking for a serum to save her from a developing intruder before he can infiltrate Atlantis.M Moderate themes, Moderate violence, a rare moderate rude languageRonon captured by his former friend, Tyre, and flipped over on the ghost. As the team fights for leads, Ronon goes through an agonizing ordeal. M Moderate themes, Moderate Violence, Infrequent Moderates Rough LanguageA Drive Malfunction aboard the mysterious duplicate Daedalus sends a team jumping through various alternate realities where they encounter sinister alien life forms, searing sun, and smashed space battle for Atlantis.M Moderate themes, moderate violence, moderately rare crude language Mysterious essence causes crippling chaos in the city's computer systems. M Moderate themes, Moderate Violence, Rare Moderate Rough Language While on a rescue mission to another planet, Dr. -

Issue 1, 2015 This Is an Advertisement
Strive Issue 1, 2015 This is an advertisement. Q&A with Jennifer Keller Amy Mahone He immediately encouraged me to do so, 423.209.4183 indicating that Jennifer is an absolute star. He [email protected] told me then that Jennifer has a wonderful Table of Contents understanding of people and the ability to be Q&A with Jennifer tough but fair and, through all of her actions, Keller extraordinarily kind. When I did meet and start In January, Baker Donelson’s CEO, Ben Adams, working with Jennifer, I could see instantly what Time Saver Savvy announced that Jennifer Keller, a shareholder in all of the fuss was about. Jennifer is a natural leader the Johnson City, Tennessee, office, would become and her style is both very thoughtful and also On My Bookshelf the Firm’s next President and Chief Operating practical. Officer effective April 1, 2015. Women’s Health Tips As our readers are well aware, having a woman in Jennifer has been with Baker Donelson for 20 one of the highest levels of leadership at a firm of Parental Leave Policy years – her entire legal career – practicing in the more than 650 attorneys is a big deal, because Labor and Employment Group and serving as despite the fact that half of associates in law firms New Faces at the Firm the L&E Department Chair for the last six years. are female, only about 20 percent of equity Attorneys in that group cannot say enough about partners in firms are female and only a handful Baker Donelson Women Jennifer’s leadership and have expressed that, of “Big Law” firms have a woman in the C-suite. -

Reinventing Business Through Disruptive
REINVENTING BUSINESS THROUGH DISRUPTIVE TECHNOLOGIES Sector Trends and Investment Opportunities for Firms in Emerging Markets FURTHER READING Additional reports about the role of technology in emerging markets, as well as a list of EM Compass Notes published by IFC Thought Leadership: ifc.org/thoughtleadership Blockchain: Opportunities for Private Enterprises in Emerging Markets | January 2019 How Technology Creates Markets – Trends and Examples for Private Investors in Emerging Markets | April 2018 See pages 106–108 for more details. About IFC IFC—a sister organization of the World Bank and member of the World Bank Group—is the largest global development institution focused on the private sector in emerging markets. We work with more than 2,000 businesses worldwide, using our capital, expertise, and influence to create markets and opportunities in the toughest areas of the world. In fiscal year 2018, we delivered more than $23 billion in long-term financing for developing countries, leveraging the power of the private sector to end extreme poverty and boost shared prosperity. For more information, visit www.ifc.org. © International Finance Corporation 2019. All rights reserved. 2121 Pennsylvania Avenue, N.W. Washington, D.C. 20433 www.ifc.org The material in this work is copyrighted. Copying and/or transmitting portions or all of this work without permission may be a violation of applicable law. IFC does not guarantee the accuracy, reliability or completeness of the content included in this work, or for the conclusions or judgments described herein, and accepts no responsibility or liability for any omissions or errors (including, without limitation, typographical errors and technical errors) in the content whatsoever or for reliance thereon. -

Director), Jennifer Keller (Member at Large), Tom Krieger (Member at Large), Nancy Berry, Colin Chesley, Annie Howard, Sharyon Mckinney, Dr
Coalition For Kids Board of Directors Meeting Minutes December 3rd, 2018 Directors present: Cay Greer (President), Jim Harlan (Treasurer), Maggie Ingram (Secretary), Randy Hensley (Executive Director), Jennifer Keller (Member at Large), Tom Krieger (Member at Large), Nancy Berry, Colin Chesley, Annie Howard, Sharyon McKinney, Dr. Wendy Nehring, Kevin Peters, Harrison Wexler, Sheila Whitlock and Bethany Patton (Director of Operations). Call to Order, Opening Prayer and Welcome Cay Greer opened the meeting in prayer, then welcomed the Board of Directors and the new Board Members Annie Howard and Kevin Peters. Kevin Peters is from Elizabethton, he works as a CPA for Blackburn Childress & Stigall. Kevin is also on the board for the Ronald McDonald House. He is looking forward to serving on the Coalition’s Board of Directors. Annie Howard is from Elk Park, North Carolina. She currently is a health care attorney with Hancock Daniel. Annie is excited to be a part of Coalition’s Board of Directors. Approval of minutes (PowerPoint included at end of minutes) Cay Greer presented the October board minutes, it was noted for the PowerPoint presentation to be included in the minutes from this meeting forward and add a summary of the PowerPoint. Maggie Ingram made a motion to approve the October minutes as presented and Harrison Wexler seconded the motion; approved as presented. Finance Report (see handout for report details) Jim Harlan Jim reports current assets are in good shape. The November income is up 3K compared to the budgeted November income with the November expenses slightly over the budgeted expenses. The YTD income is only about 3K below budgeted YTD income; therefore compared to budget we are flat. -

“ Where Words Fail, Music Speaks.”
WINONA HEALTH FOUNDATION | FALL 2017 Generosity Inspires “ Where words fail, music speaks.” — Hans Christian Andersen Charitable donations bring music to hospice patients Story on page 2. Generosity Inspires from Betsy Midthun Vice President of Community Engagement Generosity is powerful stuff You bring a casserole to a neighbor who Inspires newsletter, sharing stories of is mourning. You drive an elderly friend charity and kindness. In the past year, to a doctor’s appointment. You volunteer your generosity has provided over $1.3 at the food shelf. When you demonstrate million to our patients, residents and generosity, you help others before employees in need through the Winona yourself. Health Foundation. Give a little, help a This is the second edition of our new lot. Generosity is powerful stuff. Winona Health Foundation Generosity November is Hospice Month Have harp, will travel... Bringing peace, comfort and joy for life’s journey Sister Mary Jo Baldus, RSM, RMT, Mary Jo always plays live music. She brings music to the bedsides of local is familiar with a lot of older songs, as hospice patients. She describes music as well as church music, but she says with a tool that helps people today’s technology, she can to relax, review their find nearly any music online, life, and even get in complete with lyrics and touch with long-buried chords. She has had patients memories. The process who love country music, old- begins when Music time music, David Bowie, Therapy Services of Journey and the Moody Winona, Mary Jo’s Blues. With the help of business, receives a Google, she can meet nearly referral from a hospice any request. -

Bromance” Trope in Contemporary Film and Television
THIS FAR, BUT NO FURTHER: QUESTIONING THE “BROMANCE” TROPE IN CONTEMPORARY FILM AND TELEVISION ROBYN JOFFE A THESIS SUBMITTED TO THE FACULTY OF GRADUATE STUDIES IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF ARTS GRADUATE PROGRAM IN COMMUNICATION AND CULTURE YORK UNIVERSITY TORONTO, ONTARIO April 2020 © Robyn Joffe, 2020 ii ABSTRACT In traditionally male-oriented genres of contemporary film and television, the bromance is a relationship that outwardly suggests an acceptance of homosexuality, but is instead actually dependent upon both men being heterosexual; the closeness between these male characters is played for laughs, and no one seriously considers the possibility that the relationship may become romantic. This problem is compounded by the recent popularity of queerbaiting audiences, both within the actual narratives and by those working behind the scenes. I use post- structuralist textual analysis and interviews, as well as the practice of seeing queerly, to examine how bromance relationships are constructed and represented onscreen in the Buddy Cop, Science Fiction and Fantasy, and Superhero genres, and the effects of those representations on society. Media creators have the power to affect cultural change, but only if they stop using the idea that someone might be gay as a punchline. iii DEDICATION This thesis is dedicated to my mother, Shelley Joffe Weinstein, for supporting me in every possible way throughout this entire process. I would, literally, not be here without you. iv ACKNOWLEDGMENTS I wish to extend my utmost gratitude to my supervisor, Dr. John McCullough, and my committee members, Dr. Jennifer Burwell and Dr. Mark Hayward, for all of their support and encouragement of myself and my work over the past few years. -

STARGATE ATLANTIS Personajes Principales
Trading Cards Collection The Force Books con la colaboración especial de COLECCIÓN DE CROMOS ESTILO PUERTA ESTELAR Álbum único y The Force Books presentan Trading Cards Collection COLECCIÓN DE CROMOS ESTILO PUERTA ESTELAR Álbum único The Force Books STARGATE Trading Cards Collection © de la presente edición: © THE FORCE BOOKS www.theforcebooks.com Puedes seguirnos en: Facebook: theforcebooks Instagram: theforcebooks © STARGATE LEGEND © ROSA CARRIÓN NAVARRO © NATAN FERNÁNDEZ CHULIÁ The Force Group (Elena Sabidó, Alberto López Calvo, Robert Martex (DEP) y Jose Gracia) Diseño gráfico: Jose Gracia Corrección: Rosa Carrión Navarro Archivo y material gráfico de la obra propiedad de: Stargate Legends. Asesoramiento informático: Antonio Collado Material gratuito para descarga / Made in Spain Primera edición: Mayo 2020 Información STARGATE LEGEND: stargatelegend.com Facebook: @StargateLegendOfficial Instagram:@stargate_legend Twitter: @StargateLegend Todas las imágenes tienen el © de sus respectivos propietarios y/o licenciatarios, y se han usado en su contenido de forma histórica. Los derechos están reservados a quien se lo descargue. Se puede reproducir parte de esta obra o toda completa en cualquier sistema de reproducción, puedes compartirla, regalarla, de forma digital o fotocopias o imprimírtela de la manera que te plazca, con nuestro permiso editorial y de los autores o sin él. Este producto es totalmente gratuito y lo puedes disfrutar como quieras. De hecho nosotros hemos disfrutado haciéndolo y servirá como un pasatiempo más en estos tiempos en los que nos tenemos que quedar confinados en nuestros hogares. Así que haznos caso y.... #QUÉDATE_EN_CASA 02 STARGATE 1994 Personajes principales 0A 0B 0C Coronel Jack O’Neill (Kurt Russel) Dr. Daniel Jackson (James Spader) Dra.