Understanding Common Eye Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vision Rehabi I Itation for Patients with Age Related Macular Degeneration
Vision rehabi I itation for GARY S. RUBIN patients with age related macular degeneration Epidemiology of low vision The over-representation of macular degeneration patients in the low-vision clinic is The epidemiology of vision impairment is dealt reflected in the chief complaints of those with in detail elsewhere.1 However, there is one referred for rehabilitation. A study of 1000 particularly salient factor that bears emphasis. consecutive patients seen at the Wilmer Low The prevalence of vision impairment increases Vision clinic indicated that 64% listed 'reading' dramatically with advancing age. Statistics as their chief complaint, while other activities compiled in the UK by the Royal National were identified by fewer than 8% of patients. Institute for the Blind2 indicate that there were Undoubtedly the bias towards reading approximately 1.1 million blind or partially problems results partly from the nature of the sighted persons in 1996, of whom 82% were 65 low-vision services offered. Those served by a years of age or older. Thus it is not surprising to community-based programme that includes learn that the major causes of vision impairment home visits might be more likely to report are age-related eye diseases. Fig. 1 illustrates the problems with activities of daily living, while a distribution of causes of vision impairment blind rehabilitation centre would be more likely 5 from three recent studies?- Approximately to address mobility issues. Nevertheless, most equal percentages are attributed to macular macular degeneration patients are referred to degeneration and cataract, with smaller hospital or optometry clinic services, and as percentages for glaucoma, diabetic retinopathy their overwhelming concern is with reading, and optic neuropathies. -

Symptoms of Age Related Macular Degeneration
WHAT IS MACULAR DEGENERATION? wavy or crooked, visual distortions, doorway and the choroid are interrupted causing waste or street signs seem bowed, or objects may deposits to form. Lacking proper nutrients, the light- Age related macular degeneration (AMD) is appear smaller or farther away than they sensitive cells of the macula become damaged. a disease that may either suddenly or gradually should, decrease in or loss of central vision, and The damaged cells can no longer send normal destroy the macula’s ability to maintain sharp, a central blurry spot. signals from the macula through the optic nerve to central vision. Interestingly, one’s peripheral or DRY: Progression with dry AMD is typically slower your brain, and consequently your vision becomes side vision remains unaffected. AMD is the leading de-gradation of central vision: need for increasingly blurred cause of “legal blindness” in the United States for bright illumination for reading or near work, diffi culty In either form of AMD, your vision may remain fi ne persons over 65 years of age. AMD is present in adapting to low levels of illumination, worsening blur in one eye up to several years even while the other approximately 10 percent of the population over of printed words, decreased intensity or brightness of eye’s vision has degraded. Most patients don’t the age of 52 and in up to 33 percent of individuals colors, diffi culty recognizing faces, gradual increase realize that one eye’s vision has been severely older than 75. The macula allows alone gives us the in the haziness of overall vision, and a profound drop reduced because your brain compensates the bad ability to have: sharp vision, clear vision, color vision, in your central vision acuity. -

Vision Screening Training
Vision Screening Training Child Health and Disability Prevention (CHDP) Program State of California CMS/CHDP Department of Health Care Services Revised 7/8/2013 Acknowledgements Vision Screening Training Workgroup – comprising Health Educators, Public Health Nurses, and CHDP Medical Consultants Dr. Selim Koseoglu, Pediatric Ophthalmologist Local CHDP Staff 2 Objectives By the end of the training, participants will be able to: Understand the basic anatomy of the eye and the pathway of vision Understand the importance of vision screening Recognize common vision disorders in children Identify the steps of vision screening Describe and implement the CHDP guidelines for referral and follow-up Properly document on the PM 160 vision screening results, referrals and follow-up 3 IMPORTANCE OF VISION SCREENING 4 Why Screen for Vision? Early diagnosis of: ◦ Refractive Errors (Nearsightedness, Farsightedness) ◦ Amblyopia (“lazy eye”) ◦ Strabismus (“crossed eyes”) Early intervention is the key to successful treatment 5 Why Screen for Vision? Vision problems often go undetected because: Young children may not realize they cannot see properly Many eye problems do not cause pain, therefore a child may not complain of discomfort Many eye problems may not be obvious, especially among young children The screening procedure may have been improperly performed 6 Screening vs. Diagnosis Screening Diagnosis 1. Identifies children at 1. Identifies the child’s risk for certain eye eye condition conditions or in need 2. Allows the eye of a professional -

Macular Degeneration
DRIVEWELL Driving When You Have Macular Degeneration You have been a safe driver for years. For you, driving means freedom and control. As you get older, changes in your physical and mental health can affect how safely you drive. Macular degeneration (also known as age-related macular degeneration) damages the macula, a spot near the center of the retina (light-sensitive inner lining of the eyeball). It is a common eye problem among older drivers that makes it hard to drive safely. Age-related macular degeneration is the leading cause of new cases of blindness in people 65 and older. If you have macular degeneration, you may not notice any signs in the early stages. You may not know you have this condition until you lose your peripheral vision (what you see out of the corner of your eyes). In time it will affect your central vision, causing a dark or empty area in the center of your vision. How Can Macular Degeneration Affect the Way I Drive? • Your central vision may be dull and blurry. This can lead to loss of sharp vision. • You may not see the road, street signs, lane markers, and even people and bicyclists in the road. • You may need more bright light to see up close. • Colors may look less vivid or bright. • You may have trouble when you go from bright light to low light. • You may not be able to recognize people’s faces. What Should I Do if I Have Any of These Signs? As soon as you notice any of these warning signs: • Tell your family or someone close to you, especially if you have a family history of macular degeneration or have changes in your central vision. -

Detached and Torn Retina Retinal Detachments Occur in 1 out of 10,000 Americans Each Year
Detached and Torn Retina Retinal Detachments Occur in 1 Out of 10,000 Americans Each Year A retinal detachment is not as common as other eye conditions such as glaucoma or macular degeneration, however… it is just as serious and it is a vision threatening condition which should be treated as an emergency. Dr. Randy Katz, Florida Eye’s Diabetic Retinopathy, Retinal Detachment & Macular Degeneration Specialist says that the sooner a retinal tear or detachment is treated the better the chances of saving the vision in the eye. What Is a Retinal Detachment? The retina is the light-sensitive layer of tissue that lines the inside of the eye and sends visual messages through the optic nerve to the brain. When the retina detaches, it is lifted or pulled from its normal position. When this occurs, if not promptly treated, retinal detachment can cause permanent vision loss. In some cases there may be small areas of the retina that are torn. These areas, called retinal tears or retinal breaks, can lead to a retinal detachment. Vitreous gel, the clear material that fills the eyeball, is attached to the retina in the back of the eye. As we get older, the vitreous may change shape, pulling away from the retina. If the vitreous pulls a piece of the retina with it, it causes a retinal tear. Once a retinal tear occurs, vitreous fluid may seep through and lift the retina off the back wall of the eye, causing the retina to detach or pull away. 2 Are You At Risk for a Torn or Detached Retina? A retinal detachment can occur at any age, but it is more common in people over age 40. -

Jaeger Eye Chart
Jaeger Eye Chart DIRECTIONS FOR USE The Jaeger eye chart (or Jaeger card) is used to test and document near visual acuity at a normal reading distance. Refractive errors and conditions that cause blurry reading vision include astigmatism, hyperopia (farsightedness) and presbyopia (loss of near focusing ability after age 40). If you typically wear eyeglasses or contact lenses full-time, you should wear them during the test. 1. Hold the test card 14 inches from the eyes. Use a tape measure to verify this distance. 2. The card should be illuminated with lighting typical of that used for comfortable reading. 3. Testing usually is performed with both eyes open; but if a significant difference between the two eyes is suspected, cover one eye and test each eye separately. 4. Go to the smallest block of text you feel you can see without squinting, and read that passage aloud. 5. Then try reading the next smaller block of text. (Remember: no squinting!) 6. Continue reading successively smaller blocks of print until you reach a size that is not legible. 7. Record the “J” value of the smallest block of text you can read (example: “J1”). DISCLAIMER: Eye charts measure only visual acuity, which is just one component of good vision. They cannot determine if your eyes are “working overtime” (needing to focus more than normal, which can lead to headaches and eye strain). Nor can they determine if your eyes work properly as a team for clear, comfortable binocular vision and accurate depth perception. Eye charts also cannot detect serious eye problems such as glaucoma or early diabetic retinopathy that could lead to serious vision impairment and even blindness. -

AAO 2018 2019 BCSC Sectio
The American Academy of Ophthalmology is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. The American Academy of Ophthalmology designates this enduring material for a maximum of 15 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. CME expiration date: June 1, 2021. AMA PRA Category 1 Credits™ may be claimed only once between June 1, 2018, and the expiration date. BCSC® volumes are designed to increase the physician’s ophthalmic knowledge through study and review. Users of this activity are encouraged to read the text and then answer the study questions provided at the back of the book. To claim AMA PRA Category 1 Credits™ upon completion of this activity, learners must demonstrate appropriate knowledge and participation in the activity by taking the posttest for Section 3 and achieving a score of 80% or higher. For further details, please see the instructions for requesting CME credit at the back of the book. The Academy provides this material for educational purposes only. It is not intended to represent the only or best method or procedure in every case, nor to replace a physician’s own judgment or give specic advice for case management. Including all indications, contraindications, side eects, and alternative agents for each drug or treatment is beyond the scope of this material. All information and recommendations should be veried, prior to use, with current information included in the manufacturers’ package inserts or other independent sources, and considered in light of the patient’s condition and history. -
PROTOCOL STUDY TITLE: Evaluation of Reading Speed
PROTOCOL STUDY TITLE: Evaluation of ReAding Speed, Contrast Sensitivity, and Work Productivity in Working Individuals with Diabetic Macular Edema Following Treatment with Intravitreal Ranibizumab (ERASER Study) STUDY DRUG Recombinant humanized anti-VEGF monoclonal antibody fragment (rhuFab V2 [ranibizumab]) California Retina Research Foundation SPONSOR 525 E. Micheltorena Street, Suites A & D Santa Barbara, California, United States 93103 NCT NUMBER: NCT02107131 INVESTIGATOR Nathan Steinle, MD SUB- Robert Avery, MD INVESTIGATORS Ma’an Nasir, MD Dante Pieramici, MD Alessandro Castellarin, MD Robert See, MD Stephen Couvillion, MD Dilsher Dhoot, MD DATE: 12/4/2015 AMENDMENT: 3 Protocol: ML29184s Amendment Date: 4December2015 Lucentis IST Program 1. BACKGROUND 1.1 PATHOPHYSIOLOGY Diabetic retinopathy is the leading cause of blindness associated with retinal vascular disease. Macular edema is a major cause of central vision loss in patients presenting with diabetic retinopathy. The prevalence of diabetic macular edema after 15 years of known diabetes is approximately 20% in patients with type 1 diabetes mellitus (DM), 25% in patients with type 2 DM who are taking insulin, and 14% in patients with type 2 DM who do not take insulin. Breakdown of endothelial tight junctions and loss of the blood-retinal barrier between the retinal pigment epithelium and choriocapillaris junction lead to exudation of blood, fluid, and lipid leading to thickening of the retina. When these changes involves or threatens the fovea, there is a higher risk of central vision loss. Functional and eventual structural changes in the blood-retinal barrier as well as reduced retinal blood flow leads to the development of hypoxia. These changes may result in upregulation and release of vascular endothelial growth factor (VEGF), a 45 kD glycoprotein. -

Screening for Visual Impairment in Children Ages 1–5 Years: Update for the USPSTF
Screening for Visual Impairment in Children Ages 1–5 Years: Update for the USPSTF AUTHORS: Roger Chou, MD,a,b,c Tracy Dana, MLS,a and abstract Christina Bougatsos, BSa CONTEXT: Screening could identify preschool-aged children with vi- aOregon Evidence-Based Practice Center and Departments of bMedicine and cMedical Informatics and Clinical Epidemiology, sion problems at a critical period of visual development and lead to Oregon Health & Science University, Portland, Oregon treatments that could improve vision. KEY WORDS OBJECTIVE: To determine the effectiveness of screening preschool- impaired visual acuity, vision screening, vision tests, preschool aged children for impaired visual acuity on health outcomes. children, refractive errors, amblyopia, amblyogenic risk factors, random dot E stereoacuity test, MTI photoscreener, patching, METHODS: We searched Medline from 1950 to July 2009 and the Co- systematic review chrane Library through the third quarter of 2009, reviewed reference ABBREVIATIONS lists, and consulted experts. We selected randomized trials and con- USPSTF—US Preventive Services Task Force trolled observational studies on preschool vision screening and treat- logMAR—logarithmic minimal angle of resolution ALSPAC—Avon Longitudinal Study of Parents and Children ments, and studies of diagnostic accuracy of screening tests. One in- RR—relative risk vestigator abstracted relevant data, and a second investigator CI—confidence interval checked data abstraction and quality assessments. VIP—Vision in Preschoolers PLR—positive likelihood ratio RESULTS: Direct evidence on the effectiveness of preschool vision NLR—negative likelihood ratio screening for improving visual acuity or other clinical outcomes re- MTI—Medical Technology and Innovations OR—odds ratio mains limited and does not adequately address whether screening is D—diopter(s) more effective than no screening. -
Refractive Error Is a Disease of the Eye, and We Should Treat It
Refractive error is a disease of the eye, and we should treat it. believe that refractive error is a disease of the eye— no different from glaucoma, dry eye disease, and other issues for which we readily offer treatment. In the world of modern cataract and refractive surgery, we have the capability to correct visual Iacuity that is compromised due to astigmatism and other types refractive error, so why shouldn't we treat astigmatism during cataract surgery? A large percentage of our cataract patients, about 75%, have at least 0.50 D of astigmatism. Even this small amount of astigmatism can and often does create issues visually for patients. The higher the My Philosophy of level of astigmatism, the more it can affect vision. My philosophy is, why not try to help these people? Correcting their astigmatism will help them to achieve better visual acuity, and this is even more crucial in patients who elect a multifocal, extended depth of focus, or other premium IOL. It is important to educate patients about their astigmatism and to relay to them what we can do ASTIGMATISM to correct it. The level of care and attention to detail affects everything, from our surgical outcomes, to the practice’s reputation, to future referral patterns. THRESHOLDS AND BEST PRACTICES My threshold for astigmatism treatment is about 0.75 D. Above that, the patient can lose contrast and can have functional visual acuity issues if the astig- MANAGEMENT matism is not addressed. I believe that correction of low astigmatism, especially, is low-hanging fruit, as it provides surgeons with an additional opportunity to improve their practices. -
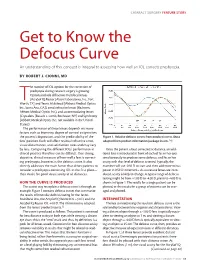
Get to Know the Defocus Curve an Understanding of This Concept Is Integral to Assessing How Well an IOL Corrects Presbyopia
CATARACT SURGERY FEATURE STORY Get to Know the Defocus Curve An understanding of this concept is integral to assessing how well an IOL corrects presbyopia. BY ROBERT J. CIONNI, MD he number of IOL options for the correction of presbyopia during cataract surgery is growing. Options include diffractive multifocal lenses (AcrySof IQ Restor [Alcon Laboratories, Inc., Fort TWorth, TX] and Tecnis Multifocal [Abbott Medical Optics Inc., Santa Ana, CA]), zonal refractive lenses (ReZoom; Abbott Medical Optics Inc.), and accommodating lenses (Crystalens [Bausch + Lomb, Rochester, NY] and Synchrony [Abbott Medical Optics Inc.; not available in the United States]). The performance of these lenses depends on many factors such as biometry, degree of corneal astigmatism, the patient’s disposition, and the predictability of the Figure 1. Relative defocus curves from product inserts. (Data lens’ position. Each will affect residual refractive error, adapted from product information/package inserts.1,2) visual disturbances, and satisfaction rates and may vary by lens. Comparing the different IOLs’ performance in Once the patient is best corrected at distance, an addi- clinical practice therefore can be difficult. One strong, tional lens is introduced in front of each of his or her eyes objective, clinical measure of how well a lens is correct- simultaneously to produce some defocus, and his or her ing presbyopia, however, is the defocus curve. It also acuity with that level of defocus is tested. Typically, the directly addresses the main factor that drives patients to examiner will use -0.50 D to start and then add more minus consider a presbyopia-correcting IOL in the first place— power in 0.50 D increments. -

A Bright Vision for the Future
RetinaReview A newsletter from the Wilmer Eye Institute at Johns Hopkins SUMMER 2013 A Bright Vision for the Future here’s little doubt that improve patient outcomes in the Wilmer faculty. Our eight other diseases and disorders in years ahead. Fernando Arevalo assistant and associate retina pro- ophthalmology, specifi- serves as chief of the retina service fessors—unquestionably some of Tcally those that involve the for Wilmer’s collaboration with the the brightest stars in ophthalmol- retina, are some of the most vex- King Khaled Eye Specialist Hospital ogy—are bringing fresh insights and ing conditions in medicine today. in Riyadh, Saudi Arabia. From energy to today’s major challenges Retinal detachment, retinitis pig- 2006 to 2012, Neil Bressler led in retina research and patient care. mentosa, and retinal vein occlusion the National Institutes of Health- Read on to learn about how these are among retina conditions that sponsored Diabetic Retinopathy junior faculty members are working rob the vision of countless children Clinical Research Network, likely to harness telemedicine in the treat- and adults throughout the world. the largest collaborative clinical ment of retina diseases, attacking The good news? Thanks to ongo- research program in retina in the vision loss from retinal detachment ing advances by Wilmer’s retina world, and now serves as Past Chair. surgery or poor circulation to the specialists, dramatic strides are being retina, developing new imaging made. The most common causes of WILMER RETINA DIVISION and robotic approaches to retinal blindness, if left untreated, are reti- BY THE NUMBERS disease, and taking their renowned nal diseases, including age-related treatments and research to those macular degeneration and diabetic 7 Number of endowed throughout the region.