Disorders Associated with an Altered Anion Gap
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Ketones, Urine
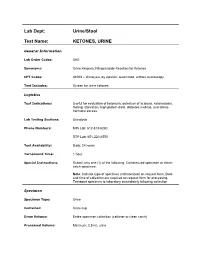
Lab Dept: Urine/Stool Test Name: KETONES, URINE General Information Lab Order Codes: UKE Synonyms: Urine Ketones; Nitroprusside Reaction for Ketones CPT Codes: 81003 – Urinalysis, by dipstick; automated, without microscopy Test Includes: Screen for urine ketones. Logistics Test Indications: Useful for evaluation of ketonuria, detection of acidosis, ketoacidosis, fasting, starvation, high protein diets, diabetes mellitus, and stress- hormone excess. Lab Testing Sections: Urinalysis Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1 hour Special Instructions: Submit only one (1) of the following: Catheterized specimen or clean- catch specimen. Note: Indicate type of specimen (catheterized) on request form. Date and time of collection are required on request form for processing. Transport specimen to laboratory immediately following collection Specimen Specimen Type: Urine Container: Urine cup Draw Volume: Entire specimen collection (catheter or clean catch) Processed Volume: Minimum: 0.5 mL urine Collection: A specimen collected by catheterization is optimal; however, a clean- catch or mid-stream specimen is also acceptable. Random, voided specimens will be accepted, but are the least desirable and are not recommended if a urine culture is also being requested. Special Processing: N/A Patient Preparation: None Sample Rejection: Less than 0.5 mL urine submitted; mislabeled or unlabeled specimen Interpretive Reference Range: Negative Critical Values: N/A Limitations: Specimens containing -

Different Response of Body Weight Change According to Ketonuria After Fasting in the Healthy Obese
ORIGINAL ARTICLE Endocrinology, Nutrition & Metabolism http://dx.doi.org/10.3346/jkms.2012.27.3.250 • J Korean Med Sci 2012; 27: 250-254 Different Response of Body Weight Change According to Ketonuria after Fasting in the Healthy Obese Hyeon-Jeong Kim1, Nam-Seok Joo1, The relationship between obesity and ketonuria is not well-established. We conducted a Kwang-Min Kim1, Duck-Joo Lee1, retrospective observational study to evaluate whether their body weight reduction response and Sang-Man Kim2 differed by the presence of ketonuria after fasting in the healthy obese. We used the data of 42 subjects, who had medical records of initial urinalysis at routine health check-up and 1Department of Family Practice and Community Health, Ajou University School of Medicine, Suwon; follow-up urinalysis in the out-patient clinic, one week later. All subjects in the initial 2Department of Family Medicine, CHA Biomedical urinalysis showed no ketonuria. However, according to the follow-up urinalysis after three Center, CHA University College of Medicine, Seoul, subsequent meals fasts, the patients were divided into a non-ketonuria group and Korea ketonuria group. We compared the data of conventional low-calorie diet programs for ± Received: 20 August 2011 3 months for both groups. Significantly greater reduction of body weight (-8.6 3.6 kg vs 2 2 Accepted: 17 January 2012 -1.1 ± 2.2 kg, P < 0.001), body mass index (-3.16 ± 1.25 kg/m vs -0.43 ± 0.86 kg/m , P < 0.001) and waist circumference (-6.92 ± 1.22 vs -2.32 ± 1.01, P < 0.001) was Address for Correspondence: observed in the ketonuria group compared to the non-ketonuria group. -

Arterial Blood Gases: Acid-Base Balance
EDUCATIONAL COMMENTARY – ARTERIAL BLOOD GASES: ACID-BASE BALANCE Educational commentary is provided through our affiliation with the American Society for Clinical Pathology (ASCP). To obtain FREE CME/CMLE credits click on Earn CE Credits under Continuing Education on the left side of the screen. **Florida licensees, please note: This exercise will appear in CE Broker under the specialty of Blood Gas Analysis. LEARNING OUTCOMES On completion of this exercise, the participant should be able to • identify the important buffering systems in the human body. • explain the Henderson-Hasselbalch equation and its relationship to the bicarbonate/carbonic acid buffer system. • explain the different acid-base disorders, causes associated with them, and compensatory measures. • evaluate acid-base status using patient pH and pCO2 and bicarbonate levels. Introduction Arterial blood gas values are an important tool for assessing oxygenation and ventilation, evaluating acid- base status, and monitoring the effectiveness of therapy. The human body produces a daily net excess of acid through normal metabolic processes: cellular metabolism produces carbonic, sulfuric, and phosphoric acids. Under normal conditions, the body buffers accumulated hydrogen ions (H+) through a variety of buffering systems, the respiratory center, and kidneys to maintain a plasma pH of between 7.35 and 7.45. This tight maintenance of blood pH is essential: even slight changes in pH can alter the functioning of enzymes, the cellular uptake and use of metabolites, and the uptake and release of oxygen. Although diagnoses are made by physicians, laboratory professionals must be able to interpret arterial blood gas values to judge the validity of the laboratory results they report. -

Deficient Diabetic Mice
Diminished Loss of Proteoglycans and Lack of Albuminuria in Protein Kinase C-␣–Deficient Diabetic Mice Jan Menne,1,2 Joon-Keun Park,2 Martin Boehne,2 Marlies Elger,2 Carsten Lindschau,2 Torsten Kirsch,2 Matthias Meier,2 Faikah Gueler,2 Annette Fiebeler,3 Ferdinand H. Bahlmann,2 Michael Leitges,4 and Hermann Haller2 Activation of protein kinase C (PKC) isoforms has been implicated in the pathogenesis of diabetic nephropathy. We showed earlier that PKC-␣ is activated in the kid- iabetes affects Ͼ300 million people worldwide; -neys of hyperglycemic animals. We now used PKC-␣؊/؊ 20–40% will develop overt nephropathy. Diabe mice to test the hypothesis that this PKC isoform tes is the most common cause of end-stage mediates streptozotocin-induced diabetic nephropathy. Drenal disease. The earliest clinical sign of ne- We observed that renal and glomerular hypertrophy was phropathy is microalbuminuria. Microalbuminuria also ؊ ؊ similar in diabetic wild-type and PKC-␣ / mice. How- heralds impending cardiovascular morbidity and mortality ever, the development of albuminuria was almost absent (1–4). Microalbuminuria predicts overt proteinuria, which ؊/؊␣ in the diabetic PKC- mice. The hyperglycemia-in- is now believed to actively promote renal insufficiency (5). duced downregulation of the negatively charged base- Therefore, successful treatment of diabetic patients ment membrane heparan sulfate proteoglycan perlecan -؊ ؊ should aim for the prevention or regression of albumin was completely prevented in the PKC-␣ / mice, com- pared with controls. We then asked whether transform- uria. Hyperglycemia seems to cause microalbuminuria in   diabetic patients (6,7). However, how the metabolic dis- ing growth factor- 1 (TGF- 1) and/or vascular endothelial growth factor (VEGF) is implicated in the turbance causes cellular effects is incompletely under- PKC-␣–mediated changes in the basement membrane. -

Ideal Conditions for Urine Sample Handling, and Potential in Vitro Artifacts Associated with Urine Storage
Urinalysis Made Easy: The Complete Urinalysis with Images from a Fully Automated Analyzer A. Rick Alleman, DVM, PhD, DABVP, DACVP Lighthouse Veterinary Consultants, LLC Gainesville, FL Ideal conditions for urine sample handling, and potential in vitro artifacts associated with urine storage 1) Potential artifacts associated with refrigeration: a) In vitro crystal formation (especially, calcium oxalate dihydrate) that increases with the duration of storage i) When clinically significant crystalluria is suspected, it is best to confirm the finding with a freshly collected urine sample that has not been refrigerated and which is analyzed within 60 minutes of collection b) A cold urine sample may inhibit enzymatic reactions in the dipstick (e.g. glucose), leading to falsely decreased results. c) The specific gravity of cold urine may be falsely increased, because cold urine is denser than room temperature urine. 2) Potential artifacts associated with prolonged storage at room temperature, and their effects: a) Bacterial overgrowth can cause: i) Increased urine turbidity ii) Altered pH (1) Increased pH, if urease-producing bacteria are present (2) Decreased pH, if bacteria use glucose to form acidic metabolites iii) Decreased concentration of chemicals that may be metabolized by bacteria (e.g. glucose, ketones) iv) Increased number of bacteria in urine sediment v) Altered urine culture results b) Increased urine pH, which may occur due to loss of carbon dioxide or bacterial overgrowth, can cause: i) False positive dipstick protein reaction ii) Degeneration of cells and casts iii) Alter the type and amount of crystals present 3) Other potential artifacts: a) Evaporative loss of volatile substances (e.g. -

TITLE: Acid-Base Disorders PRESENTER: Brenda Suh-Lailam
TITLE: Acid-Base Disorders PRESENTER: Brenda Suh-Lailam Slide 1: Hello, my name is Brenda Suh-Lailam. I am an Assistant Director of Clinical Chemistry and Mass Spectrometry at Ann & Robert H. Lurie Children’s Hospital of Chicago, and an Assistant Professor of Pathology at Northwestern Feinberg School of Medicine. Welcome to this Pearl of Laboratory Medicine on “Acid-Base Disorders.” Slide 2: During metabolism, the body produces hydrogen ions which affect metabolic processes if concentration is not regulated. To maintain pH within physiologic limits, there are several buffer systems that help regulate hydrogen ion concentration. For example, bicarbonate, plasma proteins, and hemoglobin buffer systems. The bicarbonate buffer system is the major buffer system in the blood. Slide 3: In the bicarbonate buffer system, bicarbonate, which is the metabolic component, is controlled by the kidneys. Carbon dioxide is the respiratory component and is controlled by the lungs. Changes in the respiratory and metabolic components, as depicted here, can lead to a decrease in pH termed acidosis, or an increase in pH termed alkalosis. Slide 4: Because the bicarbonate buffer system is the major buffer system of blood, estimation of pH using the Henderson-Hasselbalch equation is usually performed, expressed as a ratio of bicarbonate and carbon dioxide. Where pKa is the pH at which the concentration of protonated and unprotonated species are equal, and 0.0307 is the solubility coefficient of carbon dioxide. Four variables are present in this equation; knowing three variables allows for calculation of the fourth. Since pKa is a constant, and pH and carbon dioxide are measured during blood gas analysis, bicarbonate can, therefore, be determined using this equation. -

Approach to Acute Kidney Injury: Differentiation of Prerenal, Postrenal and Intrinsic Renal Disease, Acute Tubular Necrosis and Renal Vascular Disease
Acute Kidney Injury, Renal Vascular Disease Renal Genital Urianry System 2019 APPROACH TO ACUTE KIDNEY INJURY: DIFFERENTIATION OF PRERENAL, POSTRENAL AND INTRINSIC RENAL DISEASE, ACUTE TUBULAR NECROSIS AND RENAL VASCULAR DISEASE Biff F. Palmer, MD, Office: H5.112; Phone 87848 Email: [email protected] LEARNING OBJECTIVES • Given laboratory tests results and radiographic imaging, be able to diagnose a patients with an increased serum creatinine concentration as having post-renal renal disease and list the common clinical etiologies of urinary obstruction • Given laboratory tests results and radiographic imaging, be able to diagnose a patients with an increased serum creatinine concentration as having pre-renal kidney injury • Given pertinent aspects of the history, physical examination, serum and urine electrolytes, and urinalysis in any patient, be able to distinguish pre-renal renal failure from intrinsic renal disease • Given urine and plasma concentrations of sodium and creatinine in any patient, be able to calculate the fractional excretion of sodium (FENa) and interpret the results • List the renal syndromes associated with use of NSAID’s • List the characteristics of thromboembolic disease of the kidney, multiple choesterol emboli syndrome, renal vein thrombosis, and renal artery stenosis After determining chronicity and assessing the level of renal function, one should attempt to classify the patient with renal disease into one of several syndromes based on the renal structures most affected: pre-renal, post-renal or intrinsic renal disease. This classification is based on the information obtained in the history, physical examination, laboratory tests and selected imaging studies. It is particularly important to identify prerenal and postrenal disorders because theses disorders are often readily reversible. -

KETON.Zemia and KETONURIA in CHILDHOOD. by MURIEL J
Arch Dis Child: first published as 10.1136/adc.1.5.302 on 1 January 1926. Downloaded from KETON.zEMIA AND KETONURIA IN CHILDHOOD. BY MURIEL J. BROWN, M.B., Ch.B., D.P.H., AND GRACE GRAHAMI, AM.D. From the Medical Department, The Royal Hospital for Sick Children, Glasgow. The formation of ketone bodies and their excretion in the urine in albnormall amounts have for many years been problems of much interest to both physiologist and clinician. Much of our present knowledge of the subject has been gained from the study of carbohydrate metabolism in diabetes, where ketonuria in its classical formi is frequently observed. From this it has been established that an excess of ketone bodies occurs in the blood when the fats are incompletely ' combusted ' as a result of abnormal carbohydrate metabolism, and ample justification has been provided for the well-known sta.tement myiade by Rosenfeld(l) in 1895 ' that fat burns only in the fire of carbohydrate.' A good review of our present knowledge of ketone production and its prevention is to be found in Shaffer's recent lecture entitled ' Antiketo- genesis, its Mechanism and Signifiecance. '(2) A fu-ll discussion of the stubject in all its aspects is not within the scope of the present communication, but we may quote that ' there no Shaffer's statement is to-day question that http://adc.bmj.com/ ketosis is due to carbohydrate starvation,' and make special reference also to his remninder that the inhibitory effect of carbohydrate on ketone formation depends, not on the mnere existence of sufficient glucose, as glucose, in the blood (cf. -

Acid-Base Physiology & Anesthesia
ACID-BASE PHYSIOLOGY & ANESTHESIA Lyon Lee DVM PhD DACVA Introductions • Abnormal acid-base changes are a result of a disease process. They are not the disease. • Abnormal acid base disorder predicts the outcome of the case but often is not a direct cause of the mortality, but rather is an epiphenomenon. • Disorders of acid base balance result from disorders of primary regulating organs (lungs or kidneys etc), exogenous drugs or fluids that change the ability to maintain normal acid base balance. • An acid is a hydrogen ion or proton donor, and a substance which causes a rise in H+ concentration on being added to water. • A base is a hydrogen ion or proton acceptor, and a substance which causes a rise in OH- concentration when added to water. • Strength of acids or bases refers to their ability to donate and accept H+ ions respectively. • When hydrochloric acid is dissolved in water all or almost all of the H in the acid is released as H+. • When lactic acid is dissolved in water a considerable quantity remains as lactic acid molecules. • Lactic acid is, therefore, said to be a weaker acid than hydrochloric acid, but the lactate ion possess a stronger conjugate base than hydrochlorate. • The stronger the acid, the weaker its conjugate base, that is, the less ability of the base to accept H+, therefore termed, ‘strong acid’ • Carbonic acid ionizes less than lactic acid and so is weaker than lactic acid, therefore termed, ‘weak acid’. • Thus lactic acid might be referred to as weak when considered in relation to hydrochloric acid but strong when compared to carbonic acid. -

Hyperkalemia: This Time, Not the Usual Suspect
TUBULAR QUIZ Port J Nephrol Hypert 2018; 32(4): 395-397 • Advance Access publication 4 January 2019 Hyperkalemia: this time, not the usual suspect Anna Lima, Pedro Campos, Ana Gaspar, Afonso Santos, Patricia Carrilho Department of Nephrology, Hospital Prof Dr Fernando Fonseca, Lisbon, Portugal Received for publication: Dec 18, 2018 Accepted in revised form: Jan 4, 2019 A 49-year-old Caucasian male was admitted to the acidosis, one important step to search for the cause is emergency department with a three-day history of to calculate the anion gap.1 In this case the anion gap abdominal pain and nausea. These episodes were fre- was normal (AG= Na – (CL+HCO3) =12mmol/L). The next quent and, in the previous four months, he had noticed step was to calculate the urinary anion gap (UAG= (Na+ fatigue, more severe in the lower limbs, and symptoms + K+) – Cl-= 74mmol/L), which was highly positive. So, compatible with postural hypotension. He had no fever we were in presence of a metabolic acidosis with non- or any other symptoms. Lab tests requested by his increased anion gap, positive UAG, hyperkalemia and general practitioner six weeks earlier had revealed acidic urine (pH 5) in a patient with normal renal function hyperkalemia, without other relevant changes. He had matching a type IV (distal) renal tubular acidosis.2 followed a low-potassium diet since then. Past medical history included active smoking habits, intravenous There are many causes for hyperkalemic distal renal drug use (he suspended seventeen years ago), and tubular acidosis, the most common of which is diabetes changed bowel habits with alternating obstipation and mellitus (by definition a hyporeninemic hypoaldoster- diarrhea. -

Asymptomatic Bacteriuria and Anti-Microbial Susceptibility Patterns Among Women of Reproductive Age
Article Asymptomatic Bacteriuria and Anti-Microbial Susceptibility Patterns among Women of Reproductive Age. A Cross-Sectional Study in Primary Care, Ghana Prince Afoakwa 1, Seth Agyei Domfeh 1, Bright Oppong Afranie 2,*, Dorcas Ohui Owusu 1, Sampson Donkor 2, Kennedy Kormla Sakyi 3, Richard Akesse Adom 3, Godfred Kyeremeh 1, Bright Afranie Okyere 4, Emmanuel Acheampong 2 and Beatrice Amoah 2 1 Department of Medical Laboratory Technology, Faculty of Health and Allied Sciences, Garden City University College, P.O. Box KS 12775, Kenyasi-Kumasi, Ghana; [email protected] (P.A.); [email protected] (S.A.D.); [email protected] (D.O.O.); [email protected] (G.K.) 2 Department of Molecular Medicine, School of Medical Sciences, Kwame Nkrumah University of Science and Technology, PMB, UPO, Kumasi, Ghana; [email protected] (S.D.); [email protected] (E.A.); [email protected] (B.A.) 3 Department of Microbiology, Tetteh Quarshie memorial hospital, Akuapem Mampong-Korforidua, P.O. Box 26, Ghana; [email protected] (K.K.S.); [email protected] (R.A.A.) 4 Department of Theoretical and Applied Biology, Faculty of Biosciences, Kwame Nkrumah University of Science and Technology, PMB, UPO, Kumasi, Ghana; [email protected] * Correspondence: [email protected]; Tel.: +233-246149286 Received: 2 November 2018; Accepted: 12 December 2018; Published: 17 December 2018 Abstract: Background: Asymptomatic bacteriuria (ASB) poses serious future clinical repercussions for reproductive women. The study determined the prevalence of asymptomatic bacteriuria along with anti-microbial susceptibility patterns among women of reproductive age in a primary care facility. Method: The study recruited a total of 300 women of reproductive age attending the Tetteh Quarshie Memorial Hospital at Akuapem-Mampong, Ghana, between January and March 2018. -

Plasma 'Ketone' Levelin the Diagnosis and Treatment of Diabetic Acidosis
Postgrad. med. J. (October 1968) 44, 799-802. Postgrad Med J: first published as 10.1136/pgmj.44.516.799 on 1 October 1968. Downloaded from Plasma 'ketone' level in the diagnosis and treatment of diabetic acidosis M. S. KNAPP MARGARET E. HORN M.D., M.R.C.P. M.B., M.R.C.P. Lecturer in Medicine, University ofBristol Medical Registrar, Bristol Royal Hospital All patients in possible diabetic acidosis admit- Summary ted to one of the medical firms at the Bristol A simple method of estimating the plasma Royal Infirmary over a 3-year period had an 'ketone' level with 'Acetest' tablets has been used estimation of the plasma 'ketone' level performed in the diagnosis and treatment of diabetic acid- by the clinical staff in the ward side-room. In osis. The method is valuable when used in those patients treated for a moderate or severe association with full biochemical facilities, but it diabetic keto-acidosis the estimation was is especially useful in situations where these can- repeated, usually every four hours. The second not be easily obtained. and subsequent doses of insulin were based to a considerable extent on the plasma 'ketone' titre. Introduction If the titre had not fallen or had risen, an in- In a patient suspected of having diabetic keto- creased dose of insulin was given. A fall in titre acidosis it is useful to be able to rapidly confirm indicated a satisfactory response and either a Protected by copyright. the diagnosis. In this situation we have used a similar dose or a smaller one was used, depending simple side-room method for the detection of on previous blood sugar results.