The Highest Attainable Standard: the World Health Organization, Global Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Big Tech Dominance (1): the New Financial Tycoons
Paul-Adrien HYPPOLITE Antoine MICHON BIG TECH DOMINANCE (1): THE NEW FINANCIAL TYCOONS December 2018 fondapol.org 2 BIG TECH DOMINANCE (1): THE NEW FINANCIAL TYCOONS Paul-Adrien HYPPOLITE Antoine MICHON 3 The Fondation pour l’innovation politique is a French think tank for European integration and free economy. Chair: Nicolas Bazire Vice-chair: Grégoire Chertok Executive Director: Dominique Reynié Chair of Scientific and Evaluation Board: Christophe de Voogd 4 FONDATION POUR L’INNOVATION POLITIQUE A French think tank for European integration and free economy The Fondation pour l’innovation politique provides an independent forum for expertise, opinion and exchange aimed at producing and disseminating ideas and proposals. It contributes to pluralism of thought and the renewal of public discussion from a free market, forward-thinking and European perspective. Four main priorities guide the Foundation’s work: economic growth, the environment, values and digital technology. The website www.fondapol.org provides public access to all the Foundation’s work. Anyone can access and use all the data gathered for the various surveys via the platform “Data.fondapol” and the data relating to international surveys is available in several languages. In addition, our blog “Trop Libre” (Too Free) casts a critical eye over the news and the world of ideas. “Trop Libre” also provides extensive monitoring of the effects of the digital revolution on political, economic and social practices in its “Renaissance numérique” (Digital Renaissance) section. Additionally, reflecting the Foundation’s editorial policy, our blog “Anthropotechnie” aims to explore new avenues prompted by human enhancement, reproductive cloning, human/machine hybridization, genetic engineering and germline manipulation. -

Evolution, Not Revolution: the Effect of New Deal Legislation On
EVOLUTION, NOT REVOLUTION: THE EFFECT OF NEW DEAL LEGISLATION ON INDUSTRIAL GROWTH AND UNION DEVELOPMENT IN DALLAS, TEXAS M. Courtney Welch, B.S.E., M.A., Ed.D. Dissertation Prepared for the Degree of DOCTOR OF PHILOSOPHY UNIVERSITY OF NORTH TEXAS August 2010 APPROVED: Richard McCaslin, Major Professor and Chair of the Department of History Randolph Campbell, Committee Member John Todd, Committee Member Aaron Navarro, Committee Member Elizabeth Turner, Committee Member James D. Meernik, Acting Dean of the Robert B. Toulouse School of Graduate Studies Welch, M. Courtney. Evolution, Not Revolution: The Effect of New Deal Legislation on Industrial Growth and Union Development in Dallas, Texas. Doctor of Philosophy (History), August 2010, 226 pp., 9 tables, 11 illustrations, references, 145 titles. The New Deal legislation of the 1930s would threaten Dallas’ peaceful industrial appearance. In fact, New Deal programs and legislation did have an effect on the city, albeit an unbalanced mixture of positive and negative outcomes characterized by frustrated workers and industrial intimidation. To summarize, the New Deal did not bring a revolution, but it did continue an evolutionary change for reform. This dissertation investigated several issues pertaining to the development of the textile industry, cement industry, and the Ford automobile factory in Dallas and its labor history before, during, and after the New Deal. New Deal legislation not only created an avenue for industrial workers to achieve better representation but also improved their working conditions. Specifically focusing on the textile, cement, and automobile industries illustrates that the development of union representation is a spectrum, with one end being the passive but successful cement industry experience and the other end being the automobile industry union efforts, which were characterized by violence and intimidation. -

Energy Systems Integration: Implications for Public Policy
Energy Policy 143 (2020) 111609 Contents lists available at ScienceDirect Energy Policy journal homepage: http://www.elsevier.com/locate/enpol ☆ Energy Systems Integration: Implications for public policy Carlo Cambini a,*, Raffaele Congiu a, Tooraj Jamasb b, Manuel Llorca b, Golnoush Soroush c a Department of Management, Politecnico di Torino, Italy b Copenhagen School of Energy Infrastructure (CSEI), Department of Economics, Copenhagen Business School, Denmark c Florence School of Regulation – European University Institute, Florence, Italy ARTICLE INFO ABSTRACT JEL classification: Energy Systems Integration (ESI) is an emerging paradigm and at the centre of the EU energy debate. ESI takes a L51 holistic view of the electricity, gas, and heat sectors to deliver a clean, reliable, and affordable energy system. By L94 using the synergies within and between sectors, ESI aims to increase flexibility in the energy system, maximise Q4 the integration of renewable energy and distributed generation, and reduce environmental impact. While ESI- Keywords: enabling technologies have been studied from a technical perspective, the economic, regulatory, and policy Energy systems integration dimensions of ESI are yet to be analysed in depth. This paper discusses ESI in a multi-step approach. We first Sector coupling Regulation focus on the economics of ESI-enabling technologies. Then we briefly discuss how the EU national regulators Innovation incentivise their adoption. Major economic and policy barriers to ESI are identified and policy solutions to Research and development overcome these barriers are proposed. We conclude that current regulatory frameworks in the EU do not suf Economic and policy barriers ficiently stimulate ESI investments and only through proper design of incentives ESI can be adopted. -

Democracy on the Precipice Council of Europe Democracy 2011-12 Council of Europe Publishing Debates
Democracy on the Precipice Democracy Democracy is well-established and soundly practiced in most European countries. But despite unprecedented progress, there is growing dissatisfaction with the state of democracy and deepening mistrust of democratic institutions; a situation exacer- Democracy on the Precipice bated by the economic crisis. Are Europe’s democracies really under threat? Has the traditional model of European democracy exhausted its potential? A broad consensus is forming as to the urgent need to examine the origins of the crisis and to explore Council of Europe visions and strategies which could contribute to rebuilding confidence in democracy. Democracy Debates 2011-12 As Europe’s guardian of democracy, human rights and the rule of law, the Council of Europe is committed to exploring the state and practice of European democracy, as Debates of Europe Publishing 2011-12 Council Council of Europe Democracy well as identifying new challenges and anticipating future trends. In order to facilitate Preface by Thorbjørn Jagland this reflection, the Council of Europe held a series of Democracy Debates with the participation of renowned specialists working in a variety of backgrounds and disciplines. This publication presents the eight Democracy Debate lectures. Each presentation Zygmunt Bauman analyses a specific aspect of democracy today, placing the issues not only in their political context but also addressing the historical, technological and communication Ulrich Beck dimensions. The authors make proposals on ways to improve democratic governance Ayşe Kadıoğlu and offer their predictions on how democracy in Europe may evolve. Together, the presentations contribute to improving our understanding of democracy today and to John Keane recognising the ways it could be protected and strengthened. -

The London School of Economics and Political Science the New
The London School of Economics and Political Science The New Industrial Order: Vichy, Steel, and the Origins of the Monnet Plan, 1940-1946 Luc-André Brunet A thesis submitted to the Department of International History of the London School of Economics for the degree of Doctor of Philosophy, London, July 2014 1 Declaration I certify that the thesis I have presented for examination for the MPhil/PhD degree of the London School of Economics and Political Science is solely my own work other than where I have clearly indicated that it is the work of others (in which case the extent of any work carried out jointly by me and any other person is clearly identified in it). The copyright of this thesis rests with the author. Quotation from it is permitted, provided that full acknowledgement is made. This thesis may not be reproduced without my prior written consent. I warrant that this authorisation does not, to the best of my belief, infringe the rights of any third party. I declare that my thesis consists of 87,402 words. 2 Abstract Following the Fall of France in 1940, the nation’s industry was fundamentally reorganised under the Vichy regime. This thesis traces the history of the keystones of this New Industrial Order, the Organisation Committees, by focusing on the organisation of the French steel industry between the end of the Third Republic in 1940 and the establishment of the Fourth Republic in 1946. It challenges traditional views by showing that the Committees were created largely to facilitate economic collaboration with Nazi Germany. -

Camille Robcis the Biopolitics of Dignity
South Atlantic Quarterly Camille Robcis The Biopolitics of Dignity “Let us not allow, within a free nation, monuments of slavery, even voluntary.” —Pierre Anastase Torné, French deputy, April 6, 1792 A few days after the shocking attacks on the ofces of Charlie Hebdo in January 2015, several French political leaders called for the revival of the “crime of national indignity” as a possible sanction against terrorists of French citizenship. As the prime minister Manuel Valls put it, such a measure—backed up, according to surveys, by 76 percent of the French population—would “mark with symbolic force the consequences of the absolute transgression that a terrorist act con- stitutes” (Clavel 2015). Under French law, national indignity did indeed have a particular history and signifcation, one that was not simply “symbolic” but in fact quite concrete. As the historian Anne Simonin (2008) shows, “national indignity” was invented in 1944 by the legal experts of the Resis- tance as an exceptional measure to punish, retro- actively, the supporters of the Vichy regime who had collaborated with the Nazi occupiers and pro- moted anti-Semitic legislation. Between 1945 and 1951, around one hundred thousand citizens were The South Atlantic Quarterly 115:2, April 2016 doi 10.1215/00382876-3488431 © 2016 Duke University Press Published by Duke University Press South Atlantic Quarterly 314 The South Atlantic Quarterly • April 2016 accused of indignity and punished by “national degradation.” In practical terms, this meant that they were stripped of their civic rights and their pos- sessions, banned from exercising certain public positions and professions (lawyers, bankers, teachers), and forbidden to live in particular regions of France. -

Światowa Organizacja Zdrowia
M. Vasiliew, Student N. Kostynska, doradca językowy Żytomierski Instytut Medyczny ŚWIATOWA ORGANIZACJA ZDROWIA Światowa Organizacja Zdrowia wyspecjalizowana agencja Organizacji Narodów Zjednoczonych, jest główną organizacją międzynarodową, zajmuąca się problemami zdrowia. Jej siedzibą jest Genewa. W 1946 r. ONZ zwołała Międzynarodową Konferencję Zdrowia w Nowym Jorku, gdzie 61 krajów ratyfikowało konwencję WHO. W roku 1948 w liczbie już 88 członków ratyfikowano powstanie WHO. Do WHO należą obecnie 194 kraje. Głównym obchodem, organizowanym przez WHO co roku w dniu 7 kwietnia, jest Światowy Dzień Zdrowia. Zadaniem WHO jest: działanie na rzecz zwiększenia współpracy między państwami w dziedzinie ochrony zdrowia, zwalczania epidemii chorób zakaźnych, ustalanie norm dotyczących składu lekarstw i jakości żywności, dąży również do zapewnienia opieki medycznej ludności świata oraz zmniejszenia śmiertelności niemowląt. [6, c.3] Do największych sukcesów tej organizacji należy zwalczanie epidemii groźnych chorób, takich jak: gruźlica, malaria, cholera czy dżuma poprzez masowe szczepienie. WHO walczy także z AIDS. Główne organy Światowej Organizacji Zdrowia to: Sekretariat na czele z dyrektorem generalnym, Światowe Zgromadzenie Zdrowia, Rada Wykonawcza, Komitety Regionalne. Działalność WHO jest wspomagana przez 6 biur regionalnych oraz 147 biur krajowych i łącznikowych. Oprócz biura stałego mieszczącego się w Genewie, WHO posiada regionalne biura: Afryka – Brazzaville, dla obu Ameryk – Waszyngton, dla płd.-wsch. Azji – New Delhi, dla Europy Kopenhaga, dla regionu śródziemnomorskiego – Каir dla regionu zach. Pacyfiku – Manila. Władzą naczelną WHO jest Światowe Zgromadzenie Zdrowia, które stanowią przedstawiciele wszystkich krajów członkowskich, które zbiera się raz do roku w Genewie. Zgromadzenie wybiera na okres 3 lat Komitet Wykonawczy, w którego skład wchodzi 34 ekspertów w dziedzinie zdrowia proponowanych przez kraje członkowskie. Zadaniem Komitetu jest realizacja decyzji i wytycznych Zgromadzenia. -

CANDAU, Marcolino Gomes, Brazilian Physician and Second Director
1 CANDAU, Marcolino Gomes, Brazilian physician and second Director-General of the World Health Organization (WHO) 1953-1973, was born 30 May 1911 in Rio de Janeiro, Brazil and died 23 January 1983 in Geneva, Switzerland. He was the son of Julio Candau and Augusta Gomes Pereira. On 30 May 1936 he married Ena de Carvalho, with whom he had two sons. After their divorce he married Sîtâ Reelfs in 1973. Source: www.who.int/features/history/1940_1959/en/index7.html Candau’s family was of French-Portuguese ancestry. Candau studied at the School of Medicine of the State of Rio de Janeiro, where he earned his living by tutoring his fellow students on anatomy, and completed his medical training in 1933. Shortly after finishing his studies he decided to work in public health and demonstrated administrative skills in his first job as head of a provincial health unit in São João Marcos. A state scholarship allowed him to take a special course in public health at the University of Brazil in 1936. He also worked in the city health departments of Santana de Japuiba and Nova Iguaçu. In 1938 he was promoted to Assistant Director-General of the Department of Health of the State of Rio de Janeiro and appointed assistant professor of hygiene at the School of Medicine. In the same year Fred L. Soper, representative of the Rio de Janeiro-based Rockefeller Foundation in Brazil, asked Candau to work under his direction in a major eradication campaign against a malaria outbreak produced by the Anopheles gambiae mosquito, which resulted in Candau’s fieldwork as a medical officer in the Northeast Malaria Service. -

Stagflation in the 1930S: Why Did the French New Deal Fail?
Stagflation in the 1930s: Why did the French New Deal Fail? Jeremie Cohen-Setton, Joshua K. Hausman, and Johannes F. Wieland∗ August 15, 2014 VERSION 1.0. VERY PRELIMINARY. DO NOT CITE WITHOUT PERMISSION. The latest version is available here. Abstract Most countries started to recover from the Great Depression when they left the Gold Stan- dard. France did not. In 1936, France both left the Gold Standard and enacted New- Deal-style policies, in particular wage increases and a 40-hour week law. The result was stagflation; prices rose rapidly from 1936 to 1938 while output stagnated. Using panel data on sectoral output, we show that the 40-hour week restriction had strong negative effects on production. Absent this law, France would likely have followed the usual pattern of rapid recovery after leaving the Gold Standard. We construct a model to show how supply-side policies could have prevented output growth despite excess capacity and a large real interest rate decline. ∗Cohen-Setton: University of California, Berkeley. 530 Evans Hall #3880, Berkeley, CA 94720. Email: [email protected]. Phone: (510) 277-6413. Hausman: Ford School of Public Policy, Uni- versity of Michigan. 735 S. State St. #3309, Ann Arbor, MI 48109. Email: [email protected]. Phone: (734) 763-3479. Wieland: Department of Economics, University of California, San Diego. 9500 Gilman Dr. #0508, La Jolla, CA 92093-0508. Email: [email protected]. Phone: (510) 388-2785. We thank Walid Badawi and Matthew Haarer for superb research assistance. “CABINETS, in France, may come and Cabinets may go, but the economic crisis seems to go on for ever.” - The Economist, 2/5/1938, p. -

New Deal for Consumers
New Deal For Consumers Legal Affairs Committee Rom, 4 October 2018 New Deal For Consumers Proposals for two directives of the European Parliament and of the Council: 1. Directive on representative actions for the protection of the collective interests of consumers and amending Directive 2009/22/EC (Speaker: Ms. Freise, VdpB) 2. Directive introducing targeted amendments to EU consumer law Directives (Speaker: Ms. Holler, EFBS) 2 © European Federation of Building Societies Directive on Representative Actions Reasons for the proposal ▪ Resolution of the European Parliament “Towards a Coherent European Approach to Collective Redress” (2012) ▪ Recommendation 2013/396/EU of the European Commission on common principles for injunctive and compensatory collective redress mechanisms in the Member States (2013) ▪ REFIT Fitness Check of EU consumer and marketing law (2017) ▪ Report of the European Commission on the implementation of concerning violations of rights granted under Union Law (2018) Need for collective compensatory redress mechanisms Replacement of the Directive 2009/22/EC 3 © European Federation of Building Societies Directive on Representative Actions Subject matter of the proposal “This Directive sets out rules enabling qualified entities to seek representative actions aimed at the protection of the collective interests of consumers, while ensuring appropriate safeguards to avoid abusive litigation.” 4 © European Federation of Building Societies Directive on Representative Actions Subject matter of the proposal 1. Qualified entities 2. Possible representative actions 3. Safeguards to avoid abusive litigation 5 © European Federation of Building Societies Directive on Representative Actions 1. Qualified Entities Proposal: - legitimate interest in ensuring that provisions of Union law are complied with - non-profit making character - sufficient financial resources in particular: consumer organisations and independent public bodies Any qualified entity may apply to the courts or administrative authorities of another Member State. -
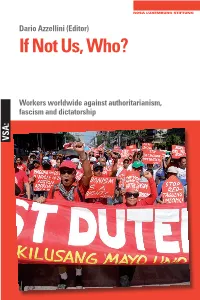
If Not Us, Who?
Dario Azzellini (Editor) If Not Us, Who? Workers worldwide against authoritarianism, fascism and dictatorship VSA: Dario Azzellini (ed.) If Not Us, Who? Global workers against authoritarianism, fascism, and dictatorships The Editor Dario Azzellini is Professor of Development Studies at the Universidad Autónoma de Zacatecas in Mexico, and visiting scholar at Cornell University in the USA. He has conducted research into social transformation processes for more than 25 years. His primary research interests are industrial sociol- ogy and the sociology of labour, local and workers’ self-management, and so- cial movements and protest, with a focus on South America and Europe. He has published more than 20 books, 11 films, and a multitude of academic ar- ticles, many of which have been translated into a variety of languages. Among them are Vom Protest zum sozialen Prozess: Betriebsbesetzungen und Arbei ten in Selbstverwaltung (VSA 2018) and The Class Strikes Back: SelfOrganised Workers’ Struggles in the TwentyFirst Century (Haymarket 2019). Further in- formation can be found at www.azzellini.net. Dario Azzellini (ed.) If Not Us, Who? Global workers against authoritarianism, fascism, and dictatorships A publication by the Rosa-Luxemburg-Stiftung VSA: Verlag Hamburg www.vsa-verlag.de www.rosalux.de This publication was financially supported by the Rosa-Luxemburg-Stiftung with funds from the Ministry for Economic Cooperation and Development (BMZ) of the Federal Republic of Germany. The publishers are solely respon- sible for the content of this publication; the opinions presented here do not reflect the position of the funders. Translations into English: Adrian Wilding (chapter 2) Translations by Gegensatz Translation Collective: Markus Fiebig (chapter 30), Louise Pain (chapter 1/4/21/28/29, CVs, cover text) Translation copy editing: Marty Hiatt English copy editing: Marty Hiatt Proofreading and editing: Dario Azzellini This work is licensed under a Creative Commons Attribution–Non- Commercial–NoDerivs 3.0 Germany License. -

Spice Brexit Update
SPICe: Brexit update paper Issue 87 30 May BREXI T UPDATE 2019 Scottish Parliament Information Centre Written by Iain McIver SPICe Research, The Scottish Parliament 1 SPICe: Brexit update paper Contents INTRODUCTION 2 CONTEXT 2 EUROPEAN UNION (WITHDRAWAL AGREEMENT) BILL 2 THE PRIME MINISTER’S NEW OFFER 3 EUROPEAN PARLIAMENT ELECTIONS 5 COMMON FRAMEWORKS: 3RD REPORT ON “FREEZING POWERS” 6 Photo copyright © The Scottish Parliamentary Corporate Body INTRODUCTION This SPICe Brexit Update #87 provides a review of the last two weeks during which the Prime Minister indicated she planned to bring forward the Withdrawal Agreement Bill in the UK Parliament before then announcing she was stepping down as leader of the Conservative Party. The update also includes a summary of the European Parliament elections which took place in the UK on 23 May. CONTEXT At the European Council meeting on 10 April, the UK requested a second extension to the Article 50 period, this resulted in a flexible extension to 31 October 2019. The extension was designed to allow the UK Government to find a way to ensure the UK can leave the EU with a ratified Withdrawal Agreement. If the Withdrawal Agreement is ratified before October, the UK will leave the EU at the end of the month in which the Agreement is ratified. As a result of the extension to the Article 50 period, the UK was required to participate in the European Parliament elections on 23 May. EUROPEAN UNION (WITHDRAWAL AGREEMENT) BILL With the UK Government failing to secure the consent of the House of Commons through the meaningful vote process, the UK Government planned to change tack by introducing the legislation necessary to implement the contents of the Withdrawal Agreement into UK law.