Development of Intervention Package Among Main Care-Givers Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

University of Yangon Department of Anthropology
UNIVERSITY OF YANGON DEPARTMENT OF ANTHROPOLOGY EDUCATION AND HEALTH EDUCATION IN SITPINQUIN VILLAGE THANLYIN TOWNSHIP, YANGON SOE MOE NAiNG M.A. Antb.6 (2009-2010) YANGON MAY,20tO UNIVERSITY OF YANGON DEPARTMENT OF ANTHROPOLOGY EDUCATION AND HEALTH EDUCATION IN SITPINQUIN VILLAGE THANLYINTOWNSHIP, YANGON SOE MOE NAING M.A. Anth.6 (2009-2010) YANGON MAY,2010 UNIVERSITY OF YANGON DEPARTMENT OF ANTHROPOLOGY EDUCATION AND HEALTH EDUCAnON IN SITPINQUIN VILLAGE THANLYIN TOWNSHIP, YANGON Research Thesis is submitted for Master Degree in Anthropology Submitted By SOE MOE NAING M.A. Anth.6 ( 2009- 2010 ) YANGON 2010 EDUCATION AND HEALTH EDUCATION IN SITPINQUIN VILLAGE THANLYIN TOWNSHIP, YANGON EDUCATION AND HEALTH EDUCATION IN SITPINQUIN VILLAGE THANLYINTOWNSHlP, YANGON SOE MOE NAING M.A. Anth.6 ( 2009- 2010 ) Master Degree in Anthropology Department of Anthropology May. 2010 proved by Board of Examiners -.1:fl'-"'J'G k,J ~D:p\(\'" ............~~~. .. .... .... .. ?f.l~ . Chairperson External Examiner (Mya Mya Khln.Dr.] ( Myint Myint Aye) Associate Professor/Head Lecturer! Head Departmentof Anthropology Department ofAnthropology University ofYangon University of Dagon Supervisor Co-supervisor ( Mya Thidar Aung) ( Zin Mar Latt ) Department of Anthropology Department ofAnthropology University of Yangon University of Yangon Contents No. Particular Page Acknowledgements Abstract Key words Introduction Chapter (I) Research Methodology Data Collection 0). Key Informant Interview (ii). Interview (iii). Focus Group Interview Data Analysis 2 Chapter (II) Background Research Area 3 (I). History of Sitpinquin Village 3 (2). Geographical Selling 4 (3). Communication and Transportation 4 (4). Population 5 (5). Pattern ofHousing 6 (6). Operational Definition 6 Chapter (tIl) Education 8 (1). Local Perception on Education 8 (2). -

A Strategic Urban Development Plan of Greater Yangon
A Strategic A Japan International Cooperation Agency (JICA) Yangon City Development Committee (YCDC) UrbanDevelopment Plan of Greater The Republic of the Union of Myanmar A Strategic Urban Development Plan of Greater Yangon The Project for the Strategic Urban Development Plan of the Greater Yangon Yangon FINAL REPORT I Part-I: The Current Conditions FINAL REPORT I FINAL Part - I:The Current Conditions April 2013 Nippon Koei Co., Ltd. NJS Consultants Co., Ltd. YACHIYO Engineering Co., Ltd. International Development Center of Japan Inc. Asia Air Survey Co., Ltd. 2013 April ALMEC Corporation JICA EI JR 13-132 N 0 300km 0 20km INDIA CHINA Yangon Region BANGLADESH MYANMAR LAOS Taikkyi T.S. Yangon Region Greater Yangon THAILAND Hmawbi T.S. Hlegu T.S. Htantabin T.S. Yangon City Kayan T.S. 20km 30km Twantay T.S. Thanlyin T.S. Thongwa T.S. Thilawa Port & SEZ Planning調査対象地域 Area Kyauktan T.S. Kawhmu T.S. Kungyangon T.S. 調査対象地域Greater Yangon (Yangon City and Periphery 6 Townships) ヤンゴン地域Yangon Region Planning調査対象位置図 Area ヤンゴン市Yangon City The Project for the Strategic Urban Development Plan of the Greater Yangon Final Report I The Project for The Strategic Urban Development Plan of the Greater Yangon Final Report I < Part-I: The Current Conditions > The Final Report I consists of three parts as shown below, and this is Part-I. 1. Part-I: The Current Conditions 2. Part-II: The Master Plan 3. Part-III: Appendix TABLE OF CONTENTS Page < Part-I: The Current Conditions > CHAPTER 1: Introduction 1.1 Background ............................................................................................................... 1-1 1.2 Objectives .................................................................................................................. 1-1 1.3 Study Period ............................................................................................................. -

THE STATE of LOCAL GOVERNANCE: TRENDS in YANGON Photo Credits
Local Governance Mapping THE STATE OF LOCAL GOVERNANCE: TRENDS IN YANGON Photo credits Yangon Heritage Trust Thomas Schaffner (bottom photo on cover and left of executive summary) Gerhard van ‘t Land Susanne Kempel Myanmar Survey Research The views expressed in this publication are those of the author, and do not necessarily represent the views of UNDP. Local Governance Mapping THE STATE OF LOCAL GOVERNANCE: TRENDS IN YANGON UNDP MYANMAR Table of Contents Acknowledgements II Acronyms III Executive Summary 1 - 4 1. Introduction to the Local Governance Mapping 5 - 8 1.1 Yangon Region - most striking features 7 1.2 Yangon City Development Committee and the Region government 8 1.3 Objectives of the report and its structure 8 2. Descriptive overview of governance structures in Yangon Region 9 - 38 2.1 Yangon Region - administrative division 11 2.2 Yangon Region - Socio-economic and historical context 13 2.3 Yangon City Development Committee (YCDC) 18 2.4 Yangon Region Government 24 2.5 Representation of Yangon Region in the Union Hluttaws 33 2.6 Some of the governance issues that Yangon Region and YCDC are facing 37 3. Organisation of service delivery at the township level 39 - 62 3.1 Governance structures at the township level 43 3.2 Planning and Budgeting 46 3.3 Role of GAD and the VTAs/WAs 48 3.4 The TDSC and the TMAC 51 3.5 Election and selection processes for peoples’ representatives 53 3.6 Three concrete services - people’s participation and providers views 54 3.7 Major development issues from a service provider perspective 60 4. -

Permitted Enterprises by Myanmar Investment Commission (1/2021)
Permitted Enterprises by Myanmar Investment Commission (1/2021) No Name of Location Type of Investment Form of Date of issue Remark Company Business Investment 1 Myanmar C.P. Holding No. 134, 140, 141/1, 141/2, Pig Farming and Wholly (1/2021) Livestock Co., Ltd. 143,144, Kwin No. 310, Zee Taw (East) Kwin, Sales of Pigs Foreign 27-1-2021 Zee Taw Village Tract, Budalin Township, Owned Myanmar Monywa District, Sagaing Region Investment Commission 2 Myanmar C.P. Holding No. 2/2, 2/3, 2/4, 3/1, 3/2, 3/3, 3/4, 3/5, Pig Farming and Wholly (1/2021) Livestock Co., Ltd. 3/6, 3/7, 3/8, Kwin No. 1428 (Thi Pin Kan), Myin Sales of Pigs Foreign 27-1-2021 Saing Village Tract, Tada-U Township, Kyauk Owned Myanmar Sae District, Mandalay Region Investment Commission 3 Scoular Myanmar Plot No. (83, 84), Myay Taing Block No. Production and Wholly (1/2021) Co., Ltd. Thilawa Industrial Zone, Thanlyin- Distribution of Fish Foreign 27-1-2021 Kyauktan Township, Yangon Region Meal Owned Myanmar Investment Commission 4 Singha Myanmar Plot No. (40), (40, 59/ ,61/2), (82ka+ Manufacturing and Joint (1/2021) Limited 82kha/2), (82-Gha), (88+89), (40/3, 60, 60/1), Distributing of Beer Venture 27-1-2021 Myay Taing Block No. 20-Ka/ Inya, Plot No. and Non-Alcoholic (82 Ka + 82 Kha/2), (82-Gha), Myay Taing Beverages Block No. 20 Ka, Palate Village tract, Sintkai Myanmar Township, Kyaukse District, Mandalay Investment Region Commission 5 Myanmar Holding No.9Kha, 27F, 28F,29F,34F,28, Kwin Manufacturing and Joint (1/2021) Tsuyatomo Co., No.410, Phoe Thein Tan Kwin, Thayattaw Marketing of Venture 27-1-2021 Ltd. -

Powerful Countries Interferring in Internal Affairs of Others Young Generation Are Duty-Bound to Safeguard Independence and Sovereignty
Established 1914 Volume XIV, Number 263 2nd Waning of Pyatho 1368 ME Thursday, 4 January, 2007 Powerful countries interferring in internal affairs of others Young generation are duty-bound to safeguard independence and sovereignty NAY PYI TAW, 4 Jan—The following is a trans- of the Union and sovereignty. the national people have stood tall and well realized lation of the message sent by Chairman of the State In the course of the history, Myanmar has stood tall the value and taste of independence throughout the Peace and Development Council Commander-in- as an independent and sovereign nation with own periods. Chief of Defence Services Senior General Than monarchs in the world. Since time immemorial, the In the late 19th Century, Myanmar fell under Shwe on the occasion of the 59th Anniversary of the national races have been living in the Union in amity alien subjugation and lost its sovereignty and inde- Independence Day for 2007. through thick and thin. pendence. However, Myanmar people are fully On this auspicious occasion of the 59th Anni- Throughout the history, Myanmar has been a un- equipped with the spirit of cherishing and valuing versary of the Independence Day of the Union of ion where multicultural national races have made their their motherland, the people, sovereignty, litera- Myanmar, I would like to extend my greetings to all home in unity and harmony since prehistoric times. ture, culture and traditions of their own, the prepar- the national people in the nation, with amity and The history of the Union of Myanmar is that of the edness to make sacrifices for the nation and the high esteem. -

Hlegu) Industrial Park Project - Located at Hlaeku Township - Jointly Developed by the Myanmar – Singapore , Has a Total Area of 1150 Acres ( 465 Hta
Outlines Why Invest in Yangon? Investment Environment in Yangon Mega Projects in Yangon Yangon Region Investment Committee 2 YANGON Heritage. Green. Livable. Commercial Region of Myanmar 3 „We are very ambitious to develop the Yangon region rapidly and create a city where sustainable economic development. We will try to create a Yangon that will be a vitally important city, not only for Myanmar but also for ASEAN countries. We are creating enabling investment environment to promote investment in Yangon Region‟ Chief Minister Yangon Region Government 4 Why Invest in Yangon ? Strong Economic Factors GDP 24 % GDP Growth Rate 9.8 % Manufacturing Sector 41% Trade Sector 28% Services Sector 29% Construction Sector 25% Electric Power Sector 22% Yangon City Working Population 70% Smallest Region 10,171 sq km Population 7.4 mil ( Yangon Region) Strategic Urban Development Plan of Greater Yangon 6 YANGON ACCOUNTS FOR - CLOSE TO 85 % OF THE COUNTRY’S TRADE - OVER HALF OF THE TOTAL INVESTMENTS INTO THE COUNTRY 7 “Yangon Region” : Investment Hub in Myanmar 8 Mission To Attain Green Growth Economy of Yangon Region by Promoting Responsible and Quality Investment 9 Investment Priority Sectors Manufacturing Sector • Export Promotion Industries • Import Substitution Industries Infrastructure Sector • Power Generation, Transmission and Distribution • Construction of affordable Housing • Industrial Estate • Construction of Seaport, River Port and Dry Port • Construction of Road, Bridge and Railway Line • City Development Activities Information -

Project on Construction of Solid Waste Management Facilities in the Thilawa Sez Zone A
PROJECT ON CONSTRUCTION OF SOLID WASTE MANAGEMENT FACILITIES IN THE THILAWA SEZ ZONE A FINAL ENVIRONMENTAL IMPACT ASSESSMENT REPORT June 2015 GOLDEN DOWA ECO-SYSTEM MYANMAR CO., LTD. Project Site Project Location Map Ministry of Environmental Conservation and Forestry Office No. (28), Ottrathiri Township Nay Pyi Taw, Myanmar Attention: His Excellency Mr. Win Tun Union Minister Ministry of Environmental Conservation and Forestry Subject: Environmental Impact Assessment (EIA) Report in respect of the “Construction of Solid Waste Management Facilities in Thilawa SEZ Zone A” Project (the EIA report including Environmental Management Plan (EMP)) Dear Sir, We refer to the captioned EIA report, which was prepared and finalized by Nippon Koei Co., Ltd., which is an EIA consulting company as the third party, in accordance with Environmental Conservation Law, Rules and Procedures under the instruction of the Ministry of Environmental Conservation and Forestry and formally submitted to the Ministry of Environmental Conservation and Forestry. Intending to be legally bound hereby and financially liable to the Ministry of Environmental Conservation and Forestry here under, we: a. Endorse and confirm to the Ministry of Environmental Conservation and Forestry the accuracy and completeness of the EIA. b. Confirm and undertake to the Ministry of Environmental Conservation and Forestry that the EIA has been prepared in strict compliance with applicable laws, rules, regulations and procedures including Environmental Conservation Law, Rules and Procedures. -

Khin Htar Nwe EMPA.Pdf (591
YANGON UNIVERSITY OF ECONOMICS MASTER OF PUBLIC ADMINISTRATION PROGRAMME A STUDY ON LAND ADMINISTRATION OF THE GENERAL ADMINISTRATION DEPARTMENT IN THANLYIN AND KYAUKTAN TOWNSHIPS, YANGON REGION KHIN HTAR NWE EMPA –18 (14th Batch) AUGUST, 2018 1 YANGON UNIVERSITY OF ECONOMICS MASTER OF PUBLIC ADMINISTRATION PROGRAMME A STUDY ON LAND ADMINISTRATION OF THE GENERAL ADMINISTRATION DEPARTMENT IN THANLYIN AND KYAUKTAN TOWNSHIPS, YANGON REGION A thesis submitted as a partial fulfillment towards the requirements for the degree of Master of Public Administration (MPA) Supervised by Submitted by Daw Sintheingie Khin Htar Nwe Professor/head (Retd.) Roll No. 18 Department of Economics EMPA 14th Batch Yangon University of Economics 2015-2018 AUGUST, 2018 2 YANGON UNIVERSITY OF ECONOMICS MASTER OF PUBLIC ADMINISTRATION PROGRAMME This is certify that this thesis entitled: A Study On Land Administration Of The General Administration Department In Thanlyin And Kyauktan Townships, Yangon Region submitted as a partial fulfillment towards the requirements for the degree of Master of Public Administration has been accepted by the Board of Examiners. Board of Examiners 1. Professor Dr. Tun Aung Pro-Rector Yangon University of Economics (Chief Examiner) 2. Professor Dr. Daw Ni Lar Myint Htoo Pro-Rector Yangon University of Economics (Examiner) 3. Professor Dr. Kyaw Min Htun Pro-Rector (Retd.) Yangon University of Economics (Examiner) 4. Professor Dr. Phyu Phyu Ei Programme Director and Head of Department Department of Applied Economics Yangon University of Economics (Examiner) 5. U Thein Naing Associate Professor Department of Applied Economics Yangon University of Economics (Examiner) August, 2018 3 ABSTRACT This study focuses on Land Administration of the General Administration Department in Thanlyin and Kyauktan Townships, which is located in Thilawa SEZ for the period 2007 - 2017. -

Permitted Enterprises by Myanmar Investment Commission (4/2020) No Name of Company Location Type of Investment Business Form Of
1 Permitted Enterprises by Myanmar Investment Commission (4/2020) Type of Investment Form of No Name of Company Location Date of issue Remark business Investment 1 HDDES Natural Plot No. 121/ 123, Thilawa Processing and Sales of Joint Venture (4/2020) Products (Myanmar) Industrial Zone, Thanlyin- Value added Agricultural Investment 6-3-2020 Limited Kyauktan Township, Yangon Products Myanmar Region Investment Commission 2 Bel Ga Myanmar Holding No. 26, Kwin No. Broiler Chick Parent Wholly Foreign (4/2020) Limited OSS/72, Kyay Taing Pyin Stock Farm Owned 6-3-2020 Kwin, Sitpinseik Village Myanmar Tract, Bago Township, Investment Bago District, Bago Region Commission 3 Dongfeng Motor Plot No.147, Myay Taing Assembling, Wholly (4/2020) Corporation Limited Block No. Thilawa Industrial manufacturing, and Sales Myanmar 6-3-2020 Zone Thanlyin-Kyat Tan of Motor Vehicles Owned Myanmar Township, Yangon Region Investment Commission 4 MCV Terminal Thilawa Port Area, Plot No.14, construction of LNG Joint Venture (4/2020) Limited Kyauk Tan Township, Yangon, terminal, providing 6-3-2020 17 Acres out of 82.61 Acres services of FSU berthing, Myanmar regasification for LNG Investment power plant Commission 2 Type of Investment Form of No Name of Company Location Date of issue Remark business Investment 5 Proficient Education No.5, Say Yone Street, Ward- special education Joint Venture (4/2020) Company Limited 16, Yankin Township, Yangon services 6-3-2020 Region Myanmar Investment Commission 6 Zwe Ka Bin Land & Holding No-16/1, 20/1, Field cable car services Wholly Myanmar (4/2020) Cable Car No-OSS-66, Htamalout Kyay Owned 6-3-2020 Development Taing Pyin Kwin, Taw Pone Myanmar Company Limited Village Tract, Hpa-an Investment Township, Hpa-an District, Kayin State And Zwekabin Commission Reserved Forest It created (2850) job opportunities from permitted enterprises by Myanmar Investment Commission meeting (4/2020). -
Zone Notification
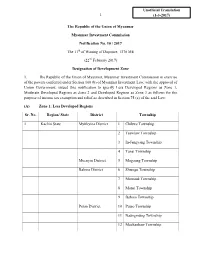
Unofficial Translation 1 (1-3-2017) The Republic of the Union of Myanmar Myanmar Investment Commission Notification No. 10 / 2017 The 11th of Waning of Dapotwe, 1378 ME (22nd February 2017) Designation of Development Zone 1. The Republic of the Union of Myanmar, Myanmar Investment Commission in exercise of the powers conferred under Section 100 (b) of Myanmar Investment Law, with the approval of Union Government, issued this notification to specify Less Developed Regions as Zone 1, Moderate Developed Regions as Zone 2 and Developed Regions as Zone 3 as follows for the purpose of income tax exemption and relief as described in Section 75 (a) of the said Law: (A) Zone 1: Less Developed Regions Sr. No. Region/ State District Township 1 Kachin State Myitkyina District 1 Chibwe Township 2 Tsawlaw Township 3 In-Jangyang Township 4 Tanai Township Moenyin District 5 Mogaung Township Bahmo District 6 Shwegu Township 7 Momauk Township 8 Mansi Township 9 Bahmo Township Putao District 10 Putao Township 11 Naungmung Township 12 Machanbaw Township 2 13 Sumprabum Township 14 Kaunglanhpu Township 2 Kayah State Bawlakhe District 1 BawlakheTownship 2 Hpasaung Township 3 Mese Township Loikaw District 4 Loikaw Township 5 Demawso Township 6 Hpruso Township 7 Shataw Township 3 Kayin State Hpa-an District 1 Hpa-an Township 2 Hlaignbwe Township 3 Papun Township 4 Thandaunggyi Township Kawkareik District 5 Kawkareik Township 6 Kyain Seikkyi Township Myawady District 7 Myawady Township 4 Chin State Falam District 1 Falam Township 2 Tiddim Township 3 Hton Zan Township -

Cho Kay Khine Soe Eco..Pdf (609.8
YANGON UNIVERSITY OF ECONOMICS DEPARTMENT OF ECONOMICS MASTER OF ECONOMICS A STUDY ON RURAL ROAD INFRASTRUCTURE DEVELOPMENT IN MYANMAR (CASE STUDY IN KYAUKTAN TOWNSHIP) CHO KAY KHINE SOE SEPTEMBER, 2019 1 YANGON UNIVERSITY OF ECONOMICS DEPARTMENT OF ECONOMICS MASTER OF ECONOMICS A STUDY ON RURAL ROAD INFRASTRUCTURE DEVELOPMENT IN MYANMAR (CASE STUDY IN KYAUKTAN TOWNSHIP) A thesis submitted as a partial fulfillment of the requirements for the degree of Master of Economics, MEcon (Economics) Supervised by Submitted by Daw Kyi Kyi Win Cho Kay Khine Soe Lecturer Roll No. 14 Department of Economics MEcon (Economics) Yangon University of Economics SEPTEMBER, 2019 2 YANGON UNIVERSITY OF ECONOMICS DEPARTMENT OF ECONOMICS MASTER OF ECONOMICS This is to certify that this thesis entitled “A STUDY ON RURAL ROAD INFRASTRUCTURE DEVELOPMENT IN MYANMAR (CASE STUDY IN KYAUKTAN TOWNSHIP)” submitted as a partial fulfillment towards the requirements for the degree of Master of Economics, has been accepted by the Board of Examiners. BOARD OF EXAMINERS 1. Dr. Tin Win Rector Yangon University of Economics (Chief Examiner) 2. Dr. Ni Lar Myint Htoo Pro-Rector Yangon University of Economics (Examiner) 3. Dr. Cho Cho Thein Professor and Head Department of Economics Yangon University of Economics (Examiner) 4. Dr. Khin Thida Nyein Professor Department of Economics Yangon University of Economics (Examiner) 5. Dr. Tha Pye Nyo Professor Department of Economics Yangon University of Economics (Examiner) SEPTEMBER, 2019 3 ABSTRACT Infrastructure plays a very important role in supporting nation’s economic development. Improvement in rural road connectivity not only assures the development but also accelerate the process of development of a region. -

List of Townships of Burma
State/ Region Name of District Township Central Burma Magway Region Gangaw District Gangaw Township Central Burma Magway Region Gangaw District Tilin Township Central Burma Magway Region Gangaw District Saw Township Central Burma Magway Region Magway District Magway Township Central Burma Magway Region Magway District Yenangyaung Township Central Burma Magway Region Magway District Chauck Township Central Burma Magway Region Magway District Taungdwingyi Township Central Burma Magway Region Magway District Myothit Township Central Burma Magway Region Magway District Natmauk Township Central Burma Magway Region Minbu District Minbu Township Central Burma Magway Region Minbu District Pwintbyu Township Central Burma Magway Region Minbu District Ngape Township Central Burma Magway Region Minbu District Salin Township Central Burma Magway Region Minbu District Sidoktaya Township Central Burma Magway Region Pakokku District Myaing Township Central Burma Magway Region Pakokku District Pakokku Township Central Burma Magway Region Pakokku District Pauk Township Central Burma Magway Region Pakokku District Seikphyu Township Central Burma Magway Region Pakokku District Yesagyo Township Central Burma Magway Region Thayet District Aunglan Township Central Burma Magway Region Thayet District Kamma Township Central Burma Magway Region Thayet District Mindon Township Central Burma Magway Region Thayet District Minhla Township Central Burma Magway Region Thayet District Sinbaungwe Township Central Burma Magway Region Thayet District Thayet Township Central