Abstract Introduction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Estimated Burden of Serious Fungal Infections in Ghana
Journal of Fungi Article Estimated Burden of Serious Fungal Infections in Ghana Bright K. Ocansey 1, George A. Pesewu 2,*, Francis S. Codjoe 2, Samuel Osei-Djarbeng 3, Patrick K. Feglo 4 and David W. Denning 5 1 Laboratory Unit, New Hope Specialist Hospital, Aflao 00233, Ghana; [email protected] 2 Department of Medical Laboratory Sciences, School of Biomedical and Allied Health Sciences, College of Health Sciences, University of Ghana, P.O. Box KB-143, Korle-Bu, Accra 00233, Ghana; [email protected] 3 Department of Pharmaceutical Sciences, Faculty of Health Sciences, Kumasi Technical University, P.O. Box 854, Kumasi 00233, Ghana; [email protected] 4 Department of Clinical Microbiology, School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi 00233, Ghana; [email protected] 5 National Aspergillosis Centre, Wythenshawe Hospital and the University of Manchester, Manchester M23 9LT, UK; [email protected] * Correspondence: [email protected] or [email protected] or [email protected]; Tel.: +233-277-301-300; Fax: +233-240-190-737 Received: 5 March 2019; Accepted: 14 April 2019; Published: 11 May 2019 Abstract: Fungal infections are increasingly becoming common and yet often neglected in developing countries. Information on the burden of these infections is important for improved patient outcomes. The burden of serious fungal infections in Ghana is unknown. We aimed to estimate this burden. Using local, regional, or global data and estimates of population and at-risk groups, deterministic modelling was employed to estimate national incidence or prevalence. Our study revealed that about 4% of Ghanaians suffer from serious fungal infections yearly, with over 35,000 affected by life-threatening invasive fungal infections. -

Fungal Infections from Human and Animal Contact
Journal of Patient-Centered Research and Reviews Volume 4 Issue 2 Article 4 4-25-2017 Fungal Infections From Human and Animal Contact Dennis J. Baumgardner Follow this and additional works at: https://aurora.org/jpcrr Part of the Bacterial Infections and Mycoses Commons, Infectious Disease Commons, and the Skin and Connective Tissue Diseases Commons Recommended Citation Baumgardner DJ. Fungal infections from human and animal contact. J Patient Cent Res Rev. 2017;4:78-89. doi: 10.17294/2330-0698.1418 Published quarterly by Midwest-based health system Advocate Aurora Health and indexed in PubMed Central, the Journal of Patient-Centered Research and Reviews (JPCRR) is an open access, peer-reviewed medical journal focused on disseminating scholarly works devoted to improving patient-centered care practices, health outcomes, and the patient experience. REVIEW Fungal Infections From Human and Animal Contact Dennis J. Baumgardner, MD Aurora University of Wisconsin Medical Group, Aurora Health Care, Milwaukee, WI; Department of Family Medicine and Community Health, University of Wisconsin School of Medicine and Public Health, Madison, WI; Center for Urban Population Health, Milwaukee, WI Abstract Fungal infections in humans resulting from human or animal contact are relatively uncommon, but they include a significant proportion of dermatophyte infections. Some of the most commonly encountered diseases of the integument are dermatomycoses. Human or animal contact may be the source of all types of tinea infections, occasional candidal infections, and some other types of superficial or deep fungal infections. This narrative review focuses on the epidemiology, clinical features, diagnosis and treatment of anthropophilic dermatophyte infections primarily found in North America. -

Introduction to Bacteriology and Bacterial Structure/Function
INTRODUCTION TO BACTERIOLOGY AND BACTERIAL STRUCTURE/FUNCTION LEARNING OBJECTIVES To describe historical landmarks of medical microbiology To describe Koch’s Postulates To describe the characteristic structures and chemical nature of cellular constituents that distinguish eukaryotic and prokaryotic cells To describe chemical, structural, and functional components of the bacterial cytoplasmic and outer membranes, cell wall and surface appendages To name the general structures, and polymers that make up bacterial cell walls To explain the differences between gram negative and gram positive cells To describe the chemical composition, function and serological classification as H antigen of bacterial flagella and how they differ from flagella of eucaryotic cells To describe the chemical composition and function of pili To explain the unique chemical composition of bacterial spores To list medically relevant bacteria that form spores To explain the function of spores in terms of chemical and heat resistance To describe characteristics of different types of membrane transport To describe the exact cellular location and serological classification as O antigen of Lipopolysaccharide (LPS) To explain how the structure of LPS confers antigenic specificity and toxicity To describe the exact cellular location of Lipid A To explain the term endotoxin in terms of its chemical composition and location in bacterial cells INTRODUCTION TO BACTERIOLOGY 1. Two main threads in the history of bacteriology: 1) the natural history of bacteria and 2) the contagious nature of infectious diseases, were united in the latter half of the 19th century. During that period many of the bacteria that cause human disease were identified and characterized. 2. Individual bacteria were first observed microscopically by Antony van Leeuwenhoek at the end of the 17th century. -

Boards' Fodder
boards’ fodder Medical Mycology By Adriana Schmidt, MD, and Natalie M. Curcio, MD, MPH. (Updated July 2015*) SUPERFICIAL ORGANISM CLINICAL HISTO/KOH TREATMENT MYCOSES* Pityriasis Malessezia furfur Hypo- or hyper-pigmented Spaghetti & meatballs: Antifungal shampoos and/or versicolor macules short hyphae + yeast PO therapy Tinea nigra Hortaea werneckii (formerly Brown-black non-scaly Branching septate hyphae Topical imidazoles or palmaris Phaeoannellomyces werneckii) macules + budding yeast allylamines Black piedra Piedraia hortae Hard firm black Dark hyphae around concretions acrospores Cut hair off, PO terbinafine, White piedra Trichosporon ovoides or inkin Soft loose white Blastoconidia, imidazoles, or triazoles (formely beigelii) concretions arthroconidia Fluorescent small Microsporum Canis KOH: spores on outside spore ectothrix: M. audouinii of the hair shaft; “Cats And Dogs M. distortum Wood’s lamp --> yellow Sometimes Fight T. schoenleinii fluorescence & Growl” M. ferrugineum+/- gypseum Large spore Trichophyton spp. (T. tonsurans in North America; T. violaceum in KOH: spores within hair Topical antifungals; PO endothrix Europe, Asia, parts of Africa). shaft antifungals for T. manuum, Tinea corporis T. rubrum > T. mentag. Majocchi’s granuloma: T. rubrum capitis, unguium T. pedis Moccasin: T. rubrum, E. floccosum. Interdigital/vesicular: T. mentag T. unguium Distal lateral, proximal and proximal white subungual: T. rubrum. White superficial: T. mentag. HIV: T. rubrum SUBQ MYCOSES** ORGANISM TRANSMISSION CLINICAL HISTO/KOH TREATMENT -

Tinea Capitis 2014 L.C
BJD GUIDELINES British Journal of Dermatology British Association of Dermatologists’ guidelines for the management of tinea capitis 2014 L.C. Fuller,1 R.C. Barton,2 M.F. Mohd Mustapa,3 L.E. Proudfoot,4 S.P. Punjabi5 and E.M. Higgins6 1Department of Dermatology, Chelsea & Westminster Hospital, Fulham Road, London SW10 9NH, U.K. 2Department of Microbiology, Leeds General Infirmary, Leeds LS1 3EX, U.K. 3British Association of Dermatologists, Willan House, 4 Fitzroy Square, London W1T 5HQ, U.K. 4St John’s Institute of Dermatology, Guy’s and St Thomas’ NHS Foundation Trust, St Thomas’ Hospital, Westminster Bridge Road, London SE1 7EH, U.K. 5Department of Dermatology, Hammersmith Hospital, 150 Du Cane Road, London W12 0HS, U.K. 6Department of Dermatology, King’s College Hospital, Denmark Hill, London SE5 9RS, U.K. 1.0 Purpose and scope Correspondence Claire Fuller. The overall objective of this guideline is to provide up-to- E-mail: [email protected] date, evidence-based recommendations for the management of tinea capitis. This document aims to update and expand Accepted for publication on the previous guidelines by (i) offering an appraisal of 8 June 2014 all relevant literature since January 1999, focusing on any key developments; (ii) addressing important, practical clini- Funding sources cal questions relating to the primary guideline objective, i.e. None. accurate diagnosis and identification of cases; suitable treat- ment to minimize duration of disease, discomfort and scar- Conflicts of interest ring; and limiting spread among other members of the L.C.F. has received sponsorship to attend conferences from Almirall, Janssen and LEO Pharma (nonspecific); has acted as a consultant for Alliance Pharma (nonspe- community; (iii) providing guideline recommendations and, cific); and has legal representation for L’Oreal U.K. -

Tinea Capitis: Unusual Chronic Presentation in an Elderly Woman
ISSN: 2474-3658 Salazar et al. J Infect Dis Epidemiol 2018, 4:048 DOI: 10.23937/2474-3658/1510048 Volume 4 | Issue 1 Journal of Open Access Infectious Diseases and Epidemiology CASE REPORT Tinea Capitis: Unusual Chronic Presentation in an Elderly Woman Elizabeth Salazar1*, Daniel Asz-Sigall2, Diana Vega3 and Roberto Arenas4 1Dermato-Oncologist, Private Practice, Mexico City, Mexico 2 Check for Dermatologist, Dermato-Oncology and Trichology Clinic, National University of Mexico, Mexico City, Mexico updates 3Mycologist, Mycology Section, Hospital General “Dr. Manuel Gea González”, Mexico City, Mexico 4Dermatologist and Mycologist, Mycology Section, General Hospital “Dr. Manuel Gea González”, Mexico City, Mexico *Corresponding authors: Elizabeth Salazar, Dermato-Oncologist, Private Practice, Mexico City, Mexico, E-mail: dra. [email protected] The non-inflammatory clinical presentation can be Abstract found in 90% of affected children. It is more frequent in Tinea capitis is a superficial fungal infection of the scalp tropical regions with low socioeconomic conditions and and hair caused by dermatophytes such as Trichophyton and Microsporum. Tinea capitis is very rare in adults, and affects almost exclusively children (98%). The inflamma- may affect those with immunosuppressive diseases or tory form is observed only in 10% and most commonly menopausal elderly women. Clinical manifestations along seen in prepubescent children. Tinea capitis is caused with trichoscopy and Wood’s light, can help the clinician to by dermatophytes that use keratin as a nutrient source. determine the correct diagnosis, in order to reduce irrevers- Scalp erythema, scaling, and crusting are typical signs of ible sequelae and decrease multiple contagion. KOH direct exam and culture confirm diagnosis and aetiology. -

Geophilic Dermatophytes and Other Keratinophilic Fungi in the Nests of Wetland Birds
ACTA MyCoLoGICA Vol. 46 (1): 83–107 2011 Geophilic dermatophytes and other keratinophilic fungi in the nests of wetland birds Teresa KoRnIŁŁoWICz-Kowalska1, IGnacy KIToWSKI2 and HELEnA IGLIK1 1Department of Environmental Microbiology, Mycological Laboratory University of Life Sciences in Lublin Leszczyńskiego 7, PL-20-069 Lublin, [email protected] 2Department of zoology, University of Life Sciences in Lublin, Akademicka 13 PL-20-950 Lublin, [email protected] Korniłłowicz-Kowalska T., Kitowski I., Iglik H.: Geophilic dermatophytes and other keratinophilic fungi in the nests of wetland birds. Acta Mycol. 46 (1): 83–107, 2011. The frequency and species diversity of keratinophilic fungi in 38 nests of nine species of wetland birds were examined. nine species of geophilic dermatophytes and 13 Chrysosporium species were recorded. Ch. keratinophilum, which together with its teleomorph (Aphanoascus fulvescens) represented 53% of the keratinolytic mycobiota of the nests, was the most frequently observed species. Chrysosporium tropicum, Trichophyton terrestre and Microsporum gypseum populations were less widespread. The distribution of individual populations was not uniform and depended on physical and chemical properties of the nests (humidity, pH). Key words: Ascomycota, mitosporic fungi, Chrysosporium, occurrence, distribution INTRODUCTION Geophilic dermatophytes and species representing the Chrysosporium group (an arbitrary term) related to them are ecologically classified as keratinophilic fungi. Ke- ratinophilic fungi colonise keratin matter (feathers, hair, etc., animal remains) in the soil, on soil surface and in other natural environments. They are keratinolytic fungi physiologically specialised in decomposing native keratin. They fully solubilise na- tive keratin (chicken feathers) used as the only source of carbon and energy in liquid cultures after 70 to 126 days of growth (20°C) (Korniłłowicz-Kowalska 1997). -

Therapies for Common Cutaneous Fungal Infections
MedicineToday 2014; 15(6): 35-47 PEER REVIEWED FEATURE 2 CPD POINTS Therapies for common cutaneous fungal infections KENG-EE THAI MB BS(Hons), BMedSci(Hons), FACD Key points A practical approach to the diagnosis and treatment of common fungal • Fungal infection should infections of the skin and hair is provided. Topical antifungal therapies always be in the differential are effective and usually used as first-line therapy, with oral antifungals diagnosis of any scaly rash. being saved for recalcitrant infections. Treatment should be for several • Topical antifungal agents are typically adequate treatment weeks at least. for simple tinea. • Oral antifungal therapy may inea and yeast infections are among the dermatophytoses (tinea) and yeast infections be required for extensive most common diagnoses found in general and their differential diagnoses and treatments disease, fungal folliculitis and practice and dermatology. Although are then discussed (Table). tinea involving the face, hair- antifungal therapies are effective in these bearing areas, palms and T infections, an accurate diagnosis is required to ANTIFUNGAL THERAPIES soles. avoid misuse of these or other topical agents. Topical antifungal preparations are the most • Tinea should be suspected if Furthermore, subsequent active prevention is commonly prescribed agents for dermatomy- there is unilateral hand just as important as the initial treatment of the coses, with systemic agents being used for dermatitis and rash on both fungal infection. complex, widespread tinea or when topical agents feet – ‘one hand and two feet’ This article provides a practical approach fail for tinea or yeast infections. The pharmacol- involvement. to antifungal therapy for common fungal infec- ogy of the systemic agents is discussed first here. -
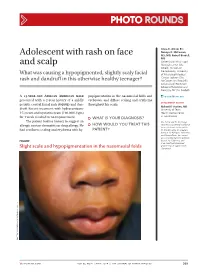
Adolescent with Rash on Face and Scalp
Photo RoUNDS Anna K. Allred, BS; Nancye K. McCowan, Adolescent with rash on face MS, MD; Robert Brodell, MD University of Mississippi and scalp Medical Center (Ms. Allred); Division of Dermatology, University What was causing a hypopigmented, slightly scaly facial of Mississippi Medical Center, Jackson (Drs. rash and dandruff in this otherwise healthy teenager? McCowan and Brodell); University of Rochester School of Medicine and Dentistry, NY (Dr. Brodell) A 13-year-old African American male popigmentation in the nasomesial folds and [email protected] presented with a 2-year history of a mildly eyebrows, and diffuse scaling and erythema DEpartment EDItOR pruritic central facial rash (FIGURE) and dan- throughout his scalp. Richard p. Usatine, MD druff. Recent treatment with hydrocortisone University of Texas 1% cream and nystatin cream (100,000 U/gm) Health Science Center at San Antonio for 1 week resulted in no improvement. ● What is youR diAgnosis? The patient had no history to suggest an Ms. Allred and Dr. McCowan allergic contact dermatitis or drug allergy. He ● HoW Would you TReAT THIS reported no potential conflict of interest relevant to this article. had confluent scaling and erythema with hy- pATIENT? Dr. Brodell serves on speaker’s bureaus for Allergan, Galderma, and PharmaDerm, has served as a consultant and on advisory Figure boards for Galderma, and is an investigator/received grant/research support from Slight scale and hypopigmentation in the nasomesial folds Genentech. PHO T o COU RT ESY OF : R o B e RT BR ODELL , MD jfponline.com Vol 63, no 4 | ApRIL 2014 | The jouRnAl of Family PracTice 209 PHOTO RoUNDS Diagnosis: the Malassezia yeast and topical steroids are Seborrheic dermatitis used to suppress inflammation. -

Tinea Capitis
BCCH Pediatric Dermatology Clinic Joseph M Lam, MD TINEA CAPITIS What is tinea capitis? Treatment Tinea capitis (also called “ringworm of the scalp) is the most Even though the scale is seen on common fungus infection in children, and usually affects the surface of the scalp, the infection goes deep to the root children from 2 to 10 years of age. Fewer than 5 percent of of the hair, under the skin. cases of ringworm of the scalp occur in adults. Most cases of Because of this, just using creams ringworm involving the scalp are due to a fungus that is or shampoos will not clear the passed from person to person, although pets can also pass on infection. the fungus. 1.Terbinafine (pill for scalp The fungal infection can begin fungus) as dandruff, areas of baldness, A pill needs to be taken once a day for about 4 weeks to clear or areas of redness on the scalp the fungus infection. Based on with swelling and pus bumps. your child’s weight, it will be either 1/2, 3/4 or a full pill. Even In some cases, big bumps if the scalp looks better, you (lymph nodes) in the neck may need to take the medicine until Scaly areas of hair loss finished. Unfortunately, there is be felt. no liquid version of terbinafine in The diagnosis of fungus infection is suspected by the Canada. appearance of the scalp and can be verified by fungal 2.Medicated shampoos cultures. The fungal culture usually grows the fungus in four Even though a medicated weeks. -
Ringworm of the Scalp (Tinea Capitis) N
n Ringworm of the Scalp (Tinea Capitis) n Can ringworm of the scalp Ringworm is infection with certain types of fungi called dermatophytes. The name comes from the be prevented? distinct, circle-shaped rash formed when the in- There are some things you can do to help prevent ring- fection involves the skin. When ringworm infects worm of the scalp. However, the infection is difficult to pre- the scalp and hair, it can look several different ways. vent because it is easily passed from person to person—for The scalp can look scaly (like dandruff) and have example, children playing together. (See under “How is bald spots or sores. Treatment with antifungal ringworm of the scalp treated?”) medications is effective. If bald patches are pres- Family members and other people with whom your child ent, the hair will usually grow back once the infec- has been in contact should be checked for infection. Other tion is eliminated. family members, including adults, can carry the infection without having any symptoms. They can be treated with medicated shampoo, as described later. What is ringworm of the scalp? How is ringworm of the Ringworm of the scalp is a common infection caused by scalp diagnosed? certain fungi called dermatophytes. Ringworm of the scalp is also called “tinea capitis.” Dermatophytes also cause infec- The doctor often suspects the diagnosis from the appear- tions of the feet (athlete’s foot) or groin (jock itch). Ring- ance of the rash on the scalp. However, it may be worm of the scalp is most common in young children, confused with other conditions, such as dandruff. -
Tinea Capitis: Current Concepts in Clinical Practice
CONTINUING MEDICAL EDUCATION Tinea Capitis: Current Concepts in Clinical Practice Matthew J. Trovato, MD; Robert A. Schwartz, MD, MPH; Camila K. Janniger, MD GOAL To understand tinea capitis to better treat patients with the condition OBJECTIVES Upon completion of this activity, dermatologists and general practitioners should be able to: 1. Describe the etiology of tinea capitis. 2. Recognize and diagnose tinea capitis. 3. Effectively treat tinea capitis. CME Test on page 88. This article has been peer reviewed and is accredited by the ACCME to provide continuing approved by Victor B. Hatcher, PhD, Professor of medical education for physicians. Medicine, Albert Einstein College of Medicine. Albert Einstein College of Medicine designates Review date: January 2006. this educational activity for a maximum of 1 This activity has been planned and implemented category 1 credit toward the AMA Physician’s in accordance with the Essential Areas and Policies Recognition Award. Each physician should of the Accreditation Council for Continuing Medical claim only that credit that he/she actually spent Education through the joint sponsorship of Albert in the activity. Einstein College of Medicine and Quadrant This activity has been planned and produced in HealthCom, Inc. Albert Einstein College of Medicine accordance with ACCME Essentials. Drs. Trovato, Schwartz, and Janniger report no conflict of interest. The authors discuss off-label use of fluconazole, itraconazole, ketoconazole, and terbinafine. Dr. Hatcher reports no conflict of interest. Tinea capitis is a common infection, particularly seen in Europe and many other countries, which among young children in urban regions. The emit a green fluorescence. However, T tonsurans, infection often is seen in a form with mild scaling like other fungi, also may less often produce an and little hair loss, a result of the prominence of intense inflammatory reaction, which is sugges- Trichophyton tonsurans (the most frequent cause tive of an acute bacterial infection.