Musculoskeletal Condition Mimicking Spinal Disorder: Lower Extremity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Juvenile Spondyloarthropathies: Inflammation in Disguise
PP.qxd:06/15-2 Ped Perspectives 7/25/08 10:49 AM Page 2 APEDIATRIC Volume 17, Number 2 2008 Juvenile Spondyloarthropathieserspective Inflammation in DisguiseP by Evren Akin, M.D. The spondyloarthropathies are a group of inflammatory conditions that involve the spine (sacroiliitis and spondylitis), joints (asymmetric peripheral Case Study arthropathy) and tendons (enthesopathy). The clinical subsets of spondyloarthropathies constitute a wide spectrum, including: • Ankylosing spondylitis What does spondyloarthropathy • Psoriatic arthritis look like in a child? • Reactive arthritis • Inflammatory bowel disease associated with arthritis A 12-year-old boy is actively involved in sports. • Undifferentiated sacroiliitis When his right toe starts to hurt, overuse injury is Depending on the subtype, extra-articular manifestations might involve the eyes, thought to be the cause. The right toe eventually skin, lungs, gastrointestinal tract and heart. The most commonly accepted swells up, and he is referred to a rheumatologist to classification criteria for spondyloarthropathies are from the European evaluate for possible gout. Over the next few Spondyloarthropathy Study Group (ESSG). See Table 1. weeks, his right knee begins hurting as well. At the rheumatologist’s office, arthritis of the right second The juvenile spondyloarthropathies — which are the focus of this article — toe and the right knee is noted. Family history is might be defined as any spondyloarthropathy subtype that is diagnosed before remarkable for back stiffness in the father, which is age 17. It should be noted, however, that adult and juvenile spondyloar- reported as “due to sports participation.” thropathies exist on a continuum. In other words, many children diagnosed with a type of juvenile spondyloarthropathy will eventually fulfill criteria for Antinuclear antibody (ANA) and rheumatoid factor adult spondyloarthropathy. -

The Painful Heel Comparative Study in Rheumatoid Arthritis, Ankylosing Spondylitis, Reiter's Syndrome, and Generalized Osteoarthrosis
Ann Rheum Dis: first published as 10.1136/ard.36.4.343 on 1 August 1977. Downloaded from Annals of the Rheumatic Diseases, 1977, 36, 343-348 The painful heel Comparative study in rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthrosis J. C. GERSTER, T. L. VISCHER, A. BENNANI, AND G. H. FALLET From the Department of Medicine, Division of Rheumatology, University Hospital, Geneva, Switzerland SUMMARY This study presents the frequency of severe and mild talalgias in unselected, consecutive patients with rheumatoid arthritis, ankylosing spondylitis, Reiter's syndrome, and generalized osteoarthosis. Achilles tendinitis and plantar fasciitis caused a severe talalgia and they were observed mainly in males with Reiter's syndrome or ankylosing spondylitis. On the other hand, sub-Achilles bursitis more frequently affected women with rheumatoid arthritis and rarely gave rise to severe talalgias. The simple calcaneal spur was associated with generalized osteoarthrosis and its frequency increased with age. This condition was not related to talalgias. Finally, clinical and radiological involvement of the subtalar and midtarsal joints were observed mainly in rheumatoid arthritis and occasionally caused apes valgoplanus. copyright. A 'painful heel' syndrome occurs at times in patients psoriasis, urethritis, conjunctivitis, or enterocolitis. with inflammatory rheumatic disease or osteo- The antigen HLA B27 was present in 29 patients arthrosis, causing significant clinical problems. Very (80%O). few studies have investigated the frequency and characteristics of this syndrome. Therefore we have RS 16 PATIENTS studied unselected groups of patients with rheuma- All of our patients had the complete triad (non- toid arthritis (RA), ankylosing spondylitis (AS), gonococcal urethritis, arthritis, and conjunctivitis). -

Shoulder Pain – Complexity to Simplicity
Shoulder Pain – Complexity to Simplicity A Regional Approach to Shoulder Pain The best way to approach a problem of shoulder pain is to look at the pain from a regional point of view. This allows for easy identification of specific pathological problems that occur at each region. In this talk, we look at the patterns of pain that occur with the different regions around the shoulder. From this, we will focus on the pathological problems that can be expected in each region and then look at specific physical examination findings that can be used to confirm a diagnosis or help further clarify the problem. Although this talk is focused on the diagnosis of causes of shoulder pain, we also take a look at some updates and salient features of treatment. In general, pain in the region of the shoulder can be grouped into 4 main types. These relate to specific patterns of pain that allow history taking to help us focus on the likely cause(s) before moving on to examination. A fairly clear-cut diagnosis is almost always achievable without the need to resort to special tests to help make the diagnosis. Of course, this does not include all possible causes of pain. The uncommon problem will still need a thorough and complete approach to determining cause, often with the requirement for special investigations. Remember that this is a good guide. Don't neglect other causes of referred pain that may cause pain in and around the shoulder. Included here is cardiac pain, diaphragmatic pain, apical lung disease and malignant bone pain. -

The Pathomechanics of Plantar Fasciitis
Sports Med 2006; 36 (7): 585-611 REVIEW ARTICLE 0112-1642/06/0007-0585/$39.95/0 2006 Adis Data Information BV. All rights reserved. The Pathomechanics of Plantar Fasciitis Scott C. Wearing,1 James E. Smeathers,1 Stephen R. Urry,1 Ewald M. Hennig2 and Andrew P. Hills1 1 Institute of Health and Biomedical Innovation, Queensland University of Technology, Kelvin Grove, Queensland, Australia 2 Biomechanik Labor, University Duisburg-Essen, Essen, Germany Contents Abstract ....................................................................................585 1. Anatomy of the Plantar Fascia ............................................................586 1.1 Gross Anatomy of the Plantar Fascia...................................................586 1.2 Histological Anatomy of the Plantar Fascia .............................................589 1.2.1 Neuroanatomy ................................................................590 1.2.2 Microcirculation ...............................................................590 1.2.3 The Enthesis ...................................................................590 2. Mechanical Properties of the Plantar Fascia ................................................592 2.1 Structural Properties ..................................................................593 2.2 Material Properties ...................................................................593 3. Mechanical Function of the Plantar Fascia .................................................594 3.1 Quasistatic Models of Plantar Fascial Function ..........................................594 -

Piriformis Syndrome Is Overdiagnosed 11 Robert A
American Association of Neuromuscular & Electrodiagnostic Medicine AANEM CROSSFIRE: CONTROVERSIES IN NEUROMUSCULAR AND ELECTRODIAGNOSTIC MEDICINE Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 AANEM COURSE F AANEM 52ND Annual Scientific Meeting Monterey, California CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 COURSE F AANEM 52nd Annual Scientific Meeting Monterey, California AANEM Copyright © September 2005 American Association of Neuromuscular & Electrodiagnostic Medicine 421 First Avenue SW, Suite 300 East Rochester, MN 55902 PRINTED BY JOHNSON PRINTING COMPANY, INC. ii CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Faculty Loren M. Fishman, MD, B.Phil Scott J. Primack, DO Assistant Clinical Professor Co-director Department of Physical Medicine and Rehabilitation Colorado Rehabilitation and Occupational Medicine Columbia College of Physicians and Surgeons Denver, Colorado New York City, New York Dr. Primack completed his residency at the Rehabilitation Institute of Dr. Fishman is a specialist in low back pain and sciatica, electrodiagnosis, Chicago in 1992. He then spent 6 months with Dr. Larry Mack at the functional assessment, and cognitive rehabilitation. Over the last 20 years, University of Washington. Dr. Mack, in conjunction with the Shoulder he has lectured frequently and contributed over 55 publications. His most and Elbow Service at the University of Washington, performed some of the recent work, Relief is in the Stretch: End Back Pain Through Yoga, and the original research utilizing musculoskeletal ultrasound in order to diagnose earlier book, Back Talk, both written with Carol Ardman, were published shoulder pathology. -

Interventional Chronic Pain Treatment in Mature Theaters of Operation
28. INTERVENTIONAL CHRONIC PAIN pain, nonradicular arm pain, groin pain, noncardiac spinal and myofascial pain); and anticonvulsants TREATMENT IN MATURE THEATERS chest pain, and neck pain. The most common diag- and tricyclic antidepressants (usually prescribed for OF OPERATION noses conferred on these patients were lumbosacral radicular and other forms of neuropathic pain). The radiculopathy, recurrence of postsurgical pain, large majority of patients received at least one inter- IMPACT OF NONBATTLE-RELATED INJURIES lumbar facetogenic pain, myofascial pain, neuro- ventional procedure. The most frequently employed AND TREATMENT pathic pain, and lumbar degenerative disc disease. nerve blocks were lumbar transforaminal epidural The most common noninterventional treatments steroid injections (ESIs), trigger point injections, Acute nonbattle injuries (NBIs) and chronic pain have been nonsteroidal antiinflammatory drugs cervical ESIs, lumbar facet blocks, various groin conditions that recur during war have been termed (NSAIDs; > 90%); physical therapy referral (for back blocks, and plantar fascia injections. Table 28-1 lists the “hidden epidemic” by the former surgeon pain, neck pain, and leg pain); muscle relaxants (for procedures for common nerve blocks conducted in general of the US Army, James Peake. Since statistics have been kept, the impact of NBIs on unit readiness TABLE 28-1 has increased. In World War I, NBI was the fourth leading cause of soldier attrition. In World War II PROCEDURES FOR COMMON NERVE BLOCKS CONDUCTED IN THEATER and the Korean conflict, NBIs were the third leading cause of morbidity. By the Vietnam War, NBIs had Injection Injectate Need for Comments become the leading cause of hospital admissions, Volume* (mL) Fluoroscopy? where they have remained ever since. -

Bilateral Calcified Ischiogluteal Bursitis and Shoulder Tendinopathy
Bilateral Calcified Ischiogluteal Bursitis and Conflict of Interest: None Shoulder Tendinopathy: A Case Report declared Seyyed-Mohsen Hosseininejad1,2, Saman Shakeri1, Hossein Mohebbi1, Mehdi Aarabi2, Shiva Momen3 This article has been peer reviewed. 1Shahid Beheshti University of Medical Sciences, Tehran, Iran 2 Golestan University of Medical Sciences, Gorgan, Iran Article Submitted on: 21st 3Mazandaran University of Medical Sciences, Sari, Iran January 2019 Article Accepted on: 1st ABSTRACT June 2020 The ischiogluteal bursitis which is a rare the buttock. Ischiogluteal bursitis Aspiration Funding Sources: None disorder is irregularly found between the showed calcareous deposits; local injection declared gluteus maximus and ischial tuberosity. A of corticosteroid helped the patient to get 41-year-old female with bilateral calcifying free of symptoms. Calcified ischiogluteal Correspondence to: Dr ischiogluteal bursitis and her right shoulder bursitis is a rare condition but simply Seyyed-Mohsen Hosseininejad tendinopathy were presented. She had no diagnosed on x-ray. Local steroid injection related past medical history nor trauma to could provide symptom relief. Address: Shahid Beheshti University of Medical Sciences, Tehran, Iran Keywords: Calcifying Ischiogluteal Bursitis; Aspiration; Treatment; Shoulder pain; Tendinopathy E-mail: Hosseininejad.s.mohsen INTRODUCTION painful swelling in her both buttocks. The patient @gmail.com Ischiogluteal bursitis is a rare condition in which had no related past medical history nor recent Cite this Article: bursa between the gluteus maximus muscle and major trauma. Ischial tuberosities had swelling Hosseininejad SM, ischial tuberosity, which physiologically and tenderness in. Right shoulder had positive Shakeri S, Mohebbi H, decreases the frictional force, develops impingement tests but full range of motion. Aarabi M, Momen S. -

Management of Radicular Pain
Management of Radicular Pain Mel Cusi MBBS, FACSP, FFSEM (UK) Sport & Exercise Medicine Physician Dr Mel Cusi Sport & Exercise Medicine Physician Management of Radicular Pain A. Background B. Epidemiology C. Diagnosis D. Treatment Dr Mel Cusi Sport & Exercise Medicine Physician A. Background • Names and concepts – Radicular pain – Radiculopathy • Structures that can produce radicular Sx – Sinu‐vertebral nerve – Nerve root • Mechanisms of pain – Direct toxic effect of disc material – Chemical substances Dr Mel Cusi Sport & Exercise Medicine Physician B. Epidemiology • Occurs in 3‐5% of the population – More frequent in males in their 40’s – More frequent in females in their 50’s • In sporting population – More frequent in sports that combine spinal flexion/extension with rotation – Fast bowlers, gymnasts, dancers, RU backrowers, golfers, weightlifters, baseball pitchers Dr Mel Cusi Sport & Exercise Medicine Physician C. Diagnosis • Radicular pain is only a descriptive symptom • Diagnosis is made on the usual basis of – History – Clinical examination – Appropriate investigations (when required) Dr Mel Cusi Sport & Exercise Medicine Physician History • Acute LBP radiating to buttock / lower limb • Worse with flexion, sneezing, coughing. Sitting worse than standing • Some pointers – Referred pain from L1‐3 does not reach the knee – Unusual Symptoms (weight loss, fever, chills) point to something else – Beware of cauda equina: surgical emergency Dr Mel Cusi Sport & Exercise Medicine Physician Neurological Examination • Sensation – Subjective -

Endoscopic Hamstring Repair
Lorem Ipsum Endoscopic Hamstring Repair Carlos A. Guanche, MD Southern California Orthopedic Institute 12 Lorem Ipsum 2 Endoscopic Hamstring Repair With the expansion of knowledge regarding hip pathologies as a result of the increased treatment of hip problems arthroscopically has come an expanded treatment of many injuries that were previously treated through open methods. The treatment of symptomatic ischial bursitis and hamstring injuries is one such area. In this paper, the author describes the surgical procedure and discusses the findings and preliminary outcomes in a group of the first 15 patients undergoing the procedure. The clinical rationale associated with the treatment algorithm is also discussed. Hamstring injuries have been effectively addressed in the past with a variety of open methods.(1,2) However, the endoscopic management of much pathology previously treated with more invasive, open approaches has evolved. The technique described in this chapter is another such evolution. Hamstring injuries are common and can affect all levels of The hamstrings originate from the ischial tuberosity and athletes. (3-7) There is a continuum of hamstring injuries insert distally below the knee on the proximal tibia, with the that can range from musculotendinous strains to avulsion exception of the short head of the biceps femoris. The tibial injuries. (3,4) Most hamstring strains do not require surgical branch of the sciatic nerve innervates the semitendinosus, intervention and resolve with a variety of modalities and semimembranosus, and the peroneal branch of the sciatic rest. (3-7) In some patients, chronic pain can occur at the nerve innervates the long head of the biceps femoris.(5) hamstring origin from either partial or complete tears as well as from chronic ischial bursitis. -

Studies on Brain and Spinal Cord Tumors
Studies on Brain and Spinal Cord Tumors Chapter 1 Osteochondroma of the Spine Iraj Lotfinia Professor of Neurosurgery, Tabriz Universsity of medical science, Tabriz, Iran. Fax: 00984113340830; Email: [email protected] Abstract Osteochondroma (OC) is the most common benign tumor of the bones, and it remains the most common precursor for secondary chondrosarcoma, which often occurs in the long bones’ metaphyseal areas. Rarely, it is also found in the spine. This tumor comprises a cartilage capped bone projection and is observed in both solitary and multiple forms. In many cases, the lesion can be definitively diagnosed according to radiological characteristics, but the rarity of these lesions in the spine, gradual onset of symptoms, and the frequent lack of observation of lesions in plain radiography may delay the diagnosis or cause misdiagnosis. These lesions are be- nign and do not risk the patient’s life; however, they rarely may be found to be a malignant degeneration that transformed into chondrosarcoma. When the lesion has led to clinical symptoms or has faced the patient with cosmetic challenges, or when definitive diagnosis is unknown, treatment is required. The primary treatment is the surgical removal of the lesion. Timely diagnosis and complete resection of the le- sion using surgery lead to complete recovery and prevent recurrence. 1. Introduction According to the World Health Organization’s (WHO’s) definition in 2002, osteocar- tilaginous exostosis are benign bone neoplasms covered by a cartilaginous cap created at the outer surface of the bone by endochondral ossification [1]. Osteochondroma (OC) is the most common benign primary tumor of the bone. -
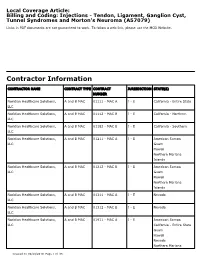
Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079)
Local Coverage Article: Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, A and B MAC 01111 - MAC A J - E California - Entire State LLC Noridian Healthcare Solutions, A and B MAC 01112 - MAC B J - E California - Northern LLC Noridian Healthcare Solutions, A and B MAC 01182 - MAC B J - E California - Southern LLC Noridian Healthcare Solutions, A and B MAC 01211 - MAC A J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01212 - MAC B J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01311 - MAC A J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01312 - MAC B J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01911 - MAC A J - E American Samoa LLC California - Entire State Guam Hawaii Nevada Northern Mariana Created on 09/28/2019. Page 1 of 33 CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Islands Article Information General Information Original Effective Date 10/01/2019 Article ID Revision Effective Date A57079 N/A Article Title Revision Ending Date Billing and Coding: Injections - Tendon, Ligament, N/A Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma Retirement Date N/A Article Type Billing and Coding AMA CPT / ADA CDT / AHA NUBC Copyright Statement CPT codes, descriptions and other data only are copyright 2018 American Medical Association. -

Tarsal Tunnel Syndrome: a Still Challenge Condition
Rev Bras Neurol. 55(1):12-17, 2019 TARSAL TUNNEL SYNDROME: A STILL CHALLENGE CONDITION SÍNDROME DO TÚNEL DO TARSO: UMA CONDIÇÃO AINDA DESAFIADORA Celmir de Oliveira Vilaça1,2, Bruno Pessoa3, Janaína de Moraes Silva4, Victor Hugo Bastos5, Diandra Martins5, Silmar Teixeira6, Victor Marinho6, Rossano Fiorelli7, Vanessa de Albuquerque Dinoa8; Marco Orsini7, 9 ABSTRACT RESUMO Tarsal tunnel syndrome is a rare, under diagnosed and often confu- A Síndrome do túnel do tarso é uma rara e subdiagnosticada neuro- sed neuropathy with other clinical entities. There is a lack of popula- patia geralmente confundida com outras entidades clínicas. Há falta tion studies on this disease. Herein, we performed a non-systematic de estudos populacionais sobre a doença. Assim sendo, realizamos review of articles between January 1992 and February 2018. Althou- uma revisão da literatura de artigos entre Janeiro de 1992 e fevereiro gh with a less complex anatomy comparing to the carpal tunnel, the de 2018. Apesar de possuir uma anatomia de menor complexidade tarsal tunnel is source of pain and some other conditions. Treatment comparada ao túnel do carpo, o túnel do tarso é origem de dor e involves conservative measures such as analgesics and physical the- algumas outras condições. O tratamento envolve medidas conserva- rapy rehabilitation or surgical procedures in case of conservative doras como analgésicos e terapia de reabilitação ou procedimentos treatment failure. Randomized control studies are lack and manda- cirúrgicos, em caso de falha do tratamento conservador. Estudos ran- tory for uncover the best modality of treatment for this condition. domizados são escassos e necessários para descoberta da melhor modalidade de tratamento desta condição.