History of UK Biobank, Electronic Medical Records in the NHS, and the Proposal for Data-Sharing Without Consent
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Wellcome Trust Annual Report and Financial Statements 2017 Contents
Annual Report and Financial Statements 2017 2 Wellcome Trust Annual Report and Financial Statements 2017 Contents Report from the Chair and the Director 5 Trustee’s Report 8 What we do 8 Review of Charitable Activities 9 Review of Investment Activities 18 Financial Review 29 Structure and Governance 34 Risk Management 37 Remuneration Report 40 Audit Committee Report 43 Independent Auditor’s Report 45 Financial Statements 58 Consolidated Statement of Financial Activities 58 Consolidated Balance Sheet 59 Statement of Financial Activities of the Trust 60 Balance Sheet of the Trust 61 Consolidated Cash Flow Statement 62 Notes to the Financial Statements 63 Reference and Administrative Details 117 3 Wellcome Trust Annual Report and Financial Statements 2017 “ At Wellcome, we believe in the power of ideas to improve health” Jeremy Farrar Director 4 Wellcome Trust Annual Report and Financial Statements 2017 Report from the Chair and the Director “Our core approach is funding people to explore great ideas, at every step of the way from discovery to impact” At Wellcome, we believe in the power of ideas to improve cause of maternal mortality in the world. It also includes health. Funded from our independent investment portfolio, supporting research in the humanities and social sciences, we support thousands of scientists and researchers in more such as a project which this year published ethical guidelines than 70 countries, as well as innovators, educators and artists. for involving pregnant women in Zika vaccine research. Together, we take on big problems, fuel imaginations and spark And resources like the Human Induced Pluripotent Stem Cell debate, working always to achieve better health for everyone. -
The Electron Microscopy Science Technology Platform at the Francis
The Francis Crick Institute is a The Electron biomedical discovery institute Microscopy dedicated to understanding the fundamental biology underlying Science health and disease. Its work Technology is helping to understand why disease develops and to translate Platform at discoveries into new ways to the Francis prevent, diagnose and treat illnesses such as cancer, heart Crick Institute disease, stroke, infections, and Lucy Collinson neurodegenerative diseases. An independent organisation, its founding partners are the Medical Research Council (MRC), Cancer Research UK, Wellcome, University College London, Imperial College London and King’s College London. The Crick was formed in 2015, with many of the Crick’s scientists joining from two ‘parent’ institutes, the MRC’s National Institute for Medical Research and Cancer Research UK’s London Research Institute, and in 2016 it moved into a brand new state-of- the-art building in central London which brings together 1500 scientists and support staff working collaboratively across disciplines, making it the biggest biomedical research facility under a single roof in Europe. © Nick Guttridge 4 ISSUE 46 JUNE 2017 5 Each microscope room is a six-sided shielded box, • The Phenom-World DelPhi benchtop SEM with walls that contain complex metallic layers has an integrated fluorescence microscope to attenuate DC fields, and an active cancellation for correlative imaging system to attenuate AC fields. Under each • The FEI Twin 120 kV TEM has a cryo stage for microscope is a concrete platform, cast in place, and screening vitrified macromolecular samples supported by air springs that remove environmental prior to imaging on 200 kV and 300 kV TEMs vibration to <1 Hz. -

A DNA Database in the NHS: Your Freedom up for Sale?
A DNA database in the NHS: Your freedom up for sale? May 2013 In April 2013, the Caldicott Committee, including Government Chief Scientist Sir Mark Walport, proposed new rules for data-sharing which would allow the Government to build a DNA database of the whole population of England in the NHS by stealth.1 The plan is to make NHS medical records and people’s genetic information available to commercial companies and to use public-private partnerships to build a system where all private information about every citizen is also accessible to the police, social workers, security services and Government. The Wellcome Trust, which was involved in the Human Genome Project and was led by Walport for ten years, has produced a plan which involves including a variant file, containing the whole genome of every person minus the reference genome, as an attachment to every medical record in the NHS in England.2 This data would be made available to ‘researchers’ (including commercial companies) for data-mining in the cloud and personalised risk assessments would be returned to individuals. The aim is to transform the NHS in line with proposals developed more than a decade ago by former GlaxoSmithKline Chairman Sir Richard Sykes. This is expected to massively expand the market for medicines, medical tests and other products, such as supplements and cholesterol-lowering margarines, by allowing products to be marketed to individuals based on personal risk assessments, created using statistical analysis of genetic data, medical records and other health information. The proposal to build a DNA database in the NHS was endorsed by the Human Genomics Strategy Group in 20123,4 and the Government (led by Prime Minister David Cameron) has quietly adopted this recommendation without telling members of the public. -

The Conservative Party's Credibility Deficit Updated Tax and Spending
The Conservative Party’s credibility deficit Updated tax and spending commitments April 2010 2 Contents Page Introduction 5 Summary 7 Methodology 8 Tables 10 Broken promises 13 45,000 new single rooms in the NHS 15 5,000 new prison places 19 Reducing taxes on savings 22 More places for science courses, training and apprenticeships 24 Maternity nurses for all 25 Reinstate the Defence Export Services Organisation (DESO) 28 National Loan Guarantee Scheme 30 Tax cuts 33 Corporation tax and investment allowance changes 35 Freeze council tax for two years 38 Reduce employers’ NICs for some small companies 41 Tax cuts for married couples 43 Inheritance tax cuts 50 Reverse impact of abolition of dividend tax credit 53 Tax reversals 57 Raise National Insurance Contributions thresholds 59 Oppose Broadband levy 61 Oppose cider duty increase 63 Tax increases 65 Non-domicile levy 67 Spending reductions 73 Cut Government “waste” 75 Savings on employment and skills programmes 78 Reduce spending on Building Schools for the Future 83 Reduce eligibility for tax credits 85 Reduce eligibility for Child Trust Funds 88 Reduce government spending on consultants and advertising 90 Reduce “bureaucracy” spending by a third 92 Welfare savings 95 Scrap ContactPoint 98 NHS IT Programme 100 Freeze pay and cap pensions for public sector workers 103 Reduce spending on Sure Start outreach workers 105 3 Scrap some Regional Development Agencies 107 Scrap regional assemblies 109 Scrap identity cards 110 “Cutting the cost of politics” 112 Scrap the Trade Union Modernisation -

Structure of Human Aspartyl Aminopeptidase Complexed With
Chaikuad et al. BMC Structural Biology 2012, 12:14 http://www.biomedcentral.com/1472-6807/12/14 RESEARCH ARTICLE Open Access Structure of human aspartyl aminopeptidase complexed with substrate analogue: insight into catalytic mechanism, substrate specificity and M18 peptidase family Apirat Chaikuad1, Ewa S Pilka1, Antonio De Riso2, Frank von Delft1, Kathryn L Kavanagh1, Catherine Vénien-Bryan2, Udo Oppermann1,3 and Wyatt W Yue1* Abstract Backround: Aspartyl aminopeptidase (DNPEP), with specificity towards an acidic amino acid at the N-terminus, is the only mammalian member among the poorly understood M18 peptidases. DNPEP has implicated roles in protein and peptide metabolism, as well as the renin-angiotensin system in blood pressure regulation. Despite previous enzyme and substrate characterization, structural details of DNPEP regarding ligand recognition and catalytic mechanism remain to be delineated. Results: The crystal structure of human DNPEP complexed with zinc and a substrate analogue aspartate-β- hydroxamate reveals a dodecameric machinery built by domain-swapped dimers, in agreement with electron microscopy data. A structural comparison with bacterial homologues identifies unifying catalytic features among the poorly understood M18 enzymes. The bound ligands in the active site also reveal the coordination mode of the binuclear zinc centre and a substrate specificity pocket for acidic amino acids. Conclusions: The DNPEP structure provides a molecular framework to understand its catalysis that is mediated by active site loop swapping, a mechanism likely adopted in other M18 and M42 metallopeptidases that form dodecameric complexes as a self-compartmentalization strategy. Small differences in the substrate binding pocket such as shape and positive charges, the latter conferred by a basic lysine residue, further provide the key to distinguishing substrate preference. -

Parliamentary Debates (Hansard)
Wednesday Volume 527 11 May 2011 No. 155 HOUSE OF COMMONS OFFICIAL REPORT PARLIAMENTARY DEBATES (HANSARD) Wednesday 11 May 2011 £5·00 © Parliamentary Copyright House of Commons 2011 This publication may be reproduced under the terms of the Parliamentary Click-Use Licence, available online through The National Archives website at www.nationalarchives.gov.uk/information-management/our-services/parliamentary-licence-information.htm Enquiries to The National Archives, Kew, Richmond, Surrey TW9 4DU; e-mail: [email protected] 1145 11 MAY 2011 1146 12. Andrew Selous (South West Bedfordshire) (Con): House of Commons What progress has been made on the Government’s commitment to undertake a process similar to the Wednesday 11 May 2011 Calman commission on devolution funding; and if she will make a statement. [54363] The House met at half-past Eleven o’clock The Secretary of State for Wales (Mrs Cheryl Gillan): Following the yes vote in the referendum on further PRAYERS powers, we have started to consider the scope and form of such a process. Now that the elections to the National [MR SPEAKER in the Chair] Assembly have taken place I intend to discuss the process with other stakeholders and the First Minister. May I also take this opportunity while I am at the Dispatch Box to offer our congratulations to Carwyn Oral Answers to Questions Jones, who is currently considering forming the Welsh Assembly Government and has the largest party in the Welsh Assembly? WALES Mary Macleod: Our priority in Wales and elsewhere The Secretary of State was asked— right now is to ensure that the deficit is under control. -

'The Left's Views on Israel: from the Establishment of the Jewish State To
‘The Left’s Views on Israel: From the establishment of the Jewish state to the intifada’ Thesis submitted by June Edmunds for PhD examination at the London School of Economics and Political Science 1 UMI Number: U615796 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. Dissertation Publishing UMI U615796 Published by ProQuest LLC 2014. Copyright in the Dissertation held by the Author. Microform Edition © ProQuest LLC. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code. ProQuest LLC 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106-1346 F 7377 POLITI 58^S8i ABSTRACT The British left has confronted a dilemma in forming its attitude towards Israel in the postwar period. The establishment of the Jewish state seemed to force people on the left to choose between competing nationalisms - Israeli, Arab and later, Palestinian. Over time, a number of key developments sharpened the dilemma. My central focus is the evolution of thinking about Israel and the Middle East in the British Labour Party. I examine four critical periods: the creation of Israel in 1948; the Suez war in 1956; the Arab-Israeli war of 1967 and the 1980s, covering mainly the Israeli invasion of Lebanon but also the intifada. In each case, entrenched attitudes were called into question and longer-term shifts were triggered in the aftermath. -

The Development of Large-Scale De-Identified Biomedical Databases in the Age of Genomics—Principles and Challenges Fida K
Dankar et al. Human Genomics (2018) 12:19 https://doi.org/10.1186/s40246-018-0147-5 REVIEW Open Access The development of large-scale de-identified biomedical databases in the age of genomics—principles and challenges Fida K. Dankar1* , Andrey Ptitsyn2 and Samar K. Dankar3 Abstract Contemporary biomedical databases include a wide range of information types from various observational and instrumental sources. Among the most important features that unite biomedical databases across the field are high volume of information and high potential to cause damage through data corruption, loss of performance, and loss of patient privacy. Thus, issues of data governance and privacy protection are essential for the construction of data depositories for biomedical research and healthcare. In this paper, we discuss various challenges of data governance in the context of population genome projects. The various challenges along with best practices and current research efforts are discussed through the steps of data collection, storage, sharing, analysis, and knowledge dissemination. Keywords: Biomedical database, Data privacy, Data governance, Whole genome sequencing Background first, now increasingly shifting to whole exome and whole Overview genome sequencing [2, 3]). The project started by Decode Databases are both the result and the instrument of has generated one of the best resources for discovery in research. From the earliest times, assembling collections biomedical sciences and inspired development of multiple of samples and stories was essential for any research pro- populational and national genomics projects, also feeding ject. The results of research feeding back into the libraries into integrated databases. Genomics England [4], Human and collections create a positive feedback in the accumula- Longevity [5], All of US (formerly known as Precision tion of knowledge limited only by the technological plat- Medicine Initiative) [6], China’s Precision Medicine Initia- form for storage and retrieval of information. -

'Iceland Inc.'?: on the Ethics of Commercial Population Genomics
University of Pennsylvania ScholarlyCommons Center for Bioethics Papers Center for Bioethics March 2004 'Iceland Inc.'?: On the ethics of commercial population genomics Jon F. Merz University of Pennsylvania, [email protected] Glenn E. McGee University of Pennsylvania Pamela Sankar University of Pennsylvania Follow this and additional works at: https://repository.upenn.edu/bioethics_papers Recommended Citation Merz, J. F., McGee, G. E., & Sankar, P. (2004). 'Iceland Inc.'?: On the ethics of commercial population genomics. Retrieved from https://repository.upenn.edu/bioethics_papers/52 Postprint version. Published in Social Science and Medicine, Volume 58, Issue 6, March 2004, pages 1201-1209. Publisher URL: http://dx.doi.org/10.1016/S0277-9536(03)00256-9 This paper is posted at ScholarlyCommons. https://repository.upenn.edu/bioethics_papers/52 For more information, please contact [email protected]. 'Iceland Inc.'?: On the ethics of commercial population genomics Abstract A detailed analysis of the Icelandic commercial population-wide genomics database project of deCODE Genetics was performed for the purpose of providing ethics insights into public/private efforts to develop genetic databases. This analysis examines the moral differences between the general case of governmental collection of medical data for public health purposes and the centralized collection planned in Iceland. Both the process of developing the database and its design vary in significant ways from typical government data collection and analysis activities. Because of these differences, the database may serve the interests of deCODE more than it serves the interests of the public, undermining the claim that presumed consent for this data collection and its proprietary use is ethical. -
2019-2020 PO No
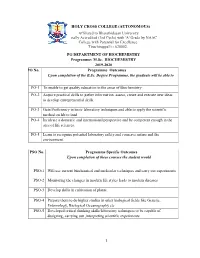
HOLY CROSS COLLEGE (AUTONOMOUS) Affiliated to Bharathidasan University Nationally Accredited (3rd Cycle) with 'A' Grade by NAAC College with Potential for Excellence. Tiruchirappalli - 620002. PG DEPARTMENT OF BIOCHEMISTRY Programme: M.Sc. BIOCHEMISTRY 2019-2020 PO No. Programme Outcomes Upon completion of the B.Sc. Degree Programme, the graduate will be able to PO-1 To enable to get quality education in the areas of Biochemistry PO-2 Acquire practical skills to gather information, assess, create and execute new ideas to develop entrepreneurial skills. PO-3 Gain Proficiency in basic laboratory techniques and able to apply the scientific method on lab to land PO-4 Inculcate a domestic and international perspective and be competent enough in the area of life sciences. PO-5 Learn to recognize potential laboratory safety and conserve nature and the environment. PSO No. Programme Specific Outcomes Upon completion of these courses the student would PSO-1 Will use current biochemical and molecular techniques and carry out experiments PSO-2 Monitoring the changes in modern life styles leads to modern diseases PSO-3 Develop skills in cultivation of plants. PSO-4 Prepare them to do higher studies in other biological fields like Genetic, Entomology, Biological Oceanography etc PSO-5 Developed critical thinking skills/laboratory techniques to be capable of designing, carrying out ,interpreting scientific experiments 1 HOLY CROSS COLLEGE (AUTONOMOUS) PG DEPARTMENT OF BIOCHEMISTRY (Students admitted from the year 2018 onwards) M.Sc. Biochemistry-Course -

Biobanks for Europe
KI-NA-25-302-EN-C This expert group report on the ethical and regulatory challenges of international biobank research has been authored by an interdisciplinary group with experts from science, law, governance and ethics. Biobanks for Biobank research is rapidly evolving, and in close interaction with developments in informatics and genomics. The size and breath of the collections of biological samples and associated data that can be Europe assembled has increased exponentially. This opens up a vast range of new options for research and diagnosis, but at the same time also holds an important challenge for the governance of these activities. In this report, the expert group makes speci c recommendations for good A Challenge for Governance governance of Biobanks Research and Innovation policy Research and Innovation ed205134cover_BAT.indd 1-3 11/06/12 09:14 How to obtain EU publications Free publications: • via EU Bookshop (http://bookshop.europa.eu); • at the European Union’s representations or delegations. You can obtain their contact details on the Internet (http://ec.europa.eu) or by sending a fax to +352 2929-42758. Priced publications: • via EU Bookshop (http://bookshop.europa.eu). Priced subscriptions (e.g. annual series of the O cial Journal of the European Union and reports of cases before the Court of Justice of the European Union): • via one of the sales agents of the Publications O ce of the European Union (http://publications.europa.eu/others/agents/index_en.htm). EUROPEAN COMMISSION Directorate-General for Research and Innovation Directorate B — European Research Area Unit B6 — Ethics and gender Contact: Lino PAULA European Commission B-1049 Brussels E-mail: [email protected] ed205134cover_BAT.indd 4-6 11/06/12 09:14 EUROPEAN COMMISSION Biobanks for Europe A challenge for governance Report of the Expert Group on Dealing with Ethical and Regulatory Challenges of International Biobank Research Chair: Herbert Gottweis Rapporteur: Jane Kaye Members: Fabrizia Bignami, Emmanuelle Rial-Sebbag, Roberto Lattanzi, Milan Macek Jr. -

Honorary Degrees 2011
Honorary Degrees 2011 The full list of those who received honorary degrees is as follows: COMMEMORATION DAY, WEDNESDAY 15 JUNE 2011 DEGREE OF DOCTOR OF DIVINITY (DD) Very Reverend David LUNAN, Clerk to the Presbytery of Glasgow DEGREE OF DOCTOR OF LAWS (LLD) Baroness Brenda HALE, Barrister and Judge DEGREE OF DOCTOR OF LETTERS (DLitt) Professor Toshiyuki TAKAMIYA, Emeritus Professor, Keio University, Tokyo DEGREE OF DOCTOR OF SCIENCE (DSc) Professor Sir Leszek BORYSIEWICZ, Vice-Chancellor of the University of Cambridge & former Chief Executive of the MRC Professor Victor J DZAU, James B Duke Professor of Medicine, Duke University, USA DEGREE OF DOCTOR OF THE UNIVERSITY (DUniv) Lord John MCFALL of Alcuith, Former MP for West Dunbartonshire SUMMER GRADUATIONS DEGREE OF DOCTOR OF LETTERS (DLitt) 5 March FAN ZENG, Prominent Artist in traditional Chinese Art DEGREE OF DOCTOR OF LETTERS (DLitt) GSA Graduation 17 June Katrina BROWN, Director of the Glasgow International Festival of Visual Arts DEGREE OF DOCTOR OF LETTERS (DLitt) 23 June 11am Professor Simon BLACKBURN, Faculty of Philosophy, University of Cambridge DEGREE OF DOCTOR OF LETTERS (DLitt) 28 June 11am Professor Sir Hilary BECKLES, University of West Indies, West Indies Professor Caroline Walker BYNUM, Emeritus Professor, Columbia University, USA DEGREE OF DOCTOR OF LETTERS (DLitt) 28 June 4pm Armando IANNUCCI, Comedy Writer, Producer and Director DEGREE OF DOCTOR OF LETTERS (DLitt) 6 July Crichton Campus Alastair REID, Writer and Translator DEGREE OF DOCTOR OF SCIENCE (DSc) 10 February