Genomic Insights Into Mycobacterium Tuberculosis and Its Interaction with the Microbiota
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A DNA Database in the NHS: Your Freedom up for Sale?
A DNA database in the NHS: Your freedom up for sale? May 2013 In April 2013, the Caldicott Committee, including Government Chief Scientist Sir Mark Walport, proposed new rules for data-sharing which would allow the Government to build a DNA database of the whole population of England in the NHS by stealth.1 The plan is to make NHS medical records and people’s genetic information available to commercial companies and to use public-private partnerships to build a system where all private information about every citizen is also accessible to the police, social workers, security services and Government. The Wellcome Trust, which was involved in the Human Genome Project and was led by Walport for ten years, has produced a plan which involves including a variant file, containing the whole genome of every person minus the reference genome, as an attachment to every medical record in the NHS in England.2 This data would be made available to ‘researchers’ (including commercial companies) for data-mining in the cloud and personalised risk assessments would be returned to individuals. The aim is to transform the NHS in line with proposals developed more than a decade ago by former GlaxoSmithKline Chairman Sir Richard Sykes. This is expected to massively expand the market for medicines, medical tests and other products, such as supplements and cholesterol-lowering margarines, by allowing products to be marketed to individuals based on personal risk assessments, created using statistical analysis of genetic data, medical records and other health information. The proposal to build a DNA database in the NHS was endorsed by the Human Genomics Strategy Group in 20123,4 and the Government (led by Prime Minister David Cameron) has quietly adopted this recommendation without telling members of the public. -

Phylogenomic Analysis of the Species of the Mycobacterium Tuberculosis
Phylogenomic analysis of the species of the Mycobacterium tuberculosis complex demonstrates that Mycobacterium africanum, Mycobacterium bovis, Mycobacterium caprae, Mycobacterium microti and Mycobacterium pinnipedii are later heterotypic synonyms of Mycobacterium tuberculosis Marco Riojas, Katya Mcgough, Cristin Rider-Riojas, Nalin Rastogi, Manzour Hernando Hazbón To cite this version: Marco Riojas, Katya Mcgough, Cristin Rider-Riojas, Nalin Rastogi, Manzour Hernando Hazbón. Phy- logenomic analysis of the species of the Mycobacterium tuberculosis complex demonstrates that My- cobacterium africanum, Mycobacterium bovis, Mycobacterium caprae, Mycobacterium microti and Mycobacterium pinnipedii are later heterotypic synonyms of Mycobacterium tuberculosis. Inter- national Journal of Systematic and Evolutionary Microbiology, Microbiology Society, 2018, 68 (1), pp.324-332. 10.1099/ijsem.0.002507. pasteur-01986654 HAL Id: pasteur-01986654 https://hal-riip.archives-ouvertes.fr/pasteur-01986654 Submitted on 18 Jan 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. RESEARCH ARTICLE Riojas et al., Int J Syst Evol Microbiol 2018;68:324–332 DOI 10.1099/ijsem.0.002507 Phylogenomic analysis of the species of the Mycobacterium tuberculosis complex demonstrates that Mycobacterium africanum, Mycobacterium bovis, Mycobacterium caprae, Mycobacterium microti and Mycobacterium pinnipedii are later heterotypic synonyms of Mycobacterium tuberculosis Marco A. -
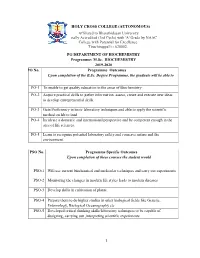
2019-2020 PO No
HOLY CROSS COLLEGE (AUTONOMOUS) Affiliated to Bharathidasan University Nationally Accredited (3rd Cycle) with 'A' Grade by NAAC College with Potential for Excellence. Tiruchirappalli - 620002. PG DEPARTMENT OF BIOCHEMISTRY Programme: M.Sc. BIOCHEMISTRY 2019-2020 PO No. Programme Outcomes Upon completion of the B.Sc. Degree Programme, the graduate will be able to PO-1 To enable to get quality education in the areas of Biochemistry PO-2 Acquire practical skills to gather information, assess, create and execute new ideas to develop entrepreneurial skills. PO-3 Gain Proficiency in basic laboratory techniques and able to apply the scientific method on lab to land PO-4 Inculcate a domestic and international perspective and be competent enough in the area of life sciences. PO-5 Learn to recognize potential laboratory safety and conserve nature and the environment. PSO No. Programme Specific Outcomes Upon completion of these courses the student would PSO-1 Will use current biochemical and molecular techniques and carry out experiments PSO-2 Monitoring the changes in modern life styles leads to modern diseases PSO-3 Develop skills in cultivation of plants. PSO-4 Prepare them to do higher studies in other biological fields like Genetic, Entomology, Biological Oceanography etc PSO-5 Developed critical thinking skills/laboratory techniques to be capable of designing, carrying out ,interpreting scientific experiments 1 HOLY CROSS COLLEGE (AUTONOMOUS) PG DEPARTMENT OF BIOCHEMISTRY (Students admitted from the year 2018 onwards) M.Sc. Biochemistry-Course -

A Simple and Efficient Multiplex PCR Assay for the Identification of Mycobacteriumgenus and Mycobacterium Tuberculosis Complex T
http://dx.doi.org/10.3349/ymj.2013.54.5.1220 Original Article pISSN: 0513-5796, eISSN: 1976-2437 Yonsei Med J 54(5):1220-1226, 2013 A Simple and Efficient Multiplex PCR Assay for the Identification ofMycobacterium Genus and Mycobacterium tuberculosis Complex to the Species Level Yeun Kim,1 Yeonim Choi,1 Bo-Young Jeon,1 Hyunwoo Jin,1,2 Sang-Nae Cho,3 and Hyeyoung Lee1 1Department of Biomedical Laboratory Science, College of Health Sciences, Yonsei University, Wonju; 2Department of Clinical Laboratory Science, College of Health Sciences, Catholic University of Pusan, Busan; 3Department of Microbiology, Yonsei University College of Medicine, Seoul, Korea. Received: September 19, 2012 Purpose: The Mycobacterium tuberculosis complex comprises M. tuberculosis, Revised: October 25, 2012 M. bovis, M. bovis bacillus Calmette-Guérin (BCG) and M. africanum, and causes Accepted: October 29, 2012 tuberculosis in humans and animals. Identification of Mycobacterium spp. and M. Corresponding author: Dr. Hyeyoung Lee, tuberculosis complex to the species level is important for practical use in microbi- Department of Biomedical Laboratory Science, College of Health Sciences, Yonsei University, ological laboratories, in addition to optimal treatment and public health. Materials 1 Yonseidae-gil, Wonju 220-710, Korea. and Methods: A novel multiplex PCR assay targeting a conserved rpoB sequence Tel: 82-33-760-2740, Fax: 82-33-760-2561 in Mycobacteria spp., as well as regions of difference (RD) 1 and RD8, was devel- E-mail: [email protected] oped and evaluated using 37 reference strains and 178 clinical isolates. Results: All mycobacterial strains produced a 518-bp product (rpoB), while other bacteria ∙ The authors have no financial conflicts of produced no product. -

Nontuberculous Mycobacterial Species and Mycobacterium Tuberculosis Complex Coinfection in Patients with Pulmonary Tuberculosis in Dr
[Downloaded free from http://www.ijmyco.org on Saturday, September 28, 2019, IP: 210.57.215.50] Original Research Article Nontuberculous Mycobacterial Species and Mycobacterium Tuberculosis Complex Coinfection in Patients with Pulmonary Tuberculosis in Dr. Soetomo Hospital, Surabaya, Indonesia Ni Made Mertaniasih1,2, Deby Kusumaningrum1,2, Eko Budi Koendhori1,2, Soedarsono3, Tutik Kusmiati3, Desak Nyoman Surya Suameitria Dewi2 Departments of 1Clinical Microbiology and 3Pulmonology, Faculty of Medicine, Airlangga University, Dr. Soetomo Hospital, Surabaya 60131, 2Institute of Tropical Disease, Airlangga University, Surabaya 60115, Indonesia Abstract Objective/Background: The aim of this study was to analyze the detection of nontuberculous mycobacterial (NTM) species derived from sputum specimens of pulmonary tuberculosis (TB) suspects. Increasing prevalence and incidence of pulmonary infection by NTM species have widely been reported in several countries with geographical variation. Materials and Methods: Between January 2014 and September 2015, sputum specimens from chronic pulmonary TB suspect patients were analyzed. Laboratory examination of mycobacteria was conducted in the TB laboratory, Department of Clinical Microbiology, Dr. Soetomo Hospital, Surabaya. Detection and identification of mycobacteria were performed by the standard culture method using the BACTEC MGIT 960 system (BD) and Lowenstein–Jensen medium. Identification of positive Mycobacterium tuberculosis complex (MTBC) was based on positive acid-fast bacilli microscopic smear, positive niacin accumulation, and positive TB Ag MPT 64 test results (SD Bioline). If the growth of positive cultures and acid-fast bacilli microscopic smear was positive, but niacin accumulation and TB Ag MPT 64 (SD Bioline) results were negative, then the isolates were categorized as NTM species. MTBC isolates were also tested for their sensitivity toward first-line anti-TB drugs, using isoniazid, rifampin, ethambutol, and streptomycin. -

Wellcome Trust Annual Report and Financial Statements 2019 Is © the Wellcome Trust and Is Licensed Under Creative Commons Attribution 2.0 UK
Annual Report and Financial Statements 2019 Table of contents Report from Chair 3 Report from Director 5 Trustee’s Report 7 What we do 8 Review of Charitable Activities 9 Review of Investment Activities 21 Financial Review 31 Structure and Governance 36 Social Responsibility 40 Risk Management 42 Remuneration Report 44 Remuneration Committee Report 46 Nomination Committee Report 47 Investment Committee Report 48 Audit and Risk Committee Report 49 Independent Auditor’s Report 52 Financial Statements 61 Consolidated Statement of Financial Activities 62 Consolidated Balance Sheet 63 Statement of Financial Activities of the Trust 64 Balance Sheet of the Trust 65 Consolidated Cash Flow Statement 66 Notes to the Financial Statements 67 Alternative Performance Measures and Key Performance Indicators 114 Glossary of Terms 115 Reference and Administrative Details 116 Table of Contents Wellcome Trust Annual Report 2019 | 2 Report from Chair During my tenure at Wellcome, which ends in The macro environment is increasingly challenging, 2020, I count myself lucky to have had the which has created volatility in financial markets. opportunity to meet inspiring people from a rich Q4 2018 was a very difficult quarter, but the diversity of sectors, backgrounds, specialisms resumption of interest rate cuts by the US Federal and scientific fields. Reserve underpinned another year of gains for our portfolio. We recognise that the cycle is extended, Wellcome’s achievements belong to the people and that the portfolio is likely to face more who work here and to the people we fund – it is challenging times ahead. a partnership that continues to grow stronger, more influential and more ambitious, spurred by The team is working hard to ensure that our independence. -

OVER £140 Prime Minister, the Rt Hon David Came
PRIME MINISTER QUARTERLY INFORMATION: 1 APRIL – 30 JUNE 2011 GIFTS (RECEIVED) OVER £140 Prime Minister, The Rt Hon David Cameron MP Date gift From Gift Value Outcome received April 2011 Prime Minister of Furniture Over Held by Department Pakistan limit April 2011 Prime Minister of Rug Over Held by BHC Pakistan limit Islamabad April 2011 Italian Aeronautica Leather jacket Over Held by Department Militare limit April 2011 Portmeirion Potteries China Over Held by Department Group limit May 2011 President Obama and Silver jewellery and Over Held by Department Mrs Obama First Edition Book limit May 2011 President of Russia Painting Over Held by Department limit May 2011 President of France Pen Set and Over Held by Department Glassware limit June 2011 Prime Minister of Picture Over Held by Department Malaysia limit GIFTS (GIVEN) OVER £140 Prime Minister, The Rt Hon David Cameron MP Date gift From Gift Value Outcome given Nil return HOSPITALITY1 Prime Minister, The Rt Hon David Cameron MP Date Name of Organisation Type of Hospitality Received NIL RETURN 1 Does not normally include attendance at functions hosted by HM Government; ‘diplomatic’ functions in the UK or abroad, hosted by overseas governments; minor refreshments at meetings, receptions, conferences, and seminars; and offers of hospitality which were declined. OVERSEAS TRAVEL Prime Minister Date(s) of trip Destination Purpose of ‘No 32 (The Number of Total cost trip Royal) officials including travel Squadron’ accompanying and or ‘other Minister, where accommodation of RAF’ or non-scheduled -

Nucleic Acid Sequences Specific for Mycobacterium Kansasii
Europaisches Patentamt 19 European Patent Office Office europeen des brevets (n) Publication number : 0 669 402 A2 12 EUROPEAN PATENT APPLICATION @ Application number: 95301106.1 @ Int. CI.6: C12Q 1/68, // (C12Q1/68, C12R1 .32) (§) Date of filing : 21.02.95 (30) Priority : 28.02.94 US 203534 @ Inventor : Spears, Patricia A. 8605 Carol ingian Court @ Date of publication of application : Raleigh, North Carolina 27615 (US) 30.08.95 Bulletin 95/35 Inventor : Shank, Daryl D. 1213 Basil Court @ Designated Contracting States : Bel Air, Maryland 21014 (US) DE FR GB IT NL SE (74) Representative : Ruffles, Graham Keith (7i) Applicant : Becton Dickinson and Company MARKS & CLERK, One Becton Drive 57-60 Lincoln's Inn Fields Franklin Lakes, New Jersey 07417-1880 (US) London WC2A 3LS (GB) (54) Nucleic acid sequences specific for mycobacterium kansasii. (57) Oligonucleotide probes and primers which exhibit M. /ransas/f-specificity in nucleic acid hybridization assays and in nucleic acid amplifi- cation reactions. The full-length M. kan- sasff-specific sequence, identified herein as o o clone MK7, is 493 base pairs in length and has a I GC content of 63%. Several M. kansasii-spec\f\c subsequences of MK7 are also provided. The > probes and primers are useful in assays for > species-specific detection and identification of M. kansasii. oa o > >CD o > CM < CM <~> O O o> CO CO LU Jouve, 18, rue Saint-Denis, 75001 PARIS EP 0 669 402 A2 FIELD OF THE INVENTION The present invention relates to oligonucleotide probes and amplification primers, and particularly relates to oligonucleotide probes and primers which hybridize in a species-specific manner to Mycobacterium kansasii 5 nucleic acids. -

Understanding the an English Agribusiness Lobby Group
Understanding the NFU an English Agribusiness Lobby Group Ethical Consumer Research Association December 2016 Understanding the NFU - an English Agribusiness Lobby-group ECRA December 2016 1 Contents 1. Introduction – The NFU an English Agribusiness Lobby group 3 2. Economic Lobbying – undermining the smaller farmer 2.1 NFU and farm subsidies – promoting agribusiness at the expense of smaller farmers 11 2.2 NFU and TTIP – favouring free trade at the expense of smaller farms 15 2.3 NFU and supermarkets – siding with retailers and opposing the GCA 17 2.4 NFU and foot and mouth disease – exports prioritised over smaller producers 20 3. Environmental Lobbying – unconcerned about sustainability 3.1 NFU, bees and neonicotinoids – risking it all for a few pence more per acre 24 3.2 NFU and soil erosion – opposing formal protection 28 3.3 NFU and air pollution – opposing EU regulation 31 3.4 NFU, biodiversity and meadows – keeping the regulations away 33 3.5 NFU and Europe – keeping sustainability out of the CAP 41 3/6 NFU and climate change – a mixed response 47 3.7 NFU and flooding – not listening to the experts? 51 4. Animal interventions – keeping protection to a minimum 4.1 Farm animal welfare – favouring the megafarm 53 4.2 NFU, badgers and bovine TB – driving a cull in the face of scientific evidence 60 4.3 The Red Tractor label – keeping standards low 74 5. Social Lobbying – passing costs on to the rest of us 5.1 NFU and Organophosphates in sheep dip – failing to protect farmers’ health 78 5.2 NFU and road safety – opposing regulations 82 5.3 NFU and workers’ rights – opposing the Agricultural Wages Board 86 5.4 NFU and Biotechnology – Supporting GM crops 89 6. -

Alagappa University M. Sc. Biotechnology
ANNEXURE I M. Sc., Biotechnology (Specialization: Marine Biotechnology) CBCS Course Structure & Syllabus (For those who joined in July 2011 or after) Department of Biotechnology (UGC-SAP and DST-FIST & PURSE Sponsored Department) Alagappa University (A State University Accredited with “A” Grade by NAAC) Karaikudi 630 003 1 DEPARTMENT OF BIOTECHNOLOGY (UGC-SAP and DST-FIST & PURSE Sponsored Department) ALAGAPPA UNIVERSITY (A State University Accredited with “A” Grade by NAAC) M. Sc., Biotechnology Programme Choice Based Credit System (CBCS) For those who joined in July 2011 or after Course Structure S. Code Name of the Course Credits Marks No SEMESTER – I Int. Ext. Total 1. 501101 Core 1: Biochemistry 4 25 75 100 2. 501102 Core 2: Microbiology 4 25 75 100 3. 501103 Core 3: Molecular Biology and Genetics 4 25 75 100 4. 501104 Core 4: Cell Biology 4 25 75 100 5. 501105 Core 5: Lab I: Analytical Biochemistry 4 25 75 100 6. 501106 Core 6: Lab II: Microbiology 4 25 75 100 7. Elective 1 5 25 75 100 29 175 525 700 SEMESTER – II Int. Ext. Total 8. 501201 Core 7: Immunobiology 4 25 75 100 9. 501202 Core 8: Recombinant DNA Technology 4 25 75 100 10. 501203 Core 9: Plant Molecular Biology 4 25 75 100 11. 501204 Core 10: Lab III: Molecular Genetics 4 25 75 100 12. 501205 Core 11:Lab IV: Immunotechnology 4 25 75 100 13. Elective 2 5 25 75 100 25 150 450 600 SEMESTER – III Int. Ext. Total 14. 501301 Core 12: Bioinformatics 4 25 75 100 15. -

Association of Mycobacterium Africanum Infection with Slower Disease Progression Compared with Mycobacterium Tuberculosis in Malian Patients with Tuberculosis
Am. J. Trop. Med. Hyg., 102(1), 2020, pp. 36–41 doi:10.4269/ajtmh.19-0264 Copyright © 2020 by The American Society of Tropical Medicine and Hygiene Association of Mycobacterium africanum Infection with Slower Disease Progression Compared with Mycobacterium tuberculosis in Malian Patients with Tuberculosis Bocar Baya,1* Bassirou Diarra,1 Seydou Diabate,1 Bourahima Kone,1 Drissa Goita,1 Yeya dit Sadio Sarro,1 Keira Cohen,2 Jane L. Holl,3 Chad J. Achenbach,3 Mohamed Tolofoudie,1 Antieme Combo Georges Togo,1 Moumine Sanogo,1 Amadou Kone,1 Ousmane Kodio,1 Djeneba Dabitao,1 Nadie Coulibaly,1 Sophia Siddiqui,4 Samba Diop,1 William Bishai,2 Sounkalo Dao,1 Seydou Doumbia,1 Robert Leo Murphy,3 Souleymane Diallo,1 and Mamoudou Maiga1,3 1University Clinical Research Center (UCRC)–SEREFO Laboratory-University of Sciences, Techniques and Technologies of Bamako (USTTB), Bamako, Mali; 2Johns Hopkins University School of Medicine, Baltimore, Maryland; 3Northwestern University, Chicago, Illinois; 4National Institutes of Allergic and Infectious Diseases (NIAID), Rockville, Maryland Abstract. Mycobacterium africanum (MAF) is known to endemically cause up to 40–50% of all pulmonary TB in West Africa. The aim of this study was to compare MAF with Mycobacterium tuberculosis (MTB) with regard to time from symptom onset to TB diagnosis, and clinical and radiological characteristics. A cross-sectional study was conducted in Bamako, Mali, between August 2014 and July 2016. Seventy-seven newly diagnosed pulmonary TB patients who were naive to treatment were enrolled at Mali’s University Clinical Research Center. Sputum cultures were performed to confirm the diagnosis and spoligotyping to identify the mycobacterial strain. -

LIST of CONFIRMED SPEAKERS 9Th FEBRUARY
SPEAKERS CONFIRMED AS OF FEBRUARY 9th 2011 - Françoise Barré-Sinoussi , Nobel Prize in Medicine 2008, Professor , Head of Unit of regulation of retroviral infections, Institut Pasteur, Paris, INSERM, France - Zhu Chen , Health Minister, People’s Republic of China - José Angel Cordoba Villalobos , Health Minister, Mexico - Jean-Marie Lehn , Nobel Prize in Chemistry 1987, Professor, University Louis Pasteur, France - Antonio Tajani , Vice president, European Commission, in charge of Industry and Entrepreneurship - Roger Tsien , Nobel Prize in Chemistry 2008, HHMI Investigator, Professor of Pharmacology and of Chemistry & Biochemistry, University of California, San Diego, USA - Ada Yonath , Nobel Prize in Chemistry 2009, Professor, Weizmann Institute, Israel - Bernard Bigot , Chairman and CEO, French Alternative Energies and Atomic Energy Commission (CEA), France - Luis Cantarell , President & CEO Nestlé Health Science S.A., Switzerland - Esther Duflo , Professor, MIT, USA - Catherine Geslain-Lanéelle , Executive Director, European Food Safety Authority - Unni Karunakara , International President, MSF, Switzerland - Vishwa Mohan Katoch , Director, Indian Council of Medical Research - Michel Kazaktchkine , Executive Director, The Global Fund to fight AIDS, Tuberculosis and Malaria - Thomas Lönngren , Executive Director, European Medicines Agency (EMA) - Alain Mérieux , President, Institut Mérieux, France - Feike Sijbesma , CEO & Chairman Managing Board, Royal DSM NV, The Netherlands - Paul Stoffels, M.D., Worldwide Chairman, Janssen, Pharmaceutical