Your Name O Your Location O Provide the Exact Location of the Patient Within the School
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Parents' Guide to Secondary School Admissions
A parents’ guide to Secondary School Admissions 2019-20 This booklet describes Dudley Council’s arrangements for admitting children to secondary schools in September 2019 If you would like this document on audiotape, in large type, or a translation into your own community language please contact The School Admissions Service. One click… makes it quick www.dudley.gov.uk/admissions A parents’ guide to Secondary School Admissions 2019-20 One click… makes it quick www.dudley.gov.uk/admissions A guide for parents This booklet provides details of the admission arrangements that will operate at secondary schools in the Dudley borough for admissions in September 2019. We have also included general information which you may find useful. If you would like further information about a particular school, a more detailed booklet (‘the School Prospectus’) may be obtained direct from the individual secondary school concerned. Other documents available direct from the school or online include the School Profile and inspection reports by the Office for Standards in Education (Ofsted). The Dudley Secondary School Performance Tables relating to the 2017 examination and test results are currently available from the People Directorate and public libraries. The results for 2018 will not be available until December 2018. Please pay particular attention to the timetable set out on Page 4, especially the closing date for applications, and the specific detail given about each school’s admission arrangements from Page 18 onwards. Local authorities (LAs) are required to liaise with each other in relation to the transfer of children from primary to secondary school for all schools, whether the schools are in Dudley or in other boroughs. -

The Buzz Newsletter Summer 2019
Dudley Academies Trust Summer Newsletter 2the buzz 019 I can hardly believe that another academic year has passed. What a year this has been for the Trust. I feel so proud of our learners and staff and I think this edition of The Buzz really does show the vast range of talent in our academies. I am delighted that learners in all year Please, take a look groups are certainly Dreaming Big and fully at the report, as embracing the opportunities presented to Ofsted have validated them. We have enjoyed so many amazing many of the Trust’s experiences with our young people; to initiatives that are name but a few: the DAT choir performance clearly making a real at University of Wolverhampton, a great difference to our quality team of young people who were trained of education. Well done by the Welsh National Opera, listening to all learners and staff at to Molly’s fantastic ‘Speak Out’ speech Pegasus. at the Speakers’ Trust regional final in Birmingham, and simply hearing about so So, our learners and staff are currently many learners receiving rewards throughout enjoying end of year celebrations by the year for their superb level of effort. participating in an action-packed activities week. I am working closely with Principals To cap it all, an and members of the central team to Ofsted inspection ensure that the Trust continues to improve team visited our academies at pace. We have exciting Pegasus Academy plans for our team of student leaders, we recently to have a ‘commitments’ programme ready undertake a to launch for all learners (a range of extra- full inspection, curricular opportunities and challenges) six months and we are launching our ‘mind to be earlier than we kind’ programme as part of our pledge to anticipated. -

Creating Inspirational Schools
more... Creating Inspirational Schools A Strategic Plan for the Dudley Academies Trust: 2018-2021 [click to enter] Sponsored by BEACON HILL PEGASUS STJAMES THE LINK ACADEMY ACADEMY ACADEMY ACADEMY Dudley College of Technology Sedgley Dudley Dudley Netherton Contents [click tabs for more information] FORWARD The Sponsor About our Our Values Mission and Strategic Strategic Strategic Strategic schools Vision Priority 1 Priority 2 Priority 3 Priority 4 Strategic Strategic Strategic Strategic The Trust’s The Trust’s The Trust’s Find out Outcomes Priority 5 Priority 6 Priority 7 Priority 8 Growth Plan Financial Plan Central Services more Forward Dudley Academies Trust combines Beacon The plans of the Trust are aspirational, not only for the The Trust places a strong emphasis on providing the very best Hill Academy, The Link Academy, Pegasus development of our teaching and learning strategies, but also educational experience for pupils so they can experience both Academy and St James Academy with a strong for the future transformation of the schools’ estates. academic and personal success. and experienced Central Team and the active sponsorship of Dudley College of Technology. The Dudley Academies Trust will bring together the expertise With a focus on English and Mathematics skills as the As a provider graded ‘outstanding’ by Ofsted, of the staff from the four schools with that of the college so foundation for academic success, exciting new ways of teaching Dudley College of Technology will work with the that together their combined management and resources can: these critical subjects will be at the heart of Trustees of Dudley Academies Trust to provide an the Trust’s activity. -

Discover Dudley Academies Trustacademies Always Lookingfor Great Peoplefor Dudley Great Jobs
Dudley Discover Dudley Academies Trust Always looking for great people for great jobs. Recruitment Pack Pack Recruitment 02 Contents Welcome from the Chair of Trustees Our Mission and Vision Dudley College of Technology the Trust’s sponsor About our schools What you have to offer us Who we are looking for Pay and rewards Pay scale Enhanced teacher status Pension Scheme Holiday and Leave Continuous Professional Development and Aspiring Manager Programmes Our Leaders What we have to offer you Living and working in the West Midlands A place to call home Roles we are recruiting to Contact with us Always looking for great Discover Dudley people for great jobs. Academies Trust 03 Recruitment Pack Pack Recruitment Welcome from the Chair of the Board of Trustees We are delighted that you are In this pack you will find a lot of information about interested in working for the joining and working with us. We understand you Dudley Academies Trust are looking for certain things from your working life, including job satisfaction, pay and rewards Dudley Academies Trust is a new Trust formed in commensurate with your skills and abilities and a September 2017 but we have set ourselves an supportive environment in which to work - which ambitious task to transform the life opportunities for presents the potential for personal career progression. the learners in our schools. This is fully articulated in We believe we can offer all of these things and that’s our Strategic Plan 2018-2021, which we would why we have put together this information, to clearly encourage you to read. -

Theatre in Education Tour to Support Personal, Social & Health
Theatre in Education Tour to support Personal, Social & Health Education In Dudley Educational Venues Academic Year 2018-19 Written by Caroline Bridges, Business Growth Manager, Loudmouth Education & Training August 2019 PAGE 1 www.loudmouth.co.uk [email protected] 0121 446 4880 Introduction This evaluation report is feeding back on a theatre in education project that took place during the academic year of 2018-19. The project was to use Theatre in Education (TIE) programmes to support the Personal, Social, Health & Economic Education (PSHE) including Relationship & Sex Education (RSE), safeguarding and alcohol and drug awareness in targeted schools (primary and secondary), colleges, and alternative provision venues in the Dudley area. The tour was delivered by Loudmouth Education & Training using eight of their TIE programmes designed to educate on safeguarding and positive relationships; One 2 Many on alcohol and drug awareness, Helping Hands on staying safe in relationships, Safe & Sound on abuse in teenage relationships, Working For Marcus on Child Exploitation (CE), Trust Me on sexual health, My Mate Fancies You on puberty, and Bully 4 U on anti-bullying (primary and secondary school versions). The primary school version of Bully 4 U was specially updated this year to include work around the 5 Ways to Wellbeing, using new ‘Bully Buster’ superheroes to explain them to the pupils. The tour was funded by the Office of Public Health, Dudley Borough Council and we would like to thank Jill Edwards and Liz Jones for their support. Established in 1994, Loudmouth Education & Training is a theatre company that supports schools and other educational organisations with their PSHE. -

Annex 8 – Academy Trusts Consolidated Into SARA 2018/19 This Annex Lists All Ats Consolidated Into SARA 2018/19, with Their Constituent Academies
Annex 8 – Academy Trusts consolidated into SARA 2018/19 This annex lists all ATs consolidated into SARA 2018/19, with their constituent Academies. * These Academies transferred into the AT from another AT during the year. ** Newly opened or converted to academy status during 2018/19. ^ These Academies transferred out of the AT into another AT during the year. + Closed during the year to 31 August 2019. ++ Closed prior to 31 August 2018. +++ ATs where the Academies had all transferred out over the course of 2018/19. # City Technology colleges (CTC) are included in the SARA consolidation, but do not appear in Annex 1 – Sector Development Data. Further details can be found at www.companieshouse.gov.uk by searching on the company number. -

Dudley Academies Trust: Summer Newsletter 2021
Dudley Academies Trust: Summer Newsletter 2021 Message from the Chief Executive As we near the end of this academic year, we can only reflect on what has been an unprecedented time. The Autumn Term started so well and then we limped towards Christmas as more and more learners and staff fell victim to Covid-19. As cases rose exponentially, it was not surprising that the country was once again locked down. In January, we responded quickly to the ‘new normal’ and moved into full distance learning mode. Our teachers rapidly developed new skills in order to deliver recorded and live lessons. Learners adapted so well to these new requirements and our leaders and support staff set up our secondary schools as testing centres to facilitate the return to face to face learning in March. All of these changes were supported by the Trust’s central team. Our strong sense of community undoubtedly enabled us to navigate these very difficult months and the support of our parents and carers has been greatly appreciated. Once again, there were no examinations in the summer term but, unlike 2020, a new system of teacher assessed grades and centre assessed grades was launched in our secondary schools. With very little notice, teachers and learners had to respond to the Department for Education’s requirements to produce evidence of a range of assessments in every examination subject. This was incredibly challenging and it is clear that formal examinations would have been easier to cope with. Nevertheless, our learners and teachers worked incredibly hard demonstrating real determination to achieve the best that they could. -
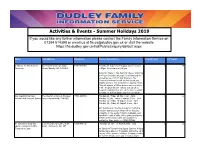
Activities and Events
Activities & Events - Summer Holidays 2019 If you would like any further information please contact the Family Information Service on 01384 814398 or email us at [email protected] or visit the website https://fis.dudley.gov.uk/fsd/PublicEnquiry/default.aspx Name Full Address Telephone Service Description From (Years) To (Years) A Tribute To The Greatest Brierley Hill Civic Hall, Bank 01384 573381 Tuesday 23 July, 6 & 20 August. Doors open at 0 99 Showman Street, Brierley Hill, DY5 3DA 1.45pm. Show starts at 2.30pm Bring the family to this fantastic show celebrating the biggest modern musicals of all time and the biggest movie of 2017. Our tribute to The Greatest Showman has all the hits to get you singing along to this energetic toe tapping show. This will answer a Million dreams so come along to the Greatest Show!! Tickets cost £8 when booked in advanced or £10 on the door. Contact provider for further details and to book tickets. Ace Coaching Summer The Crestwood School, Bromley 07891 297861 Monday 22 - Friday 26 July, 10am - 3pm 4 12 Football And Invasion Games Lane, Kingswinford, DY6 8QG Monday 29 July - Friday 2 August, 10am - 3pm Monday 12 - Friday 16 August, 10am - 3pm Monday 19 - Friday 23 August, 10am - 3pm Ace Coaching are hosting a summer football & invasion games course which will be focusing primarily on the sports football, dodgeball, and handball. Loads of skills, drills, games and goals. Details and booking forms are available by contacting Ryan Lamb on 07891 297861. Air Dynamix Trampoling Leasowes Sports Centre, Kent 07939 445010 Thursday 25 July - 15 August, 9am - 3pm 5 18 Squad - Summer Holiday Road, Halesowen, B62 8PJ Trampoline Camp Air Dynamix Trampolining Squad Summer Holiday Camps takes place on Thursdays during the 1st 4 weeks of the summer holidays. -

Dudley Academies Trust
Dudley Academies Trust Executive offices, Dudley College of Technology Priory Villa, 3 Ednam Road, Dudley, West Midlands, DY1 1HL Chair of Board of Trustees: Lowell Williams Chief Executive: Jo Higgins 16/12/20 Dear Parents/Carers Re: Reporting positive Coronavirus (COVID-19) test results Although our academies are closed over the Christmas period, Public Health England (PHE) has agreed a 6-day window, after the final day of teaching, in which academies are asked to remain contactable so they can assist with contact tracing where necessary. If your child tests positive for coronavirus (COVID-19) between Friday 18th December and Wednesday 23rd December 2020, you should notify the academy by email as soon as possible. The academy will then complete the relevant contact tracing process with Public Health England and notify any other children or staff who have been close contacts and need to self-isolate. In order to notify the school/academy, please send an email to: Blowers Green Primary, [email protected] Beacon Hill Academy, [email protected] Pegasus Academy, [email protected] St James Academy, [email protected] The Link Academy, [email protected] Please be aware that the academy office will not be staffed during the holidays therefore, please do not call the school/academy as the lines will be closed and messages will not be received. Please include the following information in the body of your email: Name of child Child’s class Date of first symptoms Date of test taken Date of positive test outcome Date and time last in school/academy Contact number in case further information is requested by Public Health England Important: The above email addresses are only active between Friday 18th December and Wednesday 23rd December. -

Strategic Plan 2020-2023
Forging Ahead A Strategic Plan for Dudley College of Technology 2020-23 2 For more information log on to www.dudleycol.ac.uk 3 Contents Section 1 Section 7 Foreword 5 Our enabling support services 51 Key achievements 6 7a. Careers, learner services, 52 marketing and public affairs Section 2 7b. Information technology & 53 150 years + of professional and 9 management information services technical education in Dudley Section 8 Section 3 Our human resource strategy 55 Our context 13 3a. A synoptic review of 2016-19 13 Section 9 3b. The fourth industrial revolution, the Industrial 14 Our financial strategy 59 Strategy and the skills needs of our region - the role of colleges in a post Augar, Section 10 post Brexit world Our estates strategy 65 3c. Collaboration, devolution and the 15 West Midlands Combined Authority 3d. Being ‘for’ a place - forging Dudley’s future 15 Section 11 Managing our risks 69 Section 4 Our mission and vision 17 Section 12 Our impact 73 Section 5 Learners at the heart of everything we do 21 5a. Our approach to teaching and learning 21 5b. Supporting our learners and keeping them safe 24 Section 6 Making a strategic impact – 26 our priority sectors 6a. Academic studies 28 6b. Adult programmes for learners returning 30 to studies or preparing for employment 6c. Building technologies and services 32 6d. Digital and creative industries 35 6e. Engineering and advanced manufacturing 38 6f. Health and life science technologies 40 6g. Inclusion programmes 44 6h. Professional services and service Industries 46 6i. Worldwide provision - 48 Dudley College Worldwide For more information log on to www.dudleycol.ac.uk 4 Section 1 Foreword Key achievements For more information log on to www.dudleycol.ac.uk 1 5 Foreword Dudley College of Technology has played a pivotal role in the provision of vocational and technical education in Dudley Borough and the wider Black Country for over 150 years. -

A Parent's Guide to Secondary School Admissions
A parent’s guide to Secondary School Admissions 2020-21 This booklet describes Dudley Council’s arrangements for admitting children to secondary schools in September 2020. If you would like this document on audiotape, in large type, or translation into your own community language, please contact The School Admissions Service. One Click… makes it quick www.dudley.gov.uk/admissions A parents’ guide to Secondary School Admissions 2020-21 One click… makes it quick www.dudley.gov.uk/admissions A guide for parents This booklet provides details of the admission arrangements that will operate at secondary schools in the Dudley borough for admissions in September 2020. We have also included general information which you may find useful. If you would like further information about a particular school, a more detailed booklet (‘the School Prospectus’) may be obtained direct from the individual secondary school concerned. Other documents available direct from the school or online include the School Profile and inspection reports by the Office for Standards in Education (Ofsted). The Dudley Secondary School Performance Tables relating to the 2018 examination and test results are currently available from the Council and in public libraries. The results for 2019 will not be available until December 2019. Please pay particular attention to the timetable set out on Page 6, especially the closing date for applications, and the specific detail given about each school’s admission arrangements that are set out from Page 20 onwards. Local authorities (LAs) are required to liaise with each other in relation to the transfer of children from primary to secondary school for all schools, whether the schools are in Dudley or in other boroughs. -

Dudley Academies Trust Spring Newsletter 2021
Dudley Academies Trust Spring Newsletter 2021 Message from the Chief Executive The spring term has, once again, presented considerable challenges to schools and I am pleased to report that all of our academies have responded superbly. Our central team has provided first class support covering a wide range of provision: the further development of distance learning, training for staff, lesson resources and all aspects of risk assessments and guidance on the adaptations required to set up lateral flow testing centres. Both learners and staff are clearly happy to return to their academies and benefit from the support of our leadership teams to settle back into the rhythm and routines of school life. I should like to thank our parents and carers for being so supportive of our re-opening plans. Our values underpin all that we do. Our Year 6 and Year 11 learners are certainly dreaming big as they are aiming to achieve the best scores and grades in their end of year assessments and examinations. Exciting times lie ahead for them all as they transition into the next phase of their educational journey. 1 - Jo Higgins, Chief Executive Finally, our Trust is all about excellent teaching and learning. Everyone has certainly demonstrated that they respect each other and their world. Our learners’ behaviour has been exemplary when I have visited our academies. Secondary learners wear their masks and have been so sensible during the later flow testing process. At Blowers Green there is always a strong sense of collective responsibility and the pupils clearly care about each other, their teachers and support staff.