Aspects of Additional Psychiatric Disorders in Severe
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dietary Patterns Are Differentially Associated with Atypical and Melancholic Subtypes of Depression
nutrients Article Dietary Patterns Are Differentially Associated with Atypical and Melancholic Subtypes of Depression Aurélie M. Lasserre 1,* , Marie-Pierre F. Strippoli 1 , Pedro Marques-Vidal 2 , Lana J. Williams 3, Felice N. Jacka 3, Caroline L. Vandeleur 1, Peter Vollenweider 2 and Martin Preisig 1 1 Department of Psychiatry, Lausanne University Hospital and University of Lausanne, 1011 Lausanne, Switzerland; [email protected] (M.-P.F.S.); [email protected] (C.L.V.); [email protected] (M.P.) 2 Department of Medicine, Internal Medicine, Lausanne University Hospital and University of Lausanne, 1011 Lausanne, Switzerland; [email protected] (P.M.-V.); [email protected] (P.V.) 3 Barwon Health, IMPACT—The Institute for Mental and Physical Health and Clinical Translation, Deakin University, Geelong 3220, Australia; [email protected] (L.J.W.); [email protected] (F.N.J.) * Correspondence: [email protected]; Tel.: +41-21-314-3552 Abstract: Diet has been associated with the risk of depression, whereas different subtypes of depres- sion have been linked with different cardiovascular risk factors (CVRFs). In this study, our aims were to (1) identify dietary patterns with exploratory factor analysis, (2) assess cross-sectional associations between dietary patterns and depression subtypes, and (3) examine the potentially mediating effect of dietary patterns in the associations between CVRFs and depression subtypes. In the first follow-up of the population-based CoLaus|PsyCoLaus study (2009–2013, 3554 participants, 45.6% men, mean age Citation: Lasserre, A.M.; Strippoli, 57.5 years), a food frequency questionnaire assessed dietary intake and a semi-structured interview M.-P.F.; Marques-Vidal, P.; Williams, allowed to characterize major depressive disorder into current or remitted atypical, melancholic, L.J.; Jacka, F.N.; Vandeleur, C.L.; and unspecified subtypes. -

Alteration of Immune Markers in a Group of Melancholic Depressed Patients and Their Response to Electroconvulsive Therapy
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author J Affect Manuscript Author Disord. Author Manuscript Author manuscript; available in PMC 2017 February 03. Published in final edited form as: J Affect Disord. 2016 November 15; 205: 60–68. doi:10.1016/j.jad.2016.06.035. Alteration of Immune Markers in a group of Melancholic Depressed patients and their Response to Electroconvulsive Therapy Gavin Rush1,*, Aoife O’Donovan2,3,4,5, Laura Nagle1, Catherine Conway1, AnnMaria McCrohan2,3, Cliona O’Farrelly6, James V. Lucey1, and Kevin M. Malone2,3 1St. Patrick’s University Hospital, Dublin, Ireland 2School of Medicine and Medical Sciences, University College Dublin, Dublin, Ireland 3Department of Psychiatry, Psychotherapy and Mental Health Research, St. Vincent’s University Hospital, Dublin, Ireland 4Stress and Health Research Program, San Francisco Veteran’s Affairs Medical Center, San Francisco, California 5Department of Psychiatry, University of California, San Francisco, California 6School of Biochemistry and Immunology, University of Dublin Trinity College, Dublin, Ireland Abstract Background—Immune system dysfunction is implicated in the pathophysiology of major depression, and is hypothesized to normalize with successful treatment. We aimed to investigate immune dysfunction in melancholic depression and its response to ECT. Methods—55 melancholic depressed patients and 26 controls participated. 33 patients (60%) were referred for ECT. Blood samples were taken at baseline, one hour after the first ECT session, and 48 hours after ECT series completion. Results—At baseline, melancholic depressed patients had significantly higher levels of the pro- inflammatory cytokine IL-6, and lower levels of the regulatory cytokine TGF-β than controls. A significant surge in IL-6 levels was observed one hour after the first ECT session, but neither IL-6 nor TGF-β levels normalized after completion of ECT series. -

Ketamine and Depression: a Review Wesley C
International Journal of Transpersonal Studies Volume 33 | Issue 2 Article 6 7-1-2014 Ketamine and Depression: A Review Wesley C. Ryan University of Washington Cole J. Marta University of California, Los Angeles Ralph J. Koek University of California, Los Angeles Follow this and additional works at: https://digitalcommons.ciis.edu/ijts-transpersonalstudies Part of the Philosophy Commons, Psychiatry and Psychology Commons, and the Religion Commons Recommended Citation Ryan, W. C., Marta, C. J., & Koek, R. J. (2014). Ryan, W. C., Marta, C. J., & Koek, R. J. (2014). Ketamine and depression: A review. International Journal of Transpersonal Studies, 33(2), 40–74.. International Journal of Transpersonal Studies, 33 (2). http://dx.doi.org/ 10.24972/ijts.2014.33.2.40 This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. This Special Topic Article is brought to you for free and open access by the Journals and Newsletters at Digital Commons @ CIIS. It has been accepted for inclusion in International Journal of Transpersonal Studies by an authorized administrator of Digital Commons @ CIIS. For more information, please contact [email protected]. Ketamine and Depression: A Review Wesley C. Ryan University of Washington Seattle, WA, USA Cole J. Marta Ralph J. Koek University of California at Los Angeles University of California at Los Angeles North Hills, CA, USA North Hills, CA, USA Ketamine, via intravenous infusions, has emerged as a novel therapy for treatment-resistant depression, given rapid onset and demonstrable efficacy in both unipolar and bipolar depression. Duration of benefit, on the order of days, varies between these subtypes, but appears longer in unipolar depression. -

A History of the Pharmacological Treatment of Bipolar Disorder
International Journal of Molecular Sciences Review A History of the Pharmacological Treatment of Bipolar Disorder Francisco López-Muñoz 1,2,3,4,* ID , Winston W. Shen 5, Pilar D’Ocon 6, Alejandro Romero 7 ID and Cecilio Álamo 8 1 Faculty of Health Sciences, University Camilo José Cela, C/Castillo de Alarcón 49, 28692 Villanueva de la Cañada, Madrid, Spain 2 Neuropsychopharmacology Unit, Hospital 12 de Octubre Research Institute (i+12), Avda. Córdoba, s/n, 28041 Madrid, Spain 3 Portucalense Institute of Neuropsychology and Cognitive and Behavioural Neurosciences (INPP), Portucalense University, R. Dr. António Bernardino de Almeida 541, 4200-072 Porto, Portugal 4 Thematic Network for Cooperative Health Research (RETICS), Addictive Disorders Network, Health Institute Carlos III, MICINN and FEDER, 28029 Madrid, Spain 5 Departments of Psychiatry, Wan Fang Medical Center and School of Medicine, Taipei Medical University, 111 Hsin Long Road Section 3, Taipei 116, Taiwan; [email protected] 6 Department of Pharmacology, Faculty of Pharmacy, University of Valencia, Avda. Vicente Andrés, s/n, 46100 Burjassot, Valencia, Spain; [email protected] 7 Department of Pharmacology and Toxicology, Faculty of Veterinary Medicine, Complutense University, Avda. Puerta de Hierro, s/n, 28040 Madrid, Spain; [email protected] 8 Department of Biomedical Sciences (Pharmacology Area), Faculty of Medicine and Health Sciences, University of Alcalá, Crta. de Madrid-Barcelona, Km. 33,600, 28871 Alcalá de Henares, Madrid, Spain; [email protected] * Correspondence: fl[email protected] or [email protected] Received: 4 June 2018; Accepted: 13 July 2018; Published: 23 July 2018 Abstract: In this paper, the authors review the history of the pharmacological treatment of bipolar disorder, from the first nonspecific sedative agents introduced in the 19th and early 20th century, such as solanaceae alkaloids, bromides and barbiturates, to John Cade’s experiments with lithium and the beginning of the so-called “Psychopharmacological Revolution” in the 1950s. -
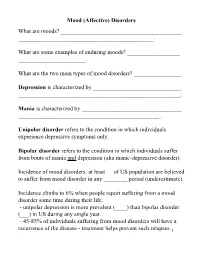
Mood (Affective) Disorders What Are Moods? ______
Mood (Affective) Disorders What are moods? _________________________________________ ______________________________________________. What are some examples of enduring moods? __________________ _______________________. What are the two main types of mood disorders? ________________ Depression is characterized by ______________________________ _______________________________________________________; Mania is characterized by __________________________________ ________________________________________________. Unipolar disorder refers to the condition in which individuals experience depressive symptoms only. Bipolar disorder refers to the condition in which individuals suffer from bouts of mania and depression (aka manic-depressive disorder). Incidence of mood disorders: at least __ of US population are believed to suffer from mood disorder in any ________ period (underestimate). Incidence climbs to 6% when people report suffering from a mood disorder some time during their life. - unipolar depression is more prevalent (____) than bipolar disorder (___) in US during any single year. - 45-85% of individuals suffering from mood disorders will have a recurrence of the disease - treatment helps prevent such relapses.1 Diagnostic criteria for Mania Criterion A - a distinct period of abnormally and persistently ______________ ____________________________. - abnormally here is defined in relation to the person’s normal behavior; - usually lasts _________________. Criterion B (requires 3 of the following symptoms, 4 if the mood is characterized as irritable): 1. __________________________________; 2. ________________________ (e.g., feels rested after only 3 hours of sleep); 3. More talkative than usual or pressure to keep talking; 4. ___________ (jumping to a new line of thought before completing the preceding one) or subjective experience that thoughts are racing; 5. ___________ (i.e., attention easily drawn by unimportant stimuli); 6. Increase in goal-directed activity (socially, at work or school, or sexually) or _____________________; 7. -
A Practical Approach to Subtyping Depression Among Your Patients
SECOND OF 2 PARTS A practical approach to subtyping depression among your patients Improve outcomes by understanding the forms that depressive disorders can take epression—sad, empty, or irritable mood accompanied by somatic or cognitive changes—is not a homoge- Dneous condition. Recognizing subtypes of depressive illness can guide treatment and relieve your patient’s suf- fering. In this 2-part article [April and May 2014 issues], I summarize information about clinically distinct subtypes of depression, as they are recognized within diagnostic systems or as descriptors of treatment outcomes for particular sub- groups of patients. My focus is on practical considerations for assessing and managing depression. Because many forms of the disorder respond inadequately to initial antidepressant treatment, optimal “next-step” pharmacotherapy, after nonre- sponse or partial response, often hinges on clinical subtyping. JON KRAUSE/THE ISPOT.COM The second part of this article examines “situational,” treat- ment-resistant, melancholic, agitated, anxious, and atypical Joseph F. Goldberg, MD depression; depression occurring with a substance use disor- Clinical Professor of Psychiatry Icahn School of Medicine at Mount Sinai der; premenstrual dysphoric disorder; and seasonal affective New York, New York disorder. Treatments for these subtypes for which there is evi- Director, Affective Disorders Research Program dence, or a clinical rationale, are given in the Table, page 42. Silver Hill Hospital New Canaan, Connecticut ‘Situational’ depression In recent decades, the phenomenon of nonsyndromal depres- sion after a life stress has undergone many name changes but lit- tle conceptual revision: “situational,” “reactive,” and “neurotic” labels for depression that were used before DSM-III became “adjustment disorders” in DSM-IV-TR and then “stress Disclosure Dr. -

Phenomenal Depth a Common Phenomenological Dimension in Depression and Depersonalization
Michael Gaebler,* Jan-Peter Lamke,* Judith K. Daniels and Henrik Walter Phenomenal Depth A Common Phenomenological Dimension in Depression and Depersonalization Abstract: Describing, understanding, and explaining subjective expe- rience in depression is a great challenge for psychopathology. Attempts to uncover neurobiological mechanisms of those experi- ences are in need of theoretical concepts that are able to bridge phen- omenological descriptions and neurocognitive approaches, which allow us to measure indicators of those experiences in quantitative terms. Based on our own ongoing work with patients who suffer from depersonalization disorder (DPD) and describe their experience as flat and detached from self, body, and world, we introduce the idea of phenomenal depth as such a concept. Phenomenal depth is conceptu- alized as a dimension inherent to all experiences, describing the relat- Copyright (c) Imprint Academic 2013 edness of one’s self with one’s mental processes, body, and the world. For personal use only -- not for reproduction More precisely, it captures the experience of this relatedness and embeddedness of one’s experiences, and it is thus a meta- or second- order experience. The psychopathology of DPD patients can be understood very generally as an instance of reduced phenomenal depth. We will argue that similar experiences in depression can also be understood as a reduction in phenomenal depth. We relate those ideas to neurocognitive studies of perception, emotion regulation, and the idea of predictive coding. Finally, we will speculate about possible Correspondence: Division of Mind & Brain Research, Department of Psychiatry & Psychotherapy, Charité - Universitätsmedizin Berlin, D-10117 Berlin Email: [email protected] [*] equal contribution Journal of Consciousness Studies, 20, No. -

Healing the Stigma of Depression
Healing the Stigma of Depression A Guide for Helping Professionals A resource for helping professionals of all disciplines serving people who may be affected by depression—and by its stigma. Written by Pamela Woll, MA, CADP for the Midwest AIDS Training and Education Center and the Great Lakes Addiction Technology Transfer Center Healing the Stigma of Depression: A Guide for Helping Professionals Published by: Midwest AIDS Training and Education Center Nathan Linsk, PhD, Principal Investigator Barbara Schechtman, MPH, Executive Director Great Lakes Addiction Technology Transfer Center Larry Bennett, PhD, Principal Investigator Nathan Linsk, PhD, Co-Principal Investigator Lonnetta Albright, Director Project Leader: Barbara Schechtman, MPH Co-Leader: Lonnetta Albright Author: Pamela Woll, MA, CADP Research Assistant: Charles M. Bright, LCSW, ACSW Midwest AIDS Training and Education Center Great Lakes Addiction Technology Transfer Center Jane Addams College of Social Work University of Illinois at Chicago 1640 W. Roosevelt Road, Suite 511 (M/C 779) Chicago, Illinois 60608 November, 2007 This publication was produced by the Midwest AIDS Training and Education Center (partially supported by a grant from the Health Resources and Services Administration and through funds raised independently), and the Great Lakes Addiction Technology Transfer Center (under a cooperative agreement from the Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment. This was produced by the Midwest AIDS Training and Education Center, funded in part by HRSA Grant # H4A HA00062. For more information on obtaining copies of this publication, please call (312) 996-1373. Developed in part under a grant funded by the Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration, U.S. -

Melancholic Depression and Its Relationship to Cognitive Decline Elizabeth Corsentino
Florida State University Libraries Electronic Theses, Treatises and Dissertations The Graduate School 2010 Melancholic Depression and Its Relationship to Cognitive Decline Elizabeth Corsentino Follow this and additional works at the FSU Digital Library. For more information, please contact [email protected] THE FLORIDA STATE UNIVERSITY COLLEGE OF ARTS AND SCIENCES MELANCHOLIC DEPRESSION AND ITS RELATIONSHIP TO COGNITIVE DECLINE By Elizabeth Corsentino A Thesis submitted to the Department of Psychology in partial fulfillment of the requirements for the degree of Master of Science Degree Awarded: Fall Semester, 2010 The members of the committee approve the Thesis of Elizabeth Corsentino defended on October 18, 2010. _______________________________________ Natalie Sachs-Ericsson Professor Directing Thesis _______________________________________ Thomas Joiner Professor Co-Directing Thesis _______________________________________ Richard Wagner Committee Member Approved: _____________________________________ Janet Kistner, Chair, Department of Psychology _____________________________________ Joseph Travis, Dean, College of Arts and Sciences The Graduate School has verified and approved the above-named committee members. ii ACKNOWLEDGEMENTS I would like to acknowledge my research advisor, Natalie Sachs-Ericsson, committee members Thomas Joiner and Richard Wagner for their helpful comments and guidance during the preparation of this manuscript. iii TABLE OF CONTENTS Abstract ........................................................................................................................................ -

E.1 DEPRESSION in CHILDREN and ADOLESCENTS 2015 Edition
IACAPAP Textbook of Child and Adolescent Mental Health Chapter MOOD DISORDERS E.1 DEPRESSION IN CHILDREN AND ADOLESCENTS 2015 Edition Joseph M Rey, Tolulope T Bella-Awusah & Jing Liu Joseph M Rey MD, PhD, FRANZCP Professor of Psychiatry, Notre Dame University Medical School Sydney & Honorary Professor, University of Sydney Medical School, Sydney, Australia Conflict of interest: none declared Tolulope T Bella-Awusah MBBS(IB), FWACP Department of Psychiatry, College of Medicine, University of Ibadan & University College Hospital, Ibadan, Nigeria Conflict of interest: none declared Jing Liu MD Professor & Director, Clinical Department for Children and Adolescents, Mental Health Institute & the Sixth Hospital, Peking University, Beijing, China. Vice-President, Asian Society for Child and Adolescent Psychiatry & Allied Photo from repowerup.com Professions This publication is intended for professionals training or practicing in mental health and not for the general public. The opinions expressed are those of the authors and do not necessarily represent the views of the Editor or IACAPAP. This publication seeks to describe the best treatments and practices based on the scientific evidence available at the time of writing as evaluated by the authors and may change as a result of new research. Readers need to apply this knowledge to patients in accordance with the guidelines and laws of their country of practice. Some medications may not be available in some countries and readers should consult the specific drug information since not all dosages and unwanted effects are mentioned. Organizations, publications and websites are cited or linked to illustrate issues or as a source of further information. This does not mean that authors, the Editor or IACAPAP endorse their content or recommendations, which should be critically assessed by the reader. -
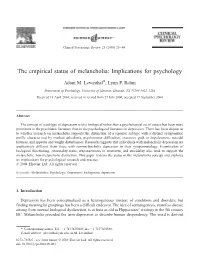
The Empirical Status of Melancholia: Implications for Psychology
Clinical Psychology Review 25 (2005) 25–44 The empirical status of melancholia: Implications for psychology Adam M. Leventhal*, Lynn P. Rehm Department of Psychology, University of Houston, Houston, TX 77204-5022, USA Received 19 April 2004; received in revised form 27 July 2004; accepted 17 September 2004 Abstract The concept of a subtype of depression with a biological rather than a psychological set of causes has been more prominent in the psychiatric literature than in the psychological literature on depression. There has been dispute as to whether research on melancholia supports the distinction of a separate subtype with a distinct symptomatic profile characterized by marked anhedonia, psychomotor difficulties, excessive guilt or hopelessness, suicidal features, and appetite and weight disturbances. Research suggests that individuals with melancholic depression are qualitatively different from those with non-melancholic depression in their symptomatology. Examination of biological functioning, personality traits, responsiveness to treatment, and suicidality also tend to support the melancholic–non-melancholic distinction. This paper reviews the status of the melancholia concept and explores its implications for psychological research and practice. D 2004 Elsevier Ltd. All rights reserved. Keywords: Melancholia; Psychology; Depression; Endogenous depression 1. Introduction Depression has been conceptualized as a heterogeneous mixture of conditions and disorders, but finding meaningful groupings has been a difficult endeavor. The idea of somatogenesis, manifest disease arising from internal biological dysfunction, is at least as old as Hippocrates’ writings in the 5th century BC. Melancholia preceded the term depression to describe human despondency. The word is derived * Corresponding author. Tel.: +1 7137438600; fax: +1 7137438588. E-mail address: [email protected] (A.M. -

The Categorisation of Dysthymic Disorder: Can Its Constituents Be Meaningfully Apportioned? 82 | Chapter 5
VU Research Portal Insight into the heterogeneity of depressive disorders Rhebergen, D. 2012 document version Publisher's PDF, also known as Version of record Link to publication in VU Research Portal citation for published version (APA) Rhebergen, D. (2012). Insight into the heterogeneity of depressive disorders. General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal ? Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. E-mail address: [email protected] Download date: 29. Sep. 2021 Chapter 55 The categorisation of Dysthymic Disorder: Can its constituents be meaningfully apportioned? 82 | Chapter 5 ABSTRACT Background Since its introduction in DSM-III, the validity of Dysthymia has been debated. Our objective is to further examine the concept of Dysthymia in an outpatient sample, and explore whether its constituents can be meaningfully apportioned. Methods 318 Patients attending the Black Dog Institute Depression Clinic were assessed by the Mini-International Neuropsychiatric Interview, and completed several self-report measures, in addition to clinical assessment by an Institute psychiatrist.