An in Vitro Investigation Into the Mechanism of the Clinically Relevant Drug-Drug Interaction Between Omeprazole Or Esomeprazole and Clopidogrel
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Summary of Product Characteristics
Sandoz Business use only Page 1 of 9 1.3.1 spc-label-pl - common-spc – 11,006 20191218 (DE/H/1772/001-002-003 – 155347 - validation) TORASEMIDE 100 MG, 200 MG, 50 MG, TABLET 721-6534.01, 721-6535.01, 721-6536.01 SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT [Nationally completed name] 50 mg tablets [Nationally completed name] 100 mg tablets [Nationally completed name] 200 mg tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each tablet contains 50 mg of torasemide. Each tablet contains 100 mg of torasemide. Each tablet contains 200 mg of torasemide. For excipients, see section 6.1 3. PHARMACEUTICAL FORM Tablet. 50 mg tablets: White to off-white round tablet. 100 mg tablets: White to off-white round tablet with break notch. The tablet can be divided into equal doses. 200 mg tablets: White to off-white round tablet with cross break notch on both sides. The tablet can be divided into four equal doses. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications The administration of [Nationally completed name] 50 mg/- 100 mg/- 200 mg tablets is exclusively indicated in patients with highly reduced renal function (creatinine clearance less than 20 ml/min and/or serum creatinine concentration greater than 6 mg/dl). For maintenance of residual diuresis in case of severe renal insufficiency – even on dialysis if there is a considerable residual diuresis (more than 200 ml/24 hours) – if oedemas, effusions and/or hypertension exist. Note: [Nationally completed name] 50 mg/- 100 mg/- 200 mg tablets tablets are to be used only in case of highly impaired and not in normal renal function. -

Health Reports for Mutual Recognition of Medical Prescriptions: State of Play
The information and views set out in this report are those of the author(s) and do not necessarily reflect the official opinion of the European Union. Neither the European Union institutions and bodies nor any person acting on their behalf may be held responsible for the use which may be made of the information contained therein. Executive Agency for Health and Consumers Health Reports for Mutual Recognition of Medical Prescriptions: State of Play 24 January 2012 Final Report Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Acknowledgements Matrix Insight Ltd would like to thank everyone who has contributed to this research. We are especially grateful to the following institutions for their support throughout the study: the Pharmaceutical Group of the European Union (PGEU) including their national member associations in Denmark, France, Germany, Greece, the Netherlands, Poland and the United Kingdom; the European Medical Association (EMANET); the Observatoire Social Européen (OSE); and The Netherlands Institute for Health Service Research (NIVEL). For questions about the report, please contact Dr Gabriele Birnberg ([email protected] ). Matrix Insight | 24 January 2012 2 Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Executive Summary This study has been carried out in the context of Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients’ rights in cross- border healthcare (CBHC). The CBHC Directive stipulates that the European Commission shall adopt measures to facilitate the recognition of prescriptions issued in another Member State (Article 11). At the time of submission of this report, the European Commission was preparing an impact assessment with regards to these measures, designed to help implement Article 11. -

Cilostazol Protects Rats Against Alcohol‑Induced Hepatic Fibrosis Via Suppression of TGF‑Β1/CTGF Activation and the Camp/Epac1 Pathway
EXPERIMENTAL AND THERAPEUTIC MEDICINE 17: 2381-2388, 2019 Cilostazol protects rats against alcohol‑induced hepatic fibrosis via suppression of TGF‑β1/CTGF activation and the cAMP/Epac1 pathway KUN HAN, YANTING ZHANG and ZHENWEI YANG Department of Gastroenterology, Xi'an Central Hospital, Xi'an, Shaanxi 710003, P.R. China Received July 2, 2018; Accepted November 23, 2018 DOI: 10.3892/etm.2019.7207 Abstract. Alcohol abuse and chronic alcohol consump- Introduction tion are major causes of alcoholic liver disease worldwide, particularly alcohol‑induced hepatic fibrosis (AHF). Liver Liver fibrosis is a wound‑healing response to a variety of liver fibrosis is an important public health concern because of its insults, including excessive alcohol intake. Alcohol abuse and high morbidity and mortality. The present study examined chronic alcohol consumption are major causes of alcoholic the mechanisms and effects of the phosphodiesterase III liver disease (ALD) worldwide (1). Alcohol‑induced hepatic inhibitor cilostazol on AHF. Rats received alcohol infu- fibrosis (AHF) may cause serious hepatic cirrhosis, and is sions via gavage to induce liver fibrosis and were treated widely accepted as a milestone event in ALD (2). However, with colchicine (positive control) or cilostazol. The serum recent evidence indicates that liver fibrosis is reversible and alcohol dehydrogenase (ADH) and acetaldehyde dehydro- that the liver may recover from cirrhosis (3). Therefore, eluci- genase (ALDH) activities and the albumin/globulin (A/G), dation of the cellular and molecular mechanisms is urgently enzymes and hyaluronic acid (HA), type III precollagen required to prevent AHF. (PC III), laminin (LA), and type IV collagen (IV‑C) levels The exact mechanism remains unclear, but certain changes were measured using commercially available kits. -
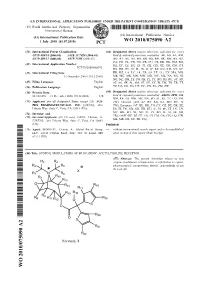
Wo 2010/075090 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 1 July 2010 (01.07.2010) WO 2010/075090 A2 (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C07D 409/14 (2006.01) A61K 31/7028 (2006.01) kind of national protection available): AE, AG, AL, AM, C07D 409/12 (2006.01) A61P 11/06 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/US2009/068073 HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 15 December 2009 (15.12.2009) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (25) Filing Language: English SE, SG, SK, SL, SM, ST, SV, SY, TJ, TM, TN, TR, TT, (26) Publication Language: English TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 61/122,478 15 December 2008 (15.12.2008) US kind of regional protection available): ARIPO (BW, GH, GM, KE, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, ZM, (71) Applicant (for all designated States except US): AUS- ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, PEX PHARMACEUTICALS, INC. -

PHARMACEUTICAL APPENDIX to the TARIFF SCHEDULE 2 Table 1
Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names INN which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service CAS registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. -

A Systematic Review of Proton Pump Inhibitors for the Treatment of Adult Patients with Symptomatic Gastroesophageal Reflux Disease Or Peptic Ulcer Disease
Title A systematic review of proton pump inhibitors for the treatment of adult patients with symptomatic gastroesophageal reflux disease or peptic ulcer disease. Review Question(s) Requested Requested by PSD 1. What is the comparative effectiveness of different proton pump inhibitors in patients with symptoms of gastroesophageal reflux disease? 2. What is the comparative effectiveness of different proton pump inhibitors in treating peptic (duodenal and gastric) ulcer? 3. What are the comparative safety and adverse events of different proton pump inhibitors in patients being treated for symptoms of gastroesophageal reflux disease and peptic ulcer? 4. Are there subgroups of patients based on demographics, other medications, or comorbidities (including nasogastric tubes and inability to swallow solid oral medication) for which a particular proton pump inhibitor or preparation is more effective or associated with fewer adverse effects? Drug The following five proton pump inhibitors (PPI) drugs will be reviewed 1. Esomeprazole (Nexium® and its generic equivalent) 2. Lansoprazole (Prevacid® and its generic equivalent) 3. Omeprazole* (Losec® and its generic equivalent) 4. Pantoprazole* sodium and magnesium (Pantoloc®, Panto IV and their generic equivalent and Tecta® 5. Rabeprazole* (Pariet® and its generic equivalent) Note: *Omeprazole, Pantoprazole and Rabeprazole have been identified as reference drugs by PSD. Esomeprazole and Lansoprazole will be compared to these three reference drugs. TABLE OF CONTENTS TABLE OF CONTENTS ..........................................................................................................................2 -

Ovid MEDLINE(R)
Supplementary material BMJ Open Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations and Daily <1946 to September 16, 2019> # Searches Results 1 exp Hypertension/ 247434 2 hypertens*.tw,kf. 420857 3 ((high* or elevat* or greater* or control*) adj4 (blood or systolic or diastolic) adj4 68657 pressure*).tw,kf. 4 1 or 2 or 3 501365 5 Sex Characteristics/ 52287 6 Sex/ 7632 7 Sex ratio/ 9049 8 Sex Factors/ 254781 9 ((sex* or gender* or man or men or male* or woman or women or female*) adj3 336361 (difference* or different or characteristic* or ratio* or factor* or imbalanc* or issue* or specific* or disparit* or dependen* or dimorphism* or gap or gaps or influenc* or discrepan* or distribut* or composition*)).tw,kf. 10 or/5-9 559186 11 4 and 10 24653 12 exp Antihypertensive Agents/ 254343 13 (antihypertensiv* or anti-hypertensiv* or ((anti?hyperten* or anti-hyperten*) adj5 52111 (therap* or treat* or effective*))).tw,kf. 14 Calcium Channel Blockers/ 36287 15 (calcium adj2 (channel* or exogenous*) adj2 (block* or inhibitor* or 20534 antagonist*)).tw,kf. 16 (agatoxin or amlodipine or anipamil or aranidipine or atagabalin or azelnidipine or 86627 azidodiltiazem or azidopamil or azidopine or belfosdil or benidipine or bepridil or brinazarone or calciseptine or caroverine or cilnidipine or clentiazem or clevidipine or columbianadin or conotoxin or cronidipine or darodipine or deacetyl n nordiltiazem or deacetyl n o dinordiltiazem or deacetyl o nordiltiazem or deacetyldiltiazem or dealkylnorverapamil or dealkylverapamil -

Cilostazol Tablets, USP50 Mg and 100 Mgrx Only
CILOSTAZOL - cilostazol tablet Physicians Total Care, Inc. ---------- Cilostazol Tablets, USP 50 mg and 100 mg Rx only CONTRAINDICATION Cilostazol and several of its metabolites are inhibitors of phosphodiesterase III. Several drugs with this pharmacologic effect have caused decreased survival compared to placebo in patients with class III-IV congestive heart failure. Cilostazol is contraindicated in patients with congestive heart failure of any severity. DESCRIPTION Cilostazol is a quinolinone derivative that inhibits cellular phosphodiesterase (more specific for phosphodiesterase III). The empirical formula of cilostazol is C20H27N5O2, and its molecular weight is 369.46. Cilostazol is 6-[4-(1-cyclohexyl-1H-tetrazol-5-yl)butoxy]-3,4-dihydro-2(1H)-quinolinone, CAS-73963-72-1. The structural formula is: Cilostazol occurs as white to off-white crystals or as a crystalline powder that is slightly soluble in methanol and ethanol, and is practically insoluble in water, 0.1 N HCl, and 0.1 N NaOH. Cilostazol Tablets, USP for oral administration are available as 50 mg or 100 mg round, white debossed tablets. Each tablet, in addition to the active ingredient, contains the following inactive ingredients: carboxymethylcellulose calcium, corn starch, hypromellose, magnesium stearate and microcrystalline cellulose. CLINICAL PHARMACOLOGY Mechanism of Action The mechanism of the effects of Cilostazol Tablets, USP on the symptoms of intermittent claudication is not fully understood. Cilostazol Tablets, USP and several of its metabolities are cyclic AMP (cAMP) phosphodiesterase III inhibitors (PDE III inhibitors), inhibiting phosphodiesterase activity and suppressing cAMP degration with a resultant increase in cAMP in platelets and blood vessels, leading to inhibition of platelet aggregation and vasodilation, respectively. -

Diuretics in Clinical Practice. Part I: Mechanisms of Action, Pharmacological Effects and 1
Review Diuretics in clinical practice. Part I: mechanisms of action, pharmacological effects and 1. Introduction clinical indications of diuretic 2. Principles of diuretic action and classification of diuretic compounds compounds † 3. Carbonic anhydrase inhibitors Pantelis A Sarafidis , Panagiotis I Georgianos & Anastasios N Lasaridis Aristotle University of Thessaloniki, AHEPA Hospital, Section of Nephrology and Hypertension, 4. Osmotic diuretics 1st Department of Medicine, Thessaloniki, St. Kiriakidi 1, 54636, Thessaloniki, Greece 5. Loop diuretics 6. Thiazides and thiazide-related Importance of the field: Diuretics are among the most important drugs of our diuretics therapeutic armamentarium and have been broadly used for > 50 years, 7. Potassium-retaining diuretics providing important help towards the treatment of several diseases. Although all diuretics act primarily by impairing sodium reabsorption in the renal 8. Conclusion tubules, they differ in their mechanism and site of action and, therefore, in 9. Expert opinion their specific pharmacological properties and clinical indications. Loop diure- tics are mainly used for oedematous disorders (i.e., cardiac failure, nephrotic syndrome) and for blood pressure and volume control in renal disease; thiazides and related agents are among the most prescribed drugs for hypertension treatment; aldosterone-blockers are traditionally used for primary or secondary aldosteronism; and other diuretic classes have more specific indications. Areas covered in this review: This article discusses the mechanisms of action, pharmacological effects and clinical indications of the various diuretic classes For personal use only. used in everyday clinical practice, with emphasis on recent knowledge sug- gesting beneficial effects of certain diuretics on clinical conditions distinct from the traditional indications of these drugs (i.e., heart protection for aldosterone blockers). -

Diuretic-Induced Hyponatraemia in Elderly Hypertensive Women
Journal of Human Hypertension (2003) 17, 151 & 2003 Nature Publishing Group All rights reserved 0950-9240/03 $25.00 www.nature.com/jhh LETTER TO THE EDITOR Diuretic-induced hyponatraemia in elderly hypertensive women Journal of Human Hypertension there were 10 with plasma so- plasma sodium of 111 mmol/l (2003) 17, 151. doi:10.1038/ dium levels in the range 101– when inadvertently rechallenged sj.jhh.1001513 109 mmol/l. Of the 26, 11 had with thiazides, the agent this time plasma potassium levels less than being hydrochlorothiazide copre- My experience of diuretic- 3.5 mmol/l. The age range was scribed with amiloride. I now induced hyponatraemia in the 74–93 and 22 were women. Hy- utilise torasemide as an adjunc- elderly is in accordance with the drochlorothiazide was the offend- tive diuretic in patients with a observations made by the ing agent in 12 cases, having been previous history of thiazide- authors.1 In my personal series coprescribed with amiloride in induced hyponatraemia. The data of 61 cases of severe hyponatraemia 10 instances, and with triamterene presented here extend the obser- (plasma sodium o120 mmol/l), in two. Bendrofluazide was the vations I published previously on compiled over a period of 18 offending agent in nine instances, this topic. years in patients aged 465, 26 the dose being 2.5 mg/day in were attributable to thiazide seven instances (coprescribed diuretics, culprit drugs in seven with amiloride in one instance), References other cases being frusemide (three and 5.0 mg/day in the other two. 1 Sharabi Y et al. -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG .