Workplace Mental Health Guideline: Depressive Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Adult Attachment and Life History Patterns in People with Borderline Personality Disorder
Adult attachment and life history patterns in people with Borderline Personality Disorder Martin Brüne LWL University Hospital Bochum Division of Social Neuropsychiatry & Evolutionary Medicine Ruhr-University Bochum A tribute to John Bowlby for the first (and only) evolutionary theory in psychiatry and psychotherapy Behavioural ecology - life history theory r selection (fast track) K selection (slow track) Life history perspective - behavioural ecology perceived or real predictability (safe) perceived or real unpredictability (unsafe) Belsky, Steinberg & Draper, 1991 From life-history theory it is known that individuals should adjust their risk-taking behaviour to their residual reproductive value, that is, their expected future fitness. Individuals with relatively high expectations should be relatively risk averse, because they have to survive to realise those expectations. By the same reasoning, individuals with relatively low expectations should be relatively risk-prone because they have little to lose. Wolf et al., 2007 Life history perspective on personality traits Del Giudice, 2014 Life history perspective on personality traits Clinical features of Borderline Personality Disorder (BPD) ‣ Fear of abandonment. ‣ Unstable and intensive relationships with rapid changes between idealisation and derogation. ‣ Identity disorder. ‣ Impulsivity (spending money, sexuality, substance abuse, other risk-taking behaviours) ‣ Recurrent suicidal behaviour, threat of committing suicide or self-injurious behaviour. ‣ Emotional instability. ‣ Feelings -

Dietary Patterns Are Differentially Associated with Atypical and Melancholic Subtypes of Depression
nutrients Article Dietary Patterns Are Differentially Associated with Atypical and Melancholic Subtypes of Depression Aurélie M. Lasserre 1,* , Marie-Pierre F. Strippoli 1 , Pedro Marques-Vidal 2 , Lana J. Williams 3, Felice N. Jacka 3, Caroline L. Vandeleur 1, Peter Vollenweider 2 and Martin Preisig 1 1 Department of Psychiatry, Lausanne University Hospital and University of Lausanne, 1011 Lausanne, Switzerland; [email protected] (M.-P.F.S.); [email protected] (C.L.V.); [email protected] (M.P.) 2 Department of Medicine, Internal Medicine, Lausanne University Hospital and University of Lausanne, 1011 Lausanne, Switzerland; [email protected] (P.M.-V.); [email protected] (P.V.) 3 Barwon Health, IMPACT—The Institute for Mental and Physical Health and Clinical Translation, Deakin University, Geelong 3220, Australia; [email protected] (L.J.W.); [email protected] (F.N.J.) * Correspondence: [email protected]; Tel.: +41-21-314-3552 Abstract: Diet has been associated with the risk of depression, whereas different subtypes of depres- sion have been linked with different cardiovascular risk factors (CVRFs). In this study, our aims were to (1) identify dietary patterns with exploratory factor analysis, (2) assess cross-sectional associations between dietary patterns and depression subtypes, and (3) examine the potentially mediating effect of dietary patterns in the associations between CVRFs and depression subtypes. In the first follow-up of the population-based CoLaus|PsyCoLaus study (2009–2013, 3554 participants, 45.6% men, mean age Citation: Lasserre, A.M.; Strippoli, 57.5 years), a food frequency questionnaire assessed dietary intake and a semi-structured interview M.-P.F.; Marques-Vidal, P.; Williams, allowed to characterize major depressive disorder into current or remitted atypical, melancholic, L.J.; Jacka, F.N.; Vandeleur, C.L.; and unspecified subtypes. -

Alteration of Immune Markers in a Group of Melancholic Depressed Patients and Their Response to Electroconvulsive Therapy
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author J Affect Manuscript Author Disord. Author Manuscript Author manuscript; available in PMC 2017 February 03. Published in final edited form as: J Affect Disord. 2016 November 15; 205: 60–68. doi:10.1016/j.jad.2016.06.035. Alteration of Immune Markers in a group of Melancholic Depressed patients and their Response to Electroconvulsive Therapy Gavin Rush1,*, Aoife O’Donovan2,3,4,5, Laura Nagle1, Catherine Conway1, AnnMaria McCrohan2,3, Cliona O’Farrelly6, James V. Lucey1, and Kevin M. Malone2,3 1St. Patrick’s University Hospital, Dublin, Ireland 2School of Medicine and Medical Sciences, University College Dublin, Dublin, Ireland 3Department of Psychiatry, Psychotherapy and Mental Health Research, St. Vincent’s University Hospital, Dublin, Ireland 4Stress and Health Research Program, San Francisco Veteran’s Affairs Medical Center, San Francisco, California 5Department of Psychiatry, University of California, San Francisco, California 6School of Biochemistry and Immunology, University of Dublin Trinity College, Dublin, Ireland Abstract Background—Immune system dysfunction is implicated in the pathophysiology of major depression, and is hypothesized to normalize with successful treatment. We aimed to investigate immune dysfunction in melancholic depression and its response to ECT. Methods—55 melancholic depressed patients and 26 controls participated. 33 patients (60%) were referred for ECT. Blood samples were taken at baseline, one hour after the first ECT session, and 48 hours after ECT series completion. Results—At baseline, melancholic depressed patients had significantly higher levels of the pro- inflammatory cytokine IL-6, and lower levels of the regulatory cytokine TGF-β than controls. A significant surge in IL-6 levels was observed one hour after the first ECT session, but neither IL-6 nor TGF-β levels normalized after completion of ECT series. -

Evolutionary Psychiatry and Nosology: Prospects and Limitations
Baltic International Yearbook of Cognition, Logic and Communication Volume 7 MORALITY AND THE COGNITIVE SCIENCES Article 5 2012 Evolutionary Psychiatry and Nosology: Prospects and Limitations Luc Faucher Université du Québec à Montréal Follow this and additional works at: https://newprairiepress.org/biyclc This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. Recommended Citation Faucher, Luc (2012) "Evolutionary Psychiatry and Nosology: Prospects and Limitations," Baltic International Yearbook of Cognition, Logic and Communication: Vol. 7. https://doi.org/10.4148/ biyclc.v7i0.1776 This Proceeding of the Symposium for Cognition, Logic and Communication is brought to you for free and open access by the Conferences at New Prairie Press. It has been accepted for inclusion in Baltic International Yearbook of Cognition, Logic and Communication by an authorized administrator of New Prairie Press. For more information, please contact [email protected]. Evolutionary Psychiatry and Nosology 2 The Baltic International Yearbook of about some disorders. Using the case of depression, I will then Cognition, Logic and Communication show what kind of problems evolutionary explanations of partic- ular psychopathologies encounter. In conclusion, I will evaluate October 2012 Volume 7: Morality and the Cognitive Sciences where evolutionary thinking leaves us in regard to what I identify pages 1-64 DOI: 10.4148/biyclc.v7i0.1776 as the main problems of our current nosologies. I’ll then argue that the prospects of evolutionary psychiatry are not good. LUC FAUCHER 1. INTRODUCTION Université du Québec à Montréal This paper was originally a chapter prepared for a volume which unfor- tunately never got to be published. -

Evolutionary Explanations of Eating Disorders
Psychological Topics 17 (2008), 2, 247-263 Original Scientific Article – UDC – 616.89-008.441.42 159.015.7 Evolutionary Explanations of Eating Disorders Igor Kardum, Asmir Gračanin, Jasna Hudek-Knežević University of Rijeka, Faculty of Arts and Sciences Department of Psychology Abstract This article reviews several most important evolutionary mechanisms that underlie eating disorders. The first part clarifies evolutionary foundations of mental disorders and various mechanisms leading to their development. In the second part selective pressures and evolved adaptations causing contemporary epidemic of obesity as well as differences in dietary regimes and life-style between modern humans and their ancestors are described. Concerning eating disorders, a number of current evolutionary explanations of anorexia nervosa are presented together with their main weaknesses. Evolutionary explanations of eating disorders based on the reproductive suppression hypothesis and its variants derived from kin selection theory and the model of parental manipulation were elaborated. The sexual competition hypothesis of eating disorder, adapted to flee famine hypothesis as well as explanation based on the concept of social attention holding power and the need to belonging were also explained. The importance of evolutionary theory in modern conceptualization and research of eating disorders is emphasized. Keywords: eating disorders, evolutionary theory, reproductive suppression, sexual competition INTRODUCTION There is a disagreement among scientists about the basic definition of mental disorder, and usually discussions concerning its definition encompass the role of social values as well as the centrality and the necessity of the presence of failures in evolved adaptive mechanisms (Lilienfield & Marino, 1995; Wakefield, 1999, 2005). Evolutionary reasoning can help to discriminate between conditions of an Igor Kardum, University of Rijeka, Faculty of Arts and Sciences, Department of Psychology, Slavka Krautzeka bb, 51000 Rijeka, Croatia. -

Ketamine and Depression: a Review Wesley C
International Journal of Transpersonal Studies Volume 33 | Issue 2 Article 6 7-1-2014 Ketamine and Depression: A Review Wesley C. Ryan University of Washington Cole J. Marta University of California, Los Angeles Ralph J. Koek University of California, Los Angeles Follow this and additional works at: https://digitalcommons.ciis.edu/ijts-transpersonalstudies Part of the Philosophy Commons, Psychiatry and Psychology Commons, and the Religion Commons Recommended Citation Ryan, W. C., Marta, C. J., & Koek, R. J. (2014). Ryan, W. C., Marta, C. J., & Koek, R. J. (2014). Ketamine and depression: A review. International Journal of Transpersonal Studies, 33(2), 40–74.. International Journal of Transpersonal Studies, 33 (2). http://dx.doi.org/ 10.24972/ijts.2014.33.2.40 This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. This Special Topic Article is brought to you for free and open access by the Journals and Newsletters at Digital Commons @ CIIS. It has been accepted for inclusion in International Journal of Transpersonal Studies by an authorized administrator of Digital Commons @ CIIS. For more information, please contact [email protected]. Ketamine and Depression: A Review Wesley C. Ryan University of Washington Seattle, WA, USA Cole J. Marta Ralph J. Koek University of California at Los Angeles University of California at Los Angeles North Hills, CA, USA North Hills, CA, USA Ketamine, via intravenous infusions, has emerged as a novel therapy for treatment-resistant depression, given rapid onset and demonstrable efficacy in both unipolar and bipolar depression. Duration of benefit, on the order of days, varies between these subtypes, but appears longer in unipolar depression. -

A History of the Pharmacological Treatment of Bipolar Disorder
International Journal of Molecular Sciences Review A History of the Pharmacological Treatment of Bipolar Disorder Francisco López-Muñoz 1,2,3,4,* ID , Winston W. Shen 5, Pilar D’Ocon 6, Alejandro Romero 7 ID and Cecilio Álamo 8 1 Faculty of Health Sciences, University Camilo José Cela, C/Castillo de Alarcón 49, 28692 Villanueva de la Cañada, Madrid, Spain 2 Neuropsychopharmacology Unit, Hospital 12 de Octubre Research Institute (i+12), Avda. Córdoba, s/n, 28041 Madrid, Spain 3 Portucalense Institute of Neuropsychology and Cognitive and Behavioural Neurosciences (INPP), Portucalense University, R. Dr. António Bernardino de Almeida 541, 4200-072 Porto, Portugal 4 Thematic Network for Cooperative Health Research (RETICS), Addictive Disorders Network, Health Institute Carlos III, MICINN and FEDER, 28029 Madrid, Spain 5 Departments of Psychiatry, Wan Fang Medical Center and School of Medicine, Taipei Medical University, 111 Hsin Long Road Section 3, Taipei 116, Taiwan; [email protected] 6 Department of Pharmacology, Faculty of Pharmacy, University of Valencia, Avda. Vicente Andrés, s/n, 46100 Burjassot, Valencia, Spain; [email protected] 7 Department of Pharmacology and Toxicology, Faculty of Veterinary Medicine, Complutense University, Avda. Puerta de Hierro, s/n, 28040 Madrid, Spain; [email protected] 8 Department of Biomedical Sciences (Pharmacology Area), Faculty of Medicine and Health Sciences, University of Alcalá, Crta. de Madrid-Barcelona, Km. 33,600, 28871 Alcalá de Henares, Madrid, Spain; [email protected] * Correspondence: fl[email protected] or [email protected] Received: 4 June 2018; Accepted: 13 July 2018; Published: 23 July 2018 Abstract: In this paper, the authors review the history of the pharmacological treatment of bipolar disorder, from the first nonspecific sedative agents introduced in the 19th and early 20th century, such as solanaceae alkaloids, bromides and barbiturates, to John Cade’s experiments with lithium and the beginning of the so-called “Psychopharmacological Revolution” in the 1950s. -
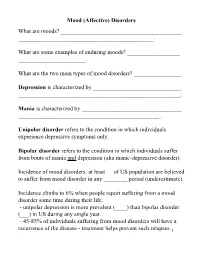
Mood (Affective) Disorders What Are Moods? ______
Mood (Affective) Disorders What are moods? _________________________________________ ______________________________________________. What are some examples of enduring moods? __________________ _______________________. What are the two main types of mood disorders? ________________ Depression is characterized by ______________________________ _______________________________________________________; Mania is characterized by __________________________________ ________________________________________________. Unipolar disorder refers to the condition in which individuals experience depressive symptoms only. Bipolar disorder refers to the condition in which individuals suffer from bouts of mania and depression (aka manic-depressive disorder). Incidence of mood disorders: at least __ of US population are believed to suffer from mood disorder in any ________ period (underestimate). Incidence climbs to 6% when people report suffering from a mood disorder some time during their life. - unipolar depression is more prevalent (____) than bipolar disorder (___) in US during any single year. - 45-85% of individuals suffering from mood disorders will have a recurrence of the disease - treatment helps prevent such relapses.1 Diagnostic criteria for Mania Criterion A - a distinct period of abnormally and persistently ______________ ____________________________. - abnormally here is defined in relation to the person’s normal behavior; - usually lasts _________________. Criterion B (requires 3 of the following symptoms, 4 if the mood is characterized as irritable): 1. __________________________________; 2. ________________________ (e.g., feels rested after only 3 hours of sleep); 3. More talkative than usual or pressure to keep talking; 4. ___________ (jumping to a new line of thought before completing the preceding one) or subjective experience that thoughts are racing; 5. ___________ (i.e., attention easily drawn by unimportant stimuli); 6. Increase in goal-directed activity (socially, at work or school, or sexually) or _____________________; 7. -
A Practical Approach to Subtyping Depression Among Your Patients
SECOND OF 2 PARTS A practical approach to subtyping depression among your patients Improve outcomes by understanding the forms that depressive disorders can take epression—sad, empty, or irritable mood accompanied by somatic or cognitive changes—is not a homoge- Dneous condition. Recognizing subtypes of depressive illness can guide treatment and relieve your patient’s suf- fering. In this 2-part article [April and May 2014 issues], I summarize information about clinically distinct subtypes of depression, as they are recognized within diagnostic systems or as descriptors of treatment outcomes for particular sub- groups of patients. My focus is on practical considerations for assessing and managing depression. Because many forms of the disorder respond inadequately to initial antidepressant treatment, optimal “next-step” pharmacotherapy, after nonre- sponse or partial response, often hinges on clinical subtyping. JON KRAUSE/THE ISPOT.COM The second part of this article examines “situational,” treat- ment-resistant, melancholic, agitated, anxious, and atypical Joseph F. Goldberg, MD depression; depression occurring with a substance use disor- Clinical Professor of Psychiatry Icahn School of Medicine at Mount Sinai der; premenstrual dysphoric disorder; and seasonal affective New York, New York disorder. Treatments for these subtypes for which there is evi- Director, Affective Disorders Research Program dence, or a clinical rationale, are given in the Table, page 42. Silver Hill Hospital New Canaan, Connecticut ‘Situational’ depression In recent decades, the phenomenon of nonsyndromal depres- sion after a life stress has undergone many name changes but lit- tle conceptual revision: “situational,” “reactive,” and “neurotic” labels for depression that were used before DSM-III became “adjustment disorders” in DSM-IV-TR and then “stress Disclosure Dr. -

Phenomenal Depth a Common Phenomenological Dimension in Depression and Depersonalization
Michael Gaebler,* Jan-Peter Lamke,* Judith K. Daniels and Henrik Walter Phenomenal Depth A Common Phenomenological Dimension in Depression and Depersonalization Abstract: Describing, understanding, and explaining subjective expe- rience in depression is a great challenge for psychopathology. Attempts to uncover neurobiological mechanisms of those experi- ences are in need of theoretical concepts that are able to bridge phen- omenological descriptions and neurocognitive approaches, which allow us to measure indicators of those experiences in quantitative terms. Based on our own ongoing work with patients who suffer from depersonalization disorder (DPD) and describe their experience as flat and detached from self, body, and world, we introduce the idea of phenomenal depth as such a concept. Phenomenal depth is conceptu- alized as a dimension inherent to all experiences, describing the relat- Copyright (c) Imprint Academic 2013 edness of one’s self with one’s mental processes, body, and the world. For personal use only -- not for reproduction More precisely, it captures the experience of this relatedness and embeddedness of one’s experiences, and it is thus a meta- or second- order experience. The psychopathology of DPD patients can be understood very generally as an instance of reduced phenomenal depth. We will argue that similar experiences in depression can also be understood as a reduction in phenomenal depth. We relate those ideas to neurocognitive studies of perception, emotion regulation, and the idea of predictive coding. Finally, we will speculate about possible Correspondence: Division of Mind & Brain Research, Department of Psychiatry & Psychotherapy, Charité - Universitätsmedizin Berlin, D-10117 Berlin Email: [email protected] [*] equal contribution Journal of Consciousness Studies, 20, No. -

Healing the Stigma of Depression
Healing the Stigma of Depression A Guide for Helping Professionals A resource for helping professionals of all disciplines serving people who may be affected by depression—and by its stigma. Written by Pamela Woll, MA, CADP for the Midwest AIDS Training and Education Center and the Great Lakes Addiction Technology Transfer Center Healing the Stigma of Depression: A Guide for Helping Professionals Published by: Midwest AIDS Training and Education Center Nathan Linsk, PhD, Principal Investigator Barbara Schechtman, MPH, Executive Director Great Lakes Addiction Technology Transfer Center Larry Bennett, PhD, Principal Investigator Nathan Linsk, PhD, Co-Principal Investigator Lonnetta Albright, Director Project Leader: Barbara Schechtman, MPH Co-Leader: Lonnetta Albright Author: Pamela Woll, MA, CADP Research Assistant: Charles M. Bright, LCSW, ACSW Midwest AIDS Training and Education Center Great Lakes Addiction Technology Transfer Center Jane Addams College of Social Work University of Illinois at Chicago 1640 W. Roosevelt Road, Suite 511 (M/C 779) Chicago, Illinois 60608 November, 2007 This publication was produced by the Midwest AIDS Training and Education Center (partially supported by a grant from the Health Resources and Services Administration and through funds raised independently), and the Great Lakes Addiction Technology Transfer Center (under a cooperative agreement from the Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment. This was produced by the Midwest AIDS Training and Education Center, funded in part by HRSA Grant # H4A HA00062. For more information on obtaining copies of this publication, please call (312) 996-1373. Developed in part under a grant funded by the Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration, U.S. -

An Evolutionary Model of Depression Markus J Rantala University of Turku Do Animals Get Depressed? Depression Is Common in Captivity Insects Have Emotions
An evolutionary model of depression Markus J Rantala University of Turku Do animals get depressed? Depression is common in captivity Insects have emotions • Unexpected rewards make bees optimistic • Agitated honeybees become pessimistic. Video: http://www.cell.com/current- biology/abstract/S0960-9822%2811%2900544-6 Science, 30 SEPTEMBER 2016 VOL 353 ISSUE 6307 Cockroaches developed depression (learned helplessness) when they were tortured with electric shocks. Brown & Stroup (1988). Learned helplessness in the cockroach (Periplaneta americana). Behav. Neural. Biol. 50(2):246-50. Shuttlebox Exercise alleviates depression in cockroaches • For three consecutive days, adult female cockroaches received an inescapable shock. • Next day half of females were exposed to ten minutes of forced exercise on a treadmill while the other half did not exercise. • Both groups then performed a shuttle box escape task. • The cockroaches exposed to forced exercise did not become helpless in the shuttlebox escape task. In fruitflies, uncontrollable stress leads to depression (learned helplessness) Yang et al. 2013. Flies Cope with Uncontrollable Stress by Learned Helplessness. Current Biology 23, 799–803. Rejected flies turn to booze • In the fruitfly study, researchers subjected male flies to four days of repeated rejection by pairing them with females who had already mated. • The rejected males drank four times more alcohol than mated males Shohat-Ophir et al. 2012. Sexual Deprivation Increases Ethanol Intake in Drosophila. Science. 335, 1351-1355 Video: https://www.youtube.com/watch?v=sH9Xjk28cZ0 Rodents have been used for a long time as a model organism to study depression How to make rodents depressed? Rats harassed with robots get depressed Ishii et al.