Feasibility and First Reports of the MATCH-R Repeated Biopsy Trial At
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PULSE: Speaker Biographies March 2019
PULSE: Speaker Biographies March 2019 Supported by @BIA_UK www.bioindustry.org In order of appearance: Dr Barbara Domayne-Hayman Entrepreneur-in-residence, Francis Crick Institute, CBO, Autifony Therapeutics Ltd and formerly Chairman, Puridify Barbara has worked on the commercial side of life sciences for thirty years, first in a large organisation (ICI/Zeneca/AstraZeneca), before transitioning to the entrepreneurial world of biotech. Barbara joined the Francis Crick Institute in January 2018 as Entrepreneur-in- residence. She is also Chief Business officer of Autifony, where she is responsible for strategic partnering, fundraising and commercial aspects of drug development for CNS disorders. In December 2017 Autifony signed a major collaboration with Boehringer Ingelheim. Barbara was also Chair of Puridify, a UCL spin-out with a breakthrough biotherapeutics purification technology, which was acquired by GE in November 2017. She chairs the LifeArc Seed Fund investment committee, and is on the Cambridge Enterprise Seed Fund Investment Committee. Previously, Barbara was CEO of Stabilitech, and she was Commercial Director at Arrow Therapeutics until the company was acquired by AstraZeneca. Barbara was also Senior Business Development Manager at Celltech. Barbara has a BA and D Phil in Chemistry from the University of Oxford, and is a Sloan Fellow from London Business School. Steve Bates, OBE CEO, BioIndustry Association Since his appointment as Chief Executive of the BioIndustry Association in 2012, Steve has led major BIA campaigns for, amongst other things, improved access to finance, the refilling of the Biomedical Catalyst, anti-microbial resistance and the opportunity the sector presents to generalist long term investors. Steve champions the adaptive pathway approach to the licensing of new drugs, the need for Early Access and is particularly proud of the working relationship the BIA has established with the UK’s leading medical research charities. -
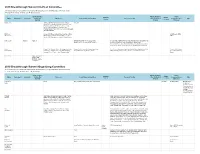
2019 Breakthrough Summit Co-Host Committee 2019 Breakthrough
2019 Breakthrough Summit Co-Host Committee All relationships are considered compensated. Relationships are self-held unless otherwise noted. I = Immediate Family Member, Inst = My Institution Stock and Other Patents, Royalties, Travel, Speakers' Expert Name Employment Leadership Ownership Honoraria Consulting or Advisory Role Research Funding Other Intellectual Accommodations, Other Bureau Testimony Interests Property Expenses Dae Ho Lee Abbvie, AstraZeneca/MedImmune, Boehringer ST Cube Ingelheim, Bristol-Myers Squibb, Chong Kun Dang Pharmaceutical, CJ Healthcare, Janssen, Lilly, Merck, MSD, Mundipharma, Novartis, Ono Pharmaceutical, Pfizer, Roche/Genentech, Samyang, ST Cube, Takeda Ekaphop Amgen, AstraZeneca, Boehringer Ingelheim, Bristol- AstraZeneca, MSD, Sirachainan Myers Squibb, Diethelm Keller Logistics, LF Asia, Pfizer Merck, MSD, Mundipharma, Roche, Sanofi/Aventis Lillian L. Siu Agios (I) Agios (I) AstraZeneca/MedImmune, Loxo, Merck, Amgen (Inst), Astellas Pharma (Inst), AstraZeneca (Inst), Bayer (Inst), MorphoSys, Roche, Symphony Evolution Boehringer Ingelheim (Inst), Bristol-Myers Squibb (Inst), Genentech/Roche (Inst), GlaxoSmithKline (Inst), MedImmune (Inst), Merck (Inst), Novartis (Inst), Pfizer (Inst), Symphony Evolution (Inst) Virote Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Amgen, AstraZeneca, Boehringer Ingelheim, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Eisai, Lilly, Amgen, AstraZeneca, Sriuranpong Bristol-Myers Squibb, Eisai, Lilly, MSD Oncology, Eisai, MSD Oncology, Novartis, Roche MSD Oncology, -

Guidelines with Regard to the Composition, Calculation and Management of the Index
INDEX METHODOLOGY Solactive Pharma Breakthrough Value Index Version 2.1 dated September 03, 2020 Contents Important Information 1. Index specifications 1.1 Short Name and ISIN 1.2 Initial Value 1.3 Distribution 1.4 Prices and Calculation Frequency 1.5 Weighting 1.6 Index Committee 1.7 Publication 1.8 Historical Data 1.9 Licensing 2. Composition of the Index 2.1 Selection of the Index Components 2.2 Ordinary Adjustment 2.3 Extraordinary Adjustment 3. Calculation of the Index 3.1 Index Formula 3.2 Accuracy 3.3 Adjustments 3.4 Dividends and other Distributions 3.5 Corporate Actions 3.6 Correction Policy 3.7 Market Disruption 3.8 Consequences of an Extraordinary Event 4. Definitions 5. Appendix 5.1 Contact Details 5.2 Calculation of the Index – Change in Calculation Method 2 Important Information This document (“Index Methodology Document”) contains the underlying principles and regulations regarding the structure and the operating of the Solactive Pharma Breakthrough Value Index. Solactive AG shall make every effort to implement regulations. Solactive AG does not offer any explicit or tacit guarantee or assurance, neither pertaining to the results from the use of the Index nor the Index value at any certain point in time nor in any other respect. The Index is merely calculated and published by Solactive AG and it strives to the best of its ability to ensure the correctness of the calculation. There is no obligation for Solactive AG – irrespective of possible obligations to issuers – to advise third parties, including investors and/or financial intermediaries, of any errors in the Index. -

Next Generation Immuno-Oncology Targeting Hot and Cold Tumors
Next generation immuno-oncology targeting hot and cold tumors March 2017 iTeos – General Disclaimer Company Presentation “This presentation has been prepared by iTeos and is furnished to you by iTeos on a confidential basis and solely for your information. This presentation contains forward-looking statements, including (without limitation) statements concerning the progress and expectations of our (pre-)clinical pipeline and the financials of the company. When used in this presentation, the words “anticipate,” “believe,” “can,” “could,” “estimate,” “expect,” “intend,” “is designed to,” “may,” “might,” “will,” “plan,” “potential,” “possible,” “predict,” “objective,” “should,” and similar expressions are intended to identify forward- looking statements. Forward-looking statements involve known and unknown risks, uncertainties and other factors which might cause the actual results, financial condition, performance or achievements of iTeos, or industry results, to be materially different from any future results, financial conditions, performance or achievements expressed or implied by such forward-looking statements. All statements contained herein speak only as of the release date of this document. iTeos expressly disclaims any obligation to update any statement in this document to reflect any change or future development with respect thereto, any future results, or any change in events, conditions and/or circumstances on which any such statement is based, unless specifically required by law or regulation. Neither iTeos nor any of its officers, -

IGNYTE-ESO: a Master Protocol to Assess Safety and Activity of Letetresgene Autoleucel (Lete-Cel; GSK3377794) Victoria L
Sandra P. D’Angelo1, Jonathan Noujaim2, Fiona Thistlethwaite3, Albiruni R. Abdul Razak4, Silvia Stacchiotti5, Warren Chow6, John B.A.G. Haanen7, Anna Chalmers8, Steven I. Robinson9, Brian A. Van Tine10, Kristen N. Ganjoo11, Melissa L. Johnson12, 13 13 13 13 13 14 15 IGNYTE-ESO: a master protocol to assess safety and activity of letetresgene autoleucel (lete-cel; GSK3377794) Victoria L. Chiou , Thomas Faitg , Mary Woessner , Laura Pearce , Aiman Shalabi , Jean-Yves Blay , George D. Demetri 1Memorial Sloan Kettering Cancer Center, New York, NY, USA; 2Institut D’Hématologie-Oncologie, Hôpital Maisonneuve-Rosemont, Montreal, QC, Canada; 3The Christie NHS Foundation Trust and University of Manchester, Manchester, United Kingdom; 4Princess Margaret Cancer Centre and in HLA-A*02+ patients with synovial sarcoma or myxoid/round cell liposarcoma (Substudies 1 and 2) Mount Sinai Hospital, Toronto, ON, Canada; 5Fondazione IRCCS Istituto Nazionale dei Tumori, Milan, Italy; 6City of Hope Comprehensive Cancer Center, Duarte, CA, United States; 7Antoni van Leeuwenhoek Ziekenhuis, Amsterdam, Netherlands; 8Huntsman Cancer Institute, University of Utah, Salt Lake City, UT, USA; 9Mayo Clinic, Rochester, MN, USA; 10Washington University in St. Louis, St. Louis, MO, USA; 11Stanford University Medical Center, Stanford, CA, USA; 12Sarah Cannon Research Institute, Nashville, TN, USA; 13GlaxoSmithKline, Philadelphia, PA, USA; Poster No. TPS11582 14Centre Léon Bérard, Lyon, France; 15Dana-Farber Cancer Institute and Ludwig Center at Harvard, Boston, MA, USA Background Study design Study phases Unmet need IGNYTE-ESO (NCT03967223) is a master protocol that enables evaluation of multiple cell therapies Figure 3 displays the patient journey for both substudies, which includes leukapheresis for lete-cel manufacture, lymphodepletion chemotherapy, lete-cel infusion, and follow-up. -

Genomic Landscape of Cell-Free DNA in Patients with Colorectal Cancer
Author Manuscript Published OnlineFirst on December 1, 2017; DOI: 10.1158/2159-8290.CD-17-1009 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Genomic landscape of cell-free DNA in patients with colorectal cancer John H. Strickler1, Jonathan M. Loree2, Leanne G. Ahronian3, Aparna R. Parikh3, Donna Niedzwiecki1, Allan Andresson Lima Pereira2, Matthew Mckinney1, W. Michael Korn4,5, Chloe E. Atreya4, Kimberly C. Banks6, Rebecca J. Nagy6, Funda Meric-Bernstam2, Richard B. Lanman6, AmirAli Talasaz6, Igor F. Tsigelny7,8, Ryan B. Corcoran3 #, Scott Kopetz2 # 1Duke University Medical Center, Durham, NC, USA; 2University of Texas MD Anderson Cancer Center, Houston, TX, USA; 3Massachusetts General Hospital Cancer Center and Department of Medicine, Harvard Medical School, Boston, MA, USA; 4Helen Diller Family Comprehensive Cancer Center, University of California, San Francisco, San Francisco, CA; Caris Life Sciences, Phoenix, AZ, USA; 6Guardant Health, Inc., Redwood City, CA, USA; 7University of California San Diego, San Diego, CA, USA; 8CureMatch Inc., San Diego, CA, USA. #To whom correspondence should be addressed: Dr. Ryan B. Corcoran Massachusetts General Hospital Cancer Center, 149 13th St., 7th floor Boston, MA 02129 Phone: 617-726-8599 Fax: 617-724-9648 Email: [email protected] Dr. Scott Kopetz University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd, Unit 426 Houston, TX 77030 Phone: 713-792-2828 Fax: 713-563-2957 Email: [email protected] 1 Downloaded from cancerdiscovery.aacrjournals.org on September 28, 2021. © 2017 American Association for Cancer Research. Author Manuscript Published OnlineFirst on December 1, 2017; DOI: 10.1158/2159-8290.CD-17-1009 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. -

Disclosure of Financial Relationships April 10-15 • May 17-21
DISCLOSURE OF FINANCIAL RELATIONSHIPS APRIL 10-15 • MAY 17-21 In compliance with the standards set by the Accreditation Council for Continuing Medical Education (ACCME), it is the policy of the American Association for Cancer Research (AACR) that the information presented at CME activities will be unbiased and based on scientific evidence. To help participants make judgments about the presence of bias, the AACR has pro- vided information that planning committee members, speakers, and abstract presenters have disclosed about financial relationships they have with commercial entities that produce or market products or services related to the content of this CME activity. Relationships are abbreviated as follows: E, Employee of listed company, G, Grant/research support recipient, A, Advisor or review panel member, C, Consultant, S, Stock Share- holder, SB, Speakers’ Bureau, H, Honoraria, O, Other. Last Name First Name Company Relationships Type Role Abate-Shen Cory NY Presbyterian Hospital Herbert Irving Comp. No Relationships Speaker Cancer Center Abdulkadir Sarki Northwestern University No Relationships Speaker Acharyya Swarnali Columbia University No Relationships Speaker Achilefu Samuel Washington University School of Medicine Sarya LLC; Integro Theranostics LLC C,O Speaker Adalsteinsson Viktor Broad Institute of MIT and Harvard Bertis Inc; AGCT GMBH A Speaker Adamopoulos Christos Icahn School of Medicine at Mount Sinai No Relationships Speaker Adamson Peter Sanofi Sanofi; AbbVie; Gilead; McKesson E,S Program Committee Agrawal Sundeep -

Compugen Ltd. (Exact Name of Registrant As Specified in Its Charter and Translation of Registrant's Name Into English) ______
UNITED STATES SECURITIES AND EXCHANGE COMMISSION WASHINGTON, D.C. 20549 FORM 20-F ☐ REGISTRATION STATEMENT PURSUANT TO SECTION 12(b) OR (g) OF THE SECURITIES EXCHANGE ACT OF 1934 OR ☒ ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 FOR THE FISCAL YEAR ENDED DECEMBER 31, 2017 OR ☐ TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 OR ☐ SHELL COMPANY REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 DATE OF EVENT REQUIRING THIS SHELL COMPANY REPORT __________ COMMISSION FILE NO. 000-30902 ____________________________________________________ Compugen Ltd. (Exact name of registrant as specified in its charter and translation of registrant's name into English) ___________________________________________________________________ Israel (Jurisdiction of incorporation or organization) Azrieli Center, 26 Harokmim Street, Building D, Holon 5885849 Israel (Address of principal executive offices) ________________________________________________ Ari Krashin, Chief Financial Officer Phone: +972-3-765-8585, Fax: +972-3-765-8555 Azrieli Center, 26 Harokmim Street, Building D, Holon 5885849 Israel (Name, Telephone, E-mail and/or Facsimile number and Address of Company Contact Person) ________________________________________________ Securities registered or to be registered pursuant to Section 12(b) of the Act: Title of each class Name of each exchange on which registered Ordinary shares, par value NIS 0.01 per share The NASDAQ Stock Market LLC (The NASDAQ Global Market) Securities registered or to be registered pursuant to Section 12(g) of the Act: None (Title of Class) Securities for which there is a reporting obligation pursuant to Section 15(d) of the Act: None Indicate the number of outstanding shares of each of the issuer's classes of capital or common stock as of the close of the period covered by the annual report: 51,293,070 Ordinary Shares Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. -

Steady Course Or Changing Tides? 2015 Trial Starts 2016 Clinical Trials Roundup – Steady Course Or Changing Tides?
2016 Clinical Trials Roundup Steady course or changing tides? 2015 Trial Starts 2016 Clinical Trials Roundup – Steady course or changing tides? Welcome to this year’s roundup where we’ll review clinical trials that initiated in 2015 to elucidate any ongoing, or new, trends within the world of pharma R&D. Here we’ll provide a high-level overview of trial activity, focused on the six major therapeutic areas (TAs) of autoimmune/inflammation, cardiovascular, CNS, infectious disease, metabolic/endocrinology, and oncology, with metrics by TA, trial phase, and disease. We’ll then zoom in on the most active industry sponsors, including a closer look at how they may (or may not be) maximizing their assets. Now, let’s take a look at the new clinical research from 2015, and see how the course of pharma R&D fared. Doro Shin, MPH Principal Analyst, Infectious & Genitourinary Diseases Manager, Thought Leadership Program 2 April 2016 © Informa UK Ltd 2016 (Unauthorized photocopying prohibited.) Rounding up the 2015 debuts Similar to years past, this annual roundup will hone in on unapproved drug3 clinical research, which comprised Approximately 4,900 Phase I-III trials started in 2015 2,769 of trials starting in 2015 (57%). Involvement across the six TAs.1 Industry sponsors2 were involved from the industry is increased as 77% of trials initiated in the majority of these trials (2934 of 4895 trials, in 2015 with an unapproved drug is linked to an 60%), particularly in autoimmune research (487 of industry sponsor (2143 of 2769 trials). Again, 668 trials, 73%). Oncology had the lowest rate and autoimmune has the largest industry participation (383 just over half of cancer trials included an industry of 424 trials, 90%) while oncology has the lowest (750 sponsor (1110 of 2080 trials). -

Supergen, Inc. Changes Name to Astex Pharmaceuticals, Inc., Announces New Stock Ticker Symbol and New Website
SuperGen, Inc. Changes Name to Astex Pharmaceuticals, Inc., Announces New Stock Ticker Symbol and New Website DUBLIN, Calif.--(BUSINESS WIRE)-- SuperGen, Inc. (NASDAQ:ASTX) announced that it has officially begun operating under the name Astex Pharmaceuticals, Inc. Concurrent with this new name, and effective at the start of trading today, September 12, 2011, the ticker symbol for the Company's common stock listed on NASDAQ has changed from "SUPG" to "ASTX." Astex Pharmaceuticals also announced the launch of its new website, www.astx.com. The website features the newly launched corporate branding, and contains information on the company's vision, pipeline and strategic partnerships. "We are extremely pleased to embark on a new era in our company's history," said James S.J. Manuso, Ph.D., chairman and chief executive officer of Astex Pharmaceuticals. "We now have the resources and capabilities in place to establish Astex Pharmaceuticals as a financially strong global leader with the aim of delivering novel cancer therapeutics targeting critical medical needs." Headquartered in Dublin, California, Astex Pharmaceuticals is dedicated to becoming a leader in the discovery, development and commercialization of a new generation of small molecule drugs, with a focus on cancer. With unrestricted cash, cash equivalents and current and non-current marketable securities of nearly $129 million as of June 30, 2011, the company plans to leverage its royalty revenue stream from Dacogen® (decitabine) for Injection, marketed in North America by Eisai and in the rest of the world by Cilag GmbH International, a wholly-owned subsidiary of Johnson & Johnson. The Company's clinical pipeline includes eight drugs in development, four of which are currently in or entering into Phase II clinical trials, and four of which are currently partnered or optioned to large pharmaceutical companies. -

Understanding Life Science Partnership Structures
MARCH 2009 MEMBER BRIEFING LIFE SCIENCES PRACTICE GROUP Understanding Life Science Partnership Structures Krist Werling, Esquire Bart Walker, Esquire Jessica Smith, Esquire McGuireWoods LLP Chicago, IL, and Charlotte, NC Companies in every industry that have attempted to raise capital and make research and development (R&D) investments over the past twelve months have faced significant challenges. The pharmaceutical and biotechnology sectors are no exception. The Dow Jones U.S. Biotechnology Index was down 18% during 2008, the pharmaceutical index DRG.X lost 19% of its market value. The entire healthcare industry has been battered during this downturn; the medical supply index DJUSAM was down 35% in 2008; managed care companies are down nearly 60%.1 While a significant wave of consolidation is coming (as evidenced by Pfizer’s announced acquisition of Wyeth), the partnership options described in this article offer options for pharmaceutical and device companies in these challenging economic times. Dramatic declines in the capital markets have been in part caused by, and accompanied by the credit crunch. This restriction in available capital has brought significant challenges to transactions in all industries, including healthcare and biotechnology. The Biotechnology Industry Organization, a prominent trade group, recently stated that 180 publicly traded biotech companies have less than one year of cash on hand.2 Both venture capital firms and private equity funds have been unable to structure leveraged buyouts and 1 Lawrence C. Strauss, Health-Care Stocks for an Ailing Economy, BARRON’S, Nov. 24, 2008. 2 Ron Winslow, Investor Prospects Look Grim, WALL ST. J., Jan. 11, 2009. 1 combination transactions requiring significant amounts of debt. -

2019 Best of ASCO Planning Committee All Relationships Are Considered Compensated
2019 Best of ASCO Planning Committee All relationships are considered compensated. Relationships are self-held unless otherwise noted. I = Immediate Family Member, Inst = My Institution Name Employment Leadership Stock and Other Honoraria Consulting or Advisory Role Speakers' Research Funding Patents, Royalties, Other Expert Travel, Accommodations, Other Ownership Bureau Intellectual Property Testimony Expenses Relationship Interests Monica M. Bertagnolli Leap Syntalogic, Syntimmune Abbvie (Inst), Agenus (Inst), Astellas Pharma (Inst), AstraZeneca (Inst), Baxalta (Inst), Therapeutics Bayer Health (Inst), Breast Cancer Research Foundation (Inst), Bristol-Myers Squibb (Inst), Celgene (Inst), Complion (Inst), Eisai (Inst), Exelixis (Inst), Genentech (Inst), GHI Pharma (Inst), Gilead Sciences (Inst), GlaxoSmithKline (Inst), Incyte (Inst), Janssen (Inst), Jazz Pharmaceuticals (Inst), Leidos (Inst), Lexicon (Inst), Lilly (Inst), Matrex (Inst), Mayo Clinic (Inst), Merck (Inst), MGH (Inst), Millenium Pharamceuticals (Inst), Novartis (Inst), Patient Centered Outcomes Research Institute (PCORI) (Inst), Pfizer (Inst), Pharmacyclics (Inst), Robert Wood Johnson Foundation (Inst), Sagerock Advisors (Inst), Sanofi (Inst), Taiho Pharmaceutical (Inst), Takeda (Inst), Tesaro (Inst), Teva (Inst) Melissa L. Johnson Araxes Pharma (Inst), Astellas Pharma (I), Abbvie (Inst), Acerta Pharma (Inst), Adaptimmune (Inst), Amgen (Inst), Array BioPharma Abbvie, Astellas Pharma, AstraZeneca (Inst), BeiGene (Inst), (Inst), AstraZeneca (Inst), BeiGene (Inst), BerGenBio