Pathophysiology of Compound Heterozygotes Involving Hemoglobinopathies and Thalassemias
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hemoglobin Variants: Biochemical Properties and Clinical Correlates
Downloaded from http://perspectivesinmedicine.cshlp.org/ on September 29, 2021 - Published by Cold Spring Harbor Laboratory Press Hemoglobin Variants: Biochemical Properties and Clinical Correlates Christopher S. Thom1,2, Claire F. Dickson3, David A. Gell3, and Mitchell J. Weiss2 1Cell and Molecular Biology Graduate Group, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania 19104 2Hematology Department, Children’s Hospital of Philadelphia, Philadelphia, Pennsylvania 19104 3Menzies Research Institute, University of Tasmania, Hobart, Australia Correspondence: [email protected] Diseases affecting hemoglobin synthesis and function are extremely common worldwide. More than 1000 naturally occurring human hemoglobin variants with single amino acid substitutions throughout the molecule have been discovered, mainly through their clinical and/or laboratory manifestations. These variants alter hemoglobin structure and biochem- ical properties with physiological effects ranging from insignificant to severe. Studies of these mutations in patients and in the laboratory have produced a wealth of information on he- moglobin biochemistry and biology with significant implications for hematology practice. More generally, landmark studies of hemoglobin performed over the past 60 years have established important paradigms for the disciplines of structural biology, genetics, biochem- istry, and medicine. Here we review the major classes of hemoglobin variants, emphasizing general concepts and illustrative examples. lobin gene mutations affecting hemoglobin stitutions, antitermination mutations, and al- G(Hb), the major blood oxygen (O2) carrier, tered posttranslational processing (Table 1). are common, affecting an estimated 7% of the Naturally occurring Hb mutations cause a world’s population (Weatherall and Clegg 2001; range of biochemical abnormalities, some of Kohne 2011). These mutations are broadly sub- which produce clinically significant symptoms. -

Hemoglobinopathies: Clinical & Hematologic Features And
Hemoglobinopathies: Clinical & Hematologic Features and Molecular Basis Abdullah Kutlar, MD Professor of Medicine Director, Sickle Cell Center Georgia Health Sciences University Types of Normal Human Hemoglobins ADULT FETAL Hb A ( 2 2) 96-98% 15-20% Hb A2 ( 2 2) 2.5-3.5% undetectable Hb F ( 2 2) < 1.0% 80-85% Embryonic Hbs: Hb Gower-1 ( 2 2) Hb Gower-2 ( 2 2) Hb Portland-1( 2 2) Hemoglobinopathies . Qualitative – Hb Variants (missense mutations) Hb S, C, E, others . Quantitative – Thalassemias Decrease or absence of production of one or more globin chains Functional Properties of Hemoglobin Variants . Increased O2 affinity . Decreased O2 affinity . Unstable variants . Methemoglobinemia Clinical Outcomes of Substitutions at Particular Sites on the Hb Molecule . On the surface: Sickle Hb . Near the Heme Pocket: Hemolytic anemia (Heinz bodies) Methemoglobinemia (cyanosis) . Interchain contacts: 1 1 contact: unstable Hbs 1 2 contact: High O2 affinity: erythrocytosis Low O2 affinity: anemia Clinically Significant Hb Variants . Altered physical/chemical properties: Hb S (deoxyhemoglobin S polymerization): sickle syndromes Hb C (crystallization): hemolytic anemia; microcytosis . Unstable Hb Variants: Congenital Heinz body hemolytic anemia (N=141) . Variants with altered Oxygen affinity High affinity variants: erythrocytosis (N=93) Low affinity variants: anemia, cyanosis (N=65) . M-Hemoglobins Methemoglobinemia, cyanosis (N=9) . Variants causing a thalassemic phenotype (N=51) -thalassemia Hb Lepore ( ) fusion Aberrant RNA processing (Hb E, Hb Knossos, Hb Malay) Hyperunstable globins (Hb Geneva, Hb Westdale, etc.) -thalassemia Chain termination mutants (Hb Constant Spring) Hyperunstable variants (Hb Quong Sze) Modified and updated from Bunn & Forget: Hemoglobin: Molecular, Genetic, and Clinical Aspects. WB Saunders, 1986. -

Diagnosis of Sickle Cell Disease and HBB Haplotyping in the Era of Personalized Medicine: Role of Next Generation Sequencing
Journal of Personalized Medicine Article Diagnosis of Sickle Cell Disease and HBB Haplotyping in the Era of Personalized Medicine: Role of Next Generation Sequencing Adekunle Adekile 1,*, Nagihan Akbulut-Jeradi 2, Rasha Al Khaldi 2, Maria Jinky Fernandez 2 and Jalaja Sukumaran 1 1 Department of Pediatrics, Faculty of Medicine, Kuwait University, P.O. Box 24923, Safat 13110, Kuwait; jalajasukumaran@hotmail 2 Advanced Technology Company, Hawali 32060, Kuwait; [email protected] (N.A.-J.); [email protected] (R.A.); [email protected] (M.J.F.) * Correspondence: [email protected]; Tel.: +965-253-194-86 Abstract: Hemoglobin genotype and HBB haplotype are established genetic factors that modify the clinical phenotype in sickle cell disease (SCD). Current methods of establishing these two factors are cumbersome and/or prone to errors. The throughput capability of next generation sequencing (NGS) makes it ideal for simultaneous interrogation of the many genes of interest in SCD. This study was designed to confirm the diagnosis in patients with HbSS and Sβ-thalassemia, identify any ß-thal mutations and simultaneously determine the ßS HBB haplotype. Illumina Ampliseq custom DNA panel was used to genotype the DNA samples. Haplotyping was based on the alleles on five haplotype-specific SNPs. The patients studied included 159 HbSS patients and 68 Sβ-thal patients, previously diagnosed using high performance liquid chromatography (HPLC). There was Citation: Adekile, A.; considerable discordance between HPLC and NGS results, giving a false +ve rate of 20.5% with a S Akbulut-Jeradi, N.; Al Khaldi, R.; sensitivity of 79% for the identification of Sβthal. -
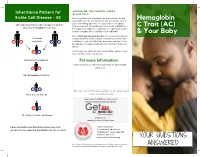
Hemoglobin C Trait (AC) Hemoglobin Eletrophoresis and a Mean Corpuscular Volume
Inheritance Pattern for SHOULD WE, THE PARENTS, TAKE A BLOOD TEST? Sickle Cell Disease - SC Before you have your next baby, we suggest that you and Hemoglobin your partner get special blood test. We all have two sets of genes for hemoglobin. One set is passed on to the baby When one parent has sickle cell trait (AS) and the from each parent. The testing should include, at minimum, a C Trait (AC) other has hemoglobin C trait (AC) hemoglobin eletrophoresis and a mean corpuscular volume. A sickle solubility test (sickledex) is not sufficient! & Your Baby Only if both you and your partner are tested can you know their baby exactly what kind of hemoglobin condition your next child A S may have A C could have. Look carefully at the inheritance pattern for the possibilities of having a baby with the SC form of sickle cell disease. A A A counselor can tell you if any of your future children could have a form of sickle cell disease. AA (normal hemoglobin) For more information or Contact your local SCDAA organization or other health A C agency at: AC (hemoglobin C trait) or A S Or contact the SCDAA National Office at the address and AS (sickle cell trait) or telephone number below. Stay connected with Get Connected the first patient powered registry S C SC (a type of sickle cell disease) Register at www.getconnectedscd.com It does not matter what their other babies have, their Sickle Cell Disease next one has the same four possibilities: AA, AC, AS, or SC. -

Phd Thesis Tjaard Pijning
University of Groningen Divergent or just different Rozeboom, Henriette IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2014 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): Rozeboom, H. (2014). Divergent or just different: Structural studies on six different enzymes. [S.n.]. Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). The publication may also be distributed here under the terms of Article 25fa of the Dutch Copyright Act, indicated by the “Taverne” license. More information can be found on the University of Groningen website: https://www.rug.nl/library/open-access/self-archiving-pure/taverne- amendment. Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. Download date: 29-09-2021 Divergent or just different Structural studies on six different enzymes Henriëtte Rozeboom Printed by Ipskamp Drukkers, Enschede The research presented in this thesis was carried out in the Protein Crystallography group at the Groningen Biomolecular Sciences and Biotechnology Institute. -

Diagnosis of Hemochromatosis in Family Members of Probands: a Comparison of Phenotyping And
Diagnosis of hemochromatosis in family members of probands: A comparison of phenotyping and James C. Barton, MD', Barry E. Rothenberg, PhP, Luigi F. Bertoli, MD1,and Ronald I: Acton, Php Purpose: We wanted to compare phenotyping and HFE genotyping for diagnosis of hemochromatosis in 150 family members of 61 probands. Methods: Phenotypes were defined by persistent transferrin saturation elevation, iron over- load, or both; genotypes were defined by HFE mutation analysis. Results: Twenty-five family members were C282Y homozygotes; 23 of these (92%)had a hemochromatosis phenotype. Twenty-three family members had HFEgenotype C282Y/H63D; eight of these (35%)had a hemochromatosis phenotype. Six of 102 (6%)family members who inher- ited other HFE genotypes had a hemochromatosis phenotype. Conclusion: Phenotyping and genotyping are comple- mentary in diagnosing hemochromatosis among family members of probands. Genetics in Medicine, 1999; 1(3):8%93 Key words: hemochromatosis, iron overload, HFE mutation, genetic counselinF! INTRODUCTION persons who participated were Caucasians and were volunteers, Hemochromatosis is an autosomal recessive disorder that but were not otherwise selected. All probands were adults (218 affects approximately 0.5% of Caucasians of European descent.'s2 years of age); all family members (except an 11-year-old boy) Iron absorption in homozygotes is inappropriately high for body were also adults. We tabulated data on all evaluable family mem- iron content, and many subjects have progressive iron deposi- bers and their corresponding -

Compound Heterozygous C282Y/H63D Mutation in Hemochromatosis: a Case Report
Open Journal of Clinical Diagnostics, 2016, 6, 30-35 http://www.scirp.org/journal/ojcd ISSN Online: 2162-5824 ISSN Print: 2162-5816 Compound Heterozygous C282Y/H63D Mutation in Hemochromatosis: A Case Report Zazour Abdelkrim*, Wafaa Khannoussi, Amine El Mekkaoui, Ghizlane Kharrasse, Zahi Ismaili Hepato-Gastro-Enterology Unit, Mohammed VI University Hospital Oujda, Oujda, Morocco How to cite this paper: Abdelkrim, Z., Abstract Khannoussi, W., El Mekkaoui, A., Kharrasse, G. and Ismaili, Z. (2016) Compound Hete- Hereditary hemochromatosis is a condition characterized by iron overload, which is rozygous C282Y/H63D Mutation in He- both treatable and preventable. It’s mainly related to hepcidin deficiency related to mochromatosis: A Case Report. Open Jour- mutations in genes involved in hepcidin regulation. Iron overload increases the risk nal of Clinical Diagnostics, 6, 30-35. http://dx.doi.org/10.4236/ojcd.2016.63006 of disease such as liver cirrhosis, heart disease and diabetes. Two HFE genotypes have been commonly described in cases of iron overload, C282Y homozygosity and Received: July 25, 2016 C282Y/H63D compound heterozygoty. The diagnosis of this rare disease now can be Accepted: September 18, 2016 explored by biological and imaging tools. We report a case of compound hetero- Published: September 21, 2016 zygous C282Y/H63D discovered by family screening for elevated serum ferritin. Copyright © 2016 by authors and Scientific Research Publishing Inc. Keywords This work is licensed under the Creative Commons Attribution International Iron Overload, Compound Heterozygoty, Phlebotomy License (CC BY 4.0). http://creativecommons.org/licenses/by/4.0/ Open Access 1. Introduction HFE hemochromatosis is a genetic disease related to mutation in HFE gene [1]. -

Genetic Modifiers at the Crossroads of Personalised Medicine for Haemoglobinopathies
Journal of Clinical Medicine Article Genetic Modifiers at the Crossroads of Personalised Medicine for Haemoglobinopathies Coralea Stephanou, Stella Tamana , Anna Minaidou, Panayiota Papasavva, , , Marina Kleanthous * y and Petros Kountouris * y Molecular Genetics Thalassaemia Department, The Cyprus Institute of Neurology and Genetics, Nicosia 2371, Cyprus; [email protected] (C.S.); [email protected] (S.T.); [email protected] (A.M.); [email protected] (P.P.) * Correspondence: [email protected] (M.K.); [email protected] (P.K.); Tel.:+357-2239-2652 (M.K.); +357-2239-2623 (P.K.) Equal contribution; Joint last authorship. y Received: 20 September 2019; Accepted: 5 November 2019; Published: 9 November 2019 Abstract: Haemoglobinopathies are common monogenic disorders with diverse clinical manifestations, partly attributed to the influence of modifier genes. Recent years have seen enormous growth in the amount of genetic data, instigating the need for ranking methods to identify candidate genes with strong modifying effects. Here, we present the first evidence-based gene ranking metric (IthaScore) for haemoglobinopathy-specific phenotypes by utilising curated data in the IthaGenes database. IthaScore successfully reflects current knowledge for well-established disease modifiers, while it can be dynamically updated with emerging evidence. Protein–protein interaction (PPI) network analysis and functional enrichment analysis were employed to identify new potential disease modifiers and to evaluate the biological profiles of selected phenotypes. The most relevant gene ontology (GO) and pathway gene annotations for (a) haemoglobin (Hb) F levels/Hb F response to hydroxyurea included urea cycle, arginine metabolism and vascular endothelial growth factor receptor (VEGFR) signalling, (b) response to iron chelators included xenobiotic metabolism and glucuronidation, and (c) stroke included cytokine signalling and inflammatory reactions. -

Adult, Embryonic and Fetal Hemoglobin Are Expressed in Human Glioblastoma Cells
514 INTERNATIONAL JOURNAL OF ONCOLOGY 44: 514-520, 2014 Adult, embryonic and fetal hemoglobin are expressed in human glioblastoma cells MARWAN EMARA1,2, A. ROBERT TURNER1 and JOAN ALLALUNIS-TURNER1 1Department of Oncology, University of Alberta and Alberta Health Services, Cross Cancer Institute, Edmonton, AB T6G 1Z2, Canada; 2Center for Aging and Associated Diseases, Zewail City of Science and Technology, Cairo, Egypt Received September 7, 2013; Accepted October 7, 2013 DOI: 10.3892/ijo.2013.2186 Abstract. Hemoglobin is a hemoprotein, produced mainly in Introduction erythrocytes circulating in the blood. However, non-erythroid hemoglobins have been previously reported in other cell Globins are hemo-containing proteins, have the ability to types including human and rodent neurons of embryonic bind gaseous ligands [oxygen (O2), nitric oxide (NO) and and adult brain, but not astrocytes and oligodendrocytes. carbon monoxide (CO)] reversibly. They have been described Human glioblastoma multiforme (GBM) is the most aggres- in prokaryotes, fungi, plants and animals with an enormous sive tumor among gliomas. However, despite extensive basic diversity of structure and function (1). To date, hemoglobin, and clinical research studies on GBM cells, little is known myoglobin, neuroglobin (Ngb) and cytoglobin (Cygb) repre- about glial defence mechanisms that allow these cells to sent the vertebrate globin family with distinct function and survive and resist various types of treatment. We have tissue distributions (2). During ontogeny, developing erythro- shown previously that the newest members of vertebrate blasts sequentially express embryonic {[Gower 1 (ζ2ε2), globin family, neuroglobin (Ngb) and cytoglobin (Cygb), are Gower 2 (α2ε2), and Portland 1 (ζ2γ2)] to fetal [Hb F(α2γ2)] expressed in human GBM cells. -

Hemoglobin C Trait What Does This Mean for My Baby, Me and My Family?
My Baby Has Hemoglobin C Trait What does this mean for my baby, me and my family? Your baby's newborn screening test showed tell them their chance to have a baby with a that he or she has hemoglobin C trait (this is hemoglobin disease. also referred to as being a “hemoglobin C carrier”). Babies who have hemoglobin C trait What does having a baby with hemoglobin are no more likely to get sick than any other C trait mean for me, my partner and for baby. They do not need any special medical future pregnancies? treatment. Hemoglobin C trait will not change Since your baby has hemoglobin C trait, this into a disease later on. means that either you or your partner or both of you have hemoglobin C trait. In almost all What causes hemoglobin C trait? cases, ONLY ONE OF YOU will have Hemoglobin C trait happens when the part of hemoglobin C trait. the red blood cell that carries oxygen throughout the body is changed. This part that Most people do not know that they have is changed is called hemoglobin. Hemoglobin hemoglobin C trait. Now that your baby is is important because it picks up oxygen in the known to have hemoglobin C trait, both you lungs and carries it to the other parts of the and your partner have the option of being body. tested. Testing involves a blood test. People usually have one type of hemoglobin. IF ONLY ONE OF YOU HAS HEMOGLOBIN This is called hemoglobin A. Babies with C TRAIT, in every pregnancy there is a: hemoglobin C trait have a second type of • 1 in 2 (50%) chance to have a baby with hemoglobin called hemoglobin C, as well as only the usual hemoglobin A. -

Pathological Conditions Involving Extracellular Hemoglobin
Pathological Conditions Involving Extracellular Hemoglobin: Molecular Mechanisms, Clinical Significance, and Novel Therapeutic Opportunities for alpha(1)-Microglobulin Gram, Magnus; Allhorn, Maria; Bülow, Leif; Hansson, Stefan; Ley, David; Olsson, Martin L; Schmidtchen, Artur; Åkerström, Bo Published in: Antioxidants & Redox Signaling DOI: 10.1089/ars.2011.4282 2012 Link to publication Citation for published version (APA): Gram, M., Allhorn, M., Bülow, L., Hansson, S., Ley, D., Olsson, M. L., Schmidtchen, A., & Åkerström, B. (2012). Pathological Conditions Involving Extracellular Hemoglobin: Molecular Mechanisms, Clinical Significance, and Novel Therapeutic Opportunities for alpha(1)-Microglobulin. Antioxidants & Redox Signaling, 17(5), 813-846. https://doi.org/10.1089/ars.2011.4282 Total number of authors: 8 General rights Unless other specific re-use rights are stated the following general rights apply: Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal Read more about Creative commons licenses: https://creativecommons.org/licenses/ Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. -

Tay Sachs Disease Carrier Screening in the Ashkenazi Jewish Population
Tay Sachs Disease carrier screening in the Ashkenazi Jewish population A needs assessment and review of current services Hilary Burton Sara Levene Corinna Alberg Alison Stewart March 2009 www.phgfoundation.org PHG Foundation Team Dr Hilary Burton Programme Director Ms Corinna Alberg Project Manager Dr Alison Stewart Principal Associate Guy’s & St Thomas’ NHS Foundation Trust Team Ms Sara Levene Registered Genetic Counsellor, Guy’s & St Thomas’ NHS Foundation Trust Dr Christine Patch Consultant Genetic Counsellor and Manager, Guy’s & St Thomas’ NHS Foundation Trust Report authors The Project Team would like to express their thanks to all members of the Advisory Group who gave so freely of Hilary Burton their time and expertise, and particularly to Sue Halliday for chairing the Advisory Group meetings and for her Sara Levene assistance in steering the work. Thanks are also due to Corinna Alberg* Guy’s Hospital for providing us with meeting rooms. Alison Stewart The work was funded through a contract with the UK Newborn Screening Programme Centre and we would like to thank the Programme Centre Director, Dr Barbara Judge, and the Strategic Director, Dr David Elliman, for Published by PHG Foundation Strangeways Research Laboratory Worts Causeway Cambridge CB1 8RN UK First edition, March 2009 © 2009 PHG Foundation ISBN 978-1-907198-00-7 * To whom correspondence should be addressed: [email protected] The PHG Foundation is the working name of the Foundation for Genomics and Population Health, an independent charitable organisation (registered in England and Wales, charity No. 1118664 company No. 5823194), which works with partners to achieve better health through the responsible and evidence-based application of biomedical science.