Phase II Two-Arm Study of Tepotinib + Osimertinib in Patients with EGFR-Mutant NSCLC and Acquired
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Positive Effects of Trilaciclib on Patient
POSITIVE EFFECTS OF TRILACICLIB ON PATIENT MYELOSUPPRESSION-RELATED SYMPTOMS AND FUNCTIONING: RESULTS FROM THREE PHASE 2 RANDOMIZED, DOUBLE-BLIND, PLACEBO-CONTROLLED SMALL CELL LUNG CANCER TRIALS J Weiss1, K Skaltsa2, C Gwaltney2, D Daniel3, S Adler4, S Wolfe4, RK Malik4, SR Morris4, JM Antal4, Z Andric5 UNC Lineberger Comprehensive Cancer Center1; IQVIA2; Sarah Cannon, Tennessee Oncology – Chattanooga3; G1 Therapeutics4; Clinical Hospital Centre Bezanijska Kosa5 Conflict of Interest Disclosure Shannon Morris, MD, PhD • Salary: G1Therapeutics • Receipt of Intellectual Property Rights/Patent Holder: GlaxoSmithKline • Ownership Interest (stocks, stock options or other ownership interest excluding diversified mutual funds): G1 Therapeutics, GlaxoSmithKline Myelosuppression: despite the availability of interventions like G-CSF, ESAs and transfusions, there is still significant unmet medical need for patients 1st Line SCLC 2nd Line SCLC Current Incidence of Incidence of Current Unmet Needs Interventions Grade 3/41 Grade 3/42 ~70% bone pain (~25% severe3) induced by G-CSFs 54% Neutropenia 23% G-CSF (severe pain treated with NSAIDs, antihistamines, (3% FN) and opioids) Box warning for shortened overall survival and ESA rescue, Anemia 14% 31% increased risk of tumor progression; increased risk transfusion rescue of thromboembolic disease Thrombocytopenia 10% 54% Transfusion rescue No options other than transfusions Trilaciclib has the potential to prevent multi-lineage myelosuppression and reduce the need for these interventions and their associated side effects Sources: 1IMpower133 Trial, atezolizumab + E/P arm (n=198), NEJM, 2018; 2von Pawel J, et al. J Clin. Oncol. 2014;32:4012-4019; 2Kirshner et al: Prevention of pegfilgrastim-induced bone pain. JCO, 2012. Trilaciclib, a First-in-Class Myelopreservation Agent, Improves Patient Outcomes when Combined with Chemotherapy SCLC HSPC Trilaciclib transiently blocks progression through the cell cycle, thereby protecting HSPCs from damage by chemotherapy . -
Treatment and Testing Guidelines
For patients with METex14 and BRAF V600E in mNSCLC, TREATMENT AND TESTING GUIDELINES METex14 BRAF V600E BRAF, v-raf murine sarcoma viral oncogene homolog B1; MET, mesenchymal-epithelial transition; METex14, MET exon 14 skipping; mNSCLC, metastatic non-small cell lung cancer. Indication Indication TABRECTA® (capmatinib) tablets is indicated for the TAFINLAR® (dabrafenib) capsules, in combination with treatment of adult patients with metastatic non-small MEKINIST® (trametinib) tablets, is indicated for the cell lung cancer (NSCLC) whose tumors have a mutation treatment of patients with metastatic non-small cell that leads to mesenchymal-epithelial transition (MET) lung cancer (NSCLC) with BRAF V600E mutation as exon 14 skipping as detected by an FDA-approved test. detected by an FDA-approved test. This indication is approved under accelerated approval Limitation of Use: TAFINLAR is not indicated for the based on overall response rate and duration of treatment of patients with wild-type BRAF NSCLC. response. Continued approval for this indication may be contingent upon verification and description of clinical Important Safety Information benefit in confirmatory trials. New Primary Malignancies. Important Safety Information Cutaneous Malignancies Interstitial Lung Disease (ILD)/Pneumonitis. Across clinical trials of TAFINLAR administered with ILD/pneumonitis, which can be fatal, occurred in MEKINIST (“the combination”), the incidence patients treated with TABRECTA. ILD/pneumonitis of cutaneous squamous cell carcinomas (cuSCCs), occurred in 4.5% of patients treated with TABRECTA including keratoacanthomas, occurred in 2% of in the GEOMETRY mono-1 study, with 1.8% of patients patients. Basal cell carcinoma and new primary experiencing grade 3 ILD/pneumonitis and 1 patient melanoma occurred in 3% and <1% of patients, experiencing death (0.3%). -

Resistance Mechanisms to Osimertinib in EGFR-Mutated Non-Small Cell Lung Cancer
www.nature.com/bjc REVIEW ARTICLE Resistance mechanisms to osimertinib in EGFR-mutated non-small cell lung cancer Alessandro Leonetti1,2, Sugandhi Sharma2, Roberta Minari1, Paola Perego3, Elisa Giovannetti2,4 and Marcello Tiseo 1,5 Osimertinib is an irreversible, third-generation epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor that is highly selective for EGFR-activating mutations as well as the EGFR T790M mutation in patients with advanced non-small cell lung cancer (NSCLC) with EGFR oncogene addiction. Despite the documented efficacy of osimertinib in first- and second-line settings, patients inevitably develop resistance, with no further clear-cut therapeutic options to date other than chemotherapy and locally ablative therapy for selected individuals. On account of the high degree of tumour heterogeneity and adaptive cellular signalling pathways in NSCLC, the acquired osimertinib resistance is highly heterogeneous, encompassing EGFR-dependent as well as EGFR- independent mechanisms. Furthermore, data from repeat plasma genotyping analyses have highlighted differences in the frequency and preponderance of resistance mechanisms when osimertinib is administered in a front-line versus second-line setting, underlying the discrepancies in selection pressure and clonal evolution. This review summarises the molecular mechanisms of resistance to osimertinib in patients with advanced EGFR-mutated NSCLC, including MET/HER2 amplification, activation of the RAS–mitogen-activated protein kinase (MAPK) or RAS–phosphatidylinositol -
Crusader Q2 2020 Research Edition Download
Your resource for the latest research into the MET alteration. CRUSADER NEWSLETTER Q2 2020 RESEARCH EDITION MET Crusaders is a community of Lung Cancer patients and care givers collaborating with advocates and medical professionals collectively dedicated to helping patients with a MET alteration live normal lives. Come Join Us! [email protected] In this edition Top-level MET gene copy number gain defines .................... 2 Molecular Mechanisms of Acquired Resistance ................... 5 a subtype of poorly differentiated pulmonary to MET Tyrosine Kinase Inhibitors in Patients adenocarcinomas with poor prognosis with MET Exon 14-Mutant NSCLC EDITOR Characteristics and Clinical Outcomes of ............................. 2 MET Alterations Are a Recurring and Actionable .................. 6 Jessica McKernan, PharmD Non-Small Cell Lung Cancer Patients in Korea Resistance Mechanism in ALK-Positive Lung Cancer with MET Exon 14 Skipping Atrium Health Tepotinib in Non-Small-Cell Lung Cancer with ...................... 6 Charlotte, NC Clinical and molecular correlates of PD-L1 ........................... 2 MET Exon 14 Skipping Mutations (VISION Trial) expression in patients with lung adenocarcinomas Therapeutic Efficacy of ABN401, a Highly ............................. 7 CONTRIBUTING EDITORS Efficacy and Safety of Anti-PD-1 Immunotherapy ................. 3 Potent and Selective MET Inhibitor, Based on Julia Stevens, PharmD in Patients With Advanced NSCLC With BRAF, HER2, Diagnostic Biomarker Test in MET-Addicted Cancer or MET Mutations or RET Translocation: GFPC 01-2018 Beth Israel Deaconess Erlotinib plus tivantinib versus erlotinib alone ..................... 7 Medical Center Alterations in the PI3K Pathway Drive Resistance ................ 3 in patients with previously treated stage IIIb/IV Boston, MA to MET Inhibitors in NSCLC Harboring MET non-small-cell lung cancer: A meta-analysis based Exon 14 Skipping Mutations on randomized controlled trials Laura Schmidt, PharmD Incidence and PD-L1 Expression of MET 14 ......................... -
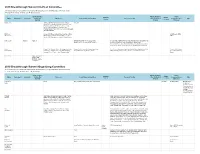
2019 Breakthrough Summit Co-Host Committee 2019 Breakthrough
2019 Breakthrough Summit Co-Host Committee All relationships are considered compensated. Relationships are self-held unless otherwise noted. I = Immediate Family Member, Inst = My Institution Stock and Other Patents, Royalties, Travel, Speakers' Expert Name Employment Leadership Ownership Honoraria Consulting or Advisory Role Research Funding Other Intellectual Accommodations, Other Bureau Testimony Interests Property Expenses Dae Ho Lee Abbvie, AstraZeneca/MedImmune, Boehringer ST Cube Ingelheim, Bristol-Myers Squibb, Chong Kun Dang Pharmaceutical, CJ Healthcare, Janssen, Lilly, Merck, MSD, Mundipharma, Novartis, Ono Pharmaceutical, Pfizer, Roche/Genentech, Samyang, ST Cube, Takeda Ekaphop Amgen, AstraZeneca, Boehringer Ingelheim, Bristol- AstraZeneca, MSD, Sirachainan Myers Squibb, Diethelm Keller Logistics, LF Asia, Pfizer Merck, MSD, Mundipharma, Roche, Sanofi/Aventis Lillian L. Siu Agios (I) Agios (I) AstraZeneca/MedImmune, Loxo, Merck, Amgen (Inst), Astellas Pharma (Inst), AstraZeneca (Inst), Bayer (Inst), MorphoSys, Roche, Symphony Evolution Boehringer Ingelheim (Inst), Bristol-Myers Squibb (Inst), Genentech/Roche (Inst), GlaxoSmithKline (Inst), MedImmune (Inst), Merck (Inst), Novartis (Inst), Pfizer (Inst), Symphony Evolution (Inst) Virote Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Amgen, AstraZeneca, Boehringer Ingelheim, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Eisai, Lilly, Amgen, AstraZeneca, Sriuranpong Bristol-Myers Squibb, Eisai, Lilly, MSD Oncology, Eisai, MSD Oncology, Novartis, Roche MSD Oncology, -

Tepotinib) Tablets, for Oral Use Any Severity
HIGHLIGHTS OF PRESCRIBING INFORMATION ------------------------WARNINGS AND PRECAUTIONS----------------------- These highlights do not include all the information needed to use TEPMETKO safely and effectively. See full prescribing information for • Interstitial Lung Disease (ILD)/Pneumonitis: Immediately withhold TEPMETKO. TEPMETKO in patients with suspected ILD/pneumonitis. Permanently discontinue TEPMETKO in patients diagnosed with ILD/pneumonitis of TEPMETKO® (tepotinib) tablets, for oral use any severity. (2.3, 5.1) Initial U.S. Approval: 2021 • Hepatotoxicity: Monitor liver function tests. Withhold, dose reduce, or permanently discontinue TEPMETKO based on severity. (5.2) ----------------------------INDICATIONS AND USAGE--------------------------- • Embryo-fetal toxicity: TEPMETKO can cause fetal harm. Advise of potential risk to a fetus and use of effective contraception. (5.3, 8.1, 8.3) TEPMETKO is a kinase inhibitor indicated for the treatment of adult patients with metastatic non-small cell lung cancer (NSCLC) harboring mesenchymal- -------------------------------ADVERSE REACTIONS------------------------------ epithelial transition (MET) exon 14 skipping alterations. (1) Most common adverse reactions (≥ 20%) were edema, fatigue, nausea, This indication is approved under accelerated approval based on overall diarrhea, musculoskeletal pain, and dyspnea. The most common Grade 3 to 4 response rate and duration of response. Continued approval for this indication laboratory abnormalities (≥ 2%) were decreased lymphocytes, decreased may be contingent upon verification and description of clinical benefit in albumin, decreased sodium, increased gamma-glutamyltransferase, increased confirmatory trials. (1) amylase, increased ALT, increased AST, and decreased hemoglobin. (6.1) -----------------------DOSAGE AND ADMINISTRATION----------------------- To report SUSPECTED ADVERSE REACTIONS, contact EMD Serono at 1-800-283-8088 ext. 5563 or FDA at 1-800-FDA-1088 or • Select patients for treatment with TEPMETKO on the presence of METex14 www.fda.gov/medwatch. -

First-Line Treatment Options for Patients with Stage IV Non-Small Cell Lung Cancer with Driver Alterations
First-Line Treatment Options for Patients with Stage IV Non-Small Cell Lung Cancer with Driver Alterations Patients with stage IV non-small cell lung cancer Nonsquamous cell carcinoma and squamous cell carcinoma Activating EGFR mutation other Sensitizing (L858R/exon 19 MET exon 14 skipping than exon 20 insertion mutations, EGFR exon 20 mutation ALK rearrangement ROS1 rearrangement BRAF V600E mutation RET rearrangement NTRK rearrangement mutations KRAS alterations HER2 alterations NRG1 alterations deletion) EGFR mutation T790M, L858R or Ex19Del PS 0-2 Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options PS 0-2 Treatment Options Emerging target; no Emerging target; no Emerging target; no Platinum doublet † † † Osimertinib monotherapy S Afatinib monotherapy M M Alectinib S Entrectinib M Dabrafenib/trametinib M Capmatinib M Selpercatinib M Entrectinib M conclusions available conclusions available conclusions available chemotherapy ± bevacizumab Gefitinib with doublet Standard treatment based on Standard treatment based on Standard treatment based on M M M Brigatinib S Crizotinib M M Tepotinib M Pralsetinib* W Larotrectinib M chemotherapy non-driver mutation guideline non-driver mutation guideline non-driver mutation guideline If alectinib or brigatinib are not available If entrectinib or crizotinib are not available Standard treatment based on Standard treatment based on Standard treatment based on Dacomitinib monotherapy M Osimertinib W M M M Ceritinib S Ceritinib W non-driver mutation guideline non-driver mutation guideline non-driver mutation guideline Monotherapy with afatinib M Crizotinib S Lortlatinib W Standard treatment based on Erlotinib/ramucirumab M M non-driver mutation guideline Erlotinib/bevacizumab M Monotherapy with erlotinib M Strength of Recommendation Monotherapy with gefitinib M S Strong M Moderate W Weak Monotherapy with icotinib M Notes. -

Original Article the Selective C-Met Inhibitor Tepotinib Can Overcome
Am J Cancer Res 2017;7(4):962-972 www.ajcr.us /ISSN:2156-6976/ajcr0053156 Original Article The selective c-Met inhibitor tepotinib can overcome epidermal growth factor receptor inhibitor resistance mediated by aberrant c-Met activation in NSCLC models Manja Friese-Hamim1, Friedhelm Bladt2, Giuseppe Locatelli2, Uz Stammberger3, Andree Blaukat3 1Translational In Vivo Pharmacology, 2Translational and Biomarker Research, 3Global Research and Development, Merck KGaA, Darmstadt, Germany Received March 17, 2017; Accepted March 27, 2017; Epub April 1, 2017; Published April 15, 2017 Abstract: Non-small cell lung cancer (NSCLC) sensitive to first-generation epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) often acquires resistance through secondary EGFR mutations, including the T790M mutation, aberrant c-Met receptor activity, or both. We assessed the ability of the highly selective c-Met inhibitor tepotinib to overcome EGFR TKI resistance in various xenograft models of NSCLC. In models with EGFR-activating mutations and low c-Met expression (patient explant-derived LU342, cell line PC-9), EGFR TKIs caused tumors to shrink, but growth resumed upon cessation of treatment. Tepotinib combined with EGFR TKIs delayed tumor regrowth, while tepotinib alone was ineffective. In patient explant-derived LU858, which has an EGFR-activating mutation and expresses high levels of c-Met/HGF, EGFR TKIs had no effect on tumor growth. Tepotinib combined with EGFR TKIs caused complete tumor regression and tepotinib alone caused tumor stasis. In cell line DFCI081 (activating EGFR mutation, c-Met amplification), EGFR TKIs were ineffective, whereas tepotinib alone induced com- plete tumor regression. Finally, in a ‘double resistant’ EGFR T790M-positive, high c-Met model (cell line HCC827-GR- T790M), the EGFR TKIs erlotinib, afatinib, and rociletinib, as well as tepotinib as a single agent or in combination with erlotinib or afatinib, slowed tumor growth, but only tepotinib in combination with rociletinib induced complete tumor regression. -

Investor Day March 6, 2019
Investor Day March 6, 2019 www.g1therapeutics.com NASDAQ: GTHX 1 Forward-looking statements This presentation and the accompanying oral commentary contain “forward-looking” statements within the meaning of the Private Securities Litigation Reform Act of 1995. Words such as "may," "will," "expect," "plan," "anticipate," "estimate," "intend" and similar expressions (as well as other words or expressions referencing future events, conditions or circumstances) are intended to identify forward-looking statements. Forward-looking statements in this presentation include, but are not limited to the following: the therapeutic potential of trilaciclib, lerociclib and G1T48; initial success in our ongoing clinical trials may not be indicative of results obtained when these trials are completed or in later stage trials; our development of trilaciclib to reduce chemotherapy-induced myelosuppression is novel, unproven and rapidly evolving and may never lead to a marketable product; our product candidates may cause undesirable side effects that could delay or prevent their marketing approval, limit the commercial profile of an approved label, or result in significant negative consequences following marketing approval, if any; we may not have the ability to recruit, enroll and complete clinical trials for, obtain approvals for, or commercialize any of our product candidates; we face substantial competition, which may result in others discovering, developing or commercializing competing products before or more successfully than we do; we may incur additional costs or experience delays in completing clinical trials; future legislation may increase the difficulty and cost for us to obtain marketing approval of and commercialize our product candidates and affect the prices we may obtain; and market conditions. -

G1 Therapeutics Presents Two Posters at ISPOR Describing The
G1 Therapeutics Presents Two Posters at ISPOR Describing the Estimated Economic Impact of Treating Myelosuppression Among Patients with Extensive-Stage Small Cell Lung Cancer May 17, 2021 - A Cost-Benefit Model of Administration of COSELATM (trilaciclib) Prior to Chemotherapy Estimates Measurable Per-Patient Cost Savings - - Myelosuppression Poses a Substantial Burden on the Health Care System Among Patients with Small Cell Lung Cancer, According to an Analysis of SEER-Medicare Data - RESEARCH TRIANGLE PARK, N.C., May 17, 2021 (GLOBE NEWSWIRE) -- G1 Therapeutics, Inc. (Nasdaq: GTHX), a commercial-stage oncology company, today presented two scientific posters at the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) describing the estimated economic impact of treating myelosuppression among patients with extensive-stage small cell lung cancer. The posters are available in the scientific publications section of the G1’s website. COSELA was approved by the U.S. Food and Drug Administration on February 12, 2021 to decrease the incidence of chemotherapy-induced myelosuppression in adult patients when administered prior to a platinum/etoposide-containing regimen or topotecan-containing regimen for ES-SCLC. Cost-Benefit Analysis of Trilaciclib for the Prevention of Chemotherapy-Induced Myelosuppression in Extensive-Stage Small Cell Lung Cancer (Deniz, B. et al.) (poster) The first poster details a cost-benefit model estimating the economic value from a U.S. commercial payer perspective of using COSELA™ (trilaciclib) prior to chemotherapy in patients with extensive-stage small cell lung cancer (ES-SCLC). According to the model, the estimated potential total cost savings per patient is $15,006 – savings that are based on a projected reduction in myelosuppressive adverse events (AEs) and their associated treatment costs. -

Next Generation Immuno-Oncology Targeting Hot and Cold Tumors
Next generation immuno-oncology targeting hot and cold tumors March 2017 iTeos – General Disclaimer Company Presentation “This presentation has been prepared by iTeos and is furnished to you by iTeos on a confidential basis and solely for your information. This presentation contains forward-looking statements, including (without limitation) statements concerning the progress and expectations of our (pre-)clinical pipeline and the financials of the company. When used in this presentation, the words “anticipate,” “believe,” “can,” “could,” “estimate,” “expect,” “intend,” “is designed to,” “may,” “might,” “will,” “plan,” “potential,” “possible,” “predict,” “objective,” “should,” and similar expressions are intended to identify forward- looking statements. Forward-looking statements involve known and unknown risks, uncertainties and other factors which might cause the actual results, financial condition, performance or achievements of iTeos, or industry results, to be materially different from any future results, financial conditions, performance or achievements expressed or implied by such forward-looking statements. All statements contained herein speak only as of the release date of this document. iTeos expressly disclaims any obligation to update any statement in this document to reflect any change or future development with respect thereto, any future results, or any change in events, conditions and/or circumstances on which any such statement is based, unless specifically required by law or regulation. Neither iTeos nor any of its officers, -

In Bladder Cancer
G1 Therapeutics Initiates PRESERVE 3, A Randomized Phase 2 Study of COSELA™ (trilaciclib) in Bladder Cancer June 14, 2021 - The Primary Endpoint of PRESERVE 3 Will Assess the Anti-Tumor Efficacy of COSELA with Platinum-Based Chemotherapy Followed by COSELA in Combination with Immune Checkpoint Inhibitor Avelumab in 90 Patients with Metastatic Urothelial Carcinoma (mUC) - RESEARCH TRIANGLE PARK, N.C., June 14, 2021 (GLOBE NEWSWIRE) -- G1 Therapeutics, Inc. (Nasdaq: GTHX), a commercial-stage oncology company, today announced that the Company has initiated PRESERVE 3, a Phase 2, randomized, open-label study of COSELA™ (trilaciclib) administered with first-line platinum-based chemotherapy and the immune checkpoint inhibitor avelumab maintenance therapy in patients with untreated, locally advanced or metastatic urothelial carcinoma (mUC). Myeloprotection and anti-tumor efficacy endpoints are being assessed in this study. Initial results of this study are expected in the second half of 2022. “Bladder cancer is unfortunately common and the five-year survival rate for metastatic urothelial carcinoma has not changed in the last 25 years, highlighting the need for new and well tolerated therapies specifically tailored for immune sensitive tumors like this,” said Raj Malik, M.D., Chief Medical Officer at G1 Therapeutics. “While chemotherapy followed by avelumab maintenance therapy has proven to be a meaningful step forward for the 1L treatment of patients with mUC, patients may not receive the maximal benefit for a variety of reasons. These Phase 2 data will be instructional and important to evaluate the benefit of adding COSELA to this regimen, and if positive, would be quickly followed by a Phase 3 registrational trial.” Patient recruitment in Preserve 3 is now underway.