Chimeric Newcastle Disease Viruses Presenting Non-Native Surface Proteins and Uses Thereof
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Novel Rhabdovirus Infecting Newly Discovered Nycteribiid Bat Flies
www.nature.com/scientificreports OPEN Kanyawara Virus: A Novel Rhabdovirus Infecting Newly Discovered Nycteribiid Bat Flies Received: 19 April 2017 Accepted: 25 May 2017 Infesting Previously Unknown Published: xx xx xxxx Pteropodid Bats in Uganda Tony L. Goldberg 1,2,3, Andrew J. Bennett1, Robert Kityo3, Jens H. Kuhn4 & Colin A. Chapman3,5 Bats are natural reservoir hosts of highly virulent pathogens such as Marburg virus, Nipah virus, and SARS coronavirus. However, little is known about the role of bat ectoparasites in transmitting and maintaining such viruses. The intricate relationship between bats and their ectoparasites suggests that ectoparasites might serve as viral vectors, but evidence to date is scant. Bat flies, in particular, are highly specialized obligate hematophagous ectoparasites that incidentally bite humans. Using next- generation sequencing, we discovered a novel ledantevirus (mononegaviral family Rhabdoviridae, genus Ledantevirus) in nycteribiid bat flies infesting pteropodid bats in western Uganda. Mitochondrial DNA analyses revealed that both the bat flies and their bat hosts belong to putative new species. The coding-complete genome of the new virus, named Kanyawara virus (KYAV), is only distantly related to that of its closest known relative, Mount Elgon bat virus, and was found at high titers in bat flies but not in blood or on mucosal surfaces of host bats. Viral genome analysis indicates unusually low CpG dinucleotide depletion in KYAV compared to other ledanteviruses and rhabdovirus groups, with KYAV displaying values similar to rhabdoviruses of arthropods. Our findings highlight the possibility of a yet- to-be-discovered diversity of potentially pathogenic viruses in bat ectoparasites. Bats (order Chiroptera) represent the second largest order of mammals after rodents (order Rodentia). -

Guide for Common Viral Diseases of Animals in Louisiana
Sampling and Testing Guide for Common Viral Diseases of Animals in Louisiana Please click on the species of interest: Cattle Deer and Small Ruminants The Louisiana Animal Swine Disease Diagnostic Horses Laboratory Dogs A service unit of the LSU School of Veterinary Medicine Adapted from Murphy, F.A., et al, Veterinary Virology, 3rd ed. Cats Academic Press, 1999. Compiled by Rob Poston Multi-species: Rabiesvirus DCN LADDL Guide for Common Viral Diseases v. B2 1 Cattle Please click on the principle system involvement Generalized viral diseases Respiratory viral diseases Enteric viral diseases Reproductive/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 2 Deer and Small Ruminants Please click on the principle system involvement Generalized viral disease Respiratory viral disease Enteric viral diseases Reproductive/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 3 Swine Please click on the principle system involvement Generalized viral diseases Respiratory viral diseases Enteric viral diseases Reproductive/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 4 Horses Please click on the principle system involvement Generalized viral diseases Neurological viral diseases Respiratory viral diseases Enteric viral diseases Abortifacient/neonatal viral diseases Viral infections affecting the skin Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. B2 5 Dogs Please click on the principle system involvement Generalized viral diseases Respiratory viral diseases Enteric viral diseases Reproductive/neonatal viral diseases Back to the Beginning DCN LADDL Guide for Common Viral Diseases v. -

Recombinant and Chimeric Viruses
Recombinant and chimeric viruses: Evaluation of risks associated with changes in tropism Ben P.H. Peeters Animal Sciences Group, Wageningen University and Research Centre, Division of Infectious Diseases, P.O. Box 65, 8200 AB Lelystad, The Netherlands. May 2005 This report represents the personal opinion of the author. The interpretation of the data presented in this report is the sole responsibility of the author and does not necessarily represent the opinion of COGEM or the Animal Sciences Group. Dit rapport is op persoonlijke titel door de auteur samengesteld. De interpretatie van de gepresenteerde gegevens komt geheel voor rekening van de auteur en representeert niet de mening van de COGEM, noch die van de Animal Sciences Group. Advisory Committee Prof. dr. R.C. Hoeben (Chairman) Leiden University Medical Centre Dr. D. van Zaane Wageningen University and Research Centre Dr. C. van Maanen Animal Health Service Drs. D. Louz Bureau Genetically Modified Organisms Ing. A.M.P van Beurden Commission on Genetic Modification Recombinant and chimeric viruses 2 INHOUDSOPGAVE RECOMBINANT AND CHIMERIC VIRUSES: EVALUATION OF RISKS ASSOCIATED WITH CHANGES IN TROPISM Executive summary............................................................................................................................... 5 Introduction............................................................................................................................................ 7 1. Genetic modification of viruses .................................................................................................9 -

Poxvirus in a Swine Farm in Italy: a Sporadic Outbreak? O
Mariano_imp:ok 20-06-2016 11:23 Pagina 219 V. Mariano et al. Large Animal Review 2015; 21: 219-220 219 Poxvirus in a swine farm in Italy: a sporadic outbreak? O V. MARIANOa, A. NARDIa, E. VERGARIa, F. CARLETTIb, L. BARBIERIc, G. CARDETId a Laboratory of Veterinary Diagnostic Disease of Grosseto, Istituto Zooprofilattico Sperimentale del Lazio e della Toscana “M. Aleandri”, Via Europa 30, Grosseto, Italy b Virology Laboratory, National Institute for Infectious Diseases, IRCCS “L. Spallanzani”, Via Portuense 292, 00149 Rome, Italy c Veterinarian freelancer, Grosseto, Italy d Laboratory of Electron Microscopy and Specialistic Virology, Biotechnology Dept., Istituto Zooprofilattico Sperimentale del Lazio e della Toscana “M. Aleandri”, Via Appia Nuova 1411, Rome, Italy SUMMARY The aim of this report is to describe the occurrence of a Swinepox virus (SWPV) outbreak in Central Italy in 2013 and the pos- sibility of its reappearance. SWPV is the only member belonging to the Suipoxvirus genus in the Poxviridae family and it re- presents the etiologic agent of a worldwide disease specific for swine with an affinity for epidermis. In Italy it has been rarely observed. In November 2013 an outbreak was registered in a biological farm of about 110 animals located in Tuscany. Skin le- sions were observed in a group of 3 months old piglets born in the farms from crossbreed animals. The disease affected 50 of the youngest animals. Diagnosis was based on clinical and pathological signs which were pustular lesions at first located mainly around the neck and the ears and in a later stage disseminated all around the body, especially concentrated in the groin and the abdomen. -

Comparison of Plant‐Adapted Rhabdovirus Protein Localization and Interactions
University of Kentucky UKnowledge University of Kentucky Doctoral Dissertations Graduate School 2011 COMPARISON OF PLANT‐ADAPTED RHABDOVIRUS PROTEIN LOCALIZATION AND INTERACTIONS Kathleen Marie Martin University of Kentucky, [email protected] Right click to open a feedback form in a new tab to let us know how this document benefits ou.y Recommended Citation Martin, Kathleen Marie, "COMPARISON OF PLANT‐ADAPTED RHABDOVIRUS PROTEIN LOCALIZATION AND INTERACTIONS" (2011). University of Kentucky Doctoral Dissertations. 172. https://uknowledge.uky.edu/gradschool_diss/172 This Dissertation is brought to you for free and open access by the Graduate School at UKnowledge. It has been accepted for inclusion in University of Kentucky Doctoral Dissertations by an authorized administrator of UKnowledge. For more information, please contact [email protected]. ABSTRACT OF DISSERTATION Kathleen Marie Martin The Graduate School University of Kentucky 2011 COMPARISON OF PLANT‐ADAPTED RHABDOVIRUS PROTEIN LOCALIZATION AND INTERACTIONS ABSTRACT OF DISSERTATION A dissertation submitted in partial fulfillment of the requirements for the Degree of Doctor of Philosophy in the College of Agriculture at the University of Kentucky By Kathleen Marie Martin Lexington, Kentucky Director: Dr. Michael M Goodin, Associate Professor of Plant Pathology Lexington, Kentucky 2011 Copyright © Kathleen Marie Martin 2011 ABSTRACT OF DISSERTATION COMPARISON OF PLANT‐ADAPTED RHABDOVIRUS PROTEIN LOCALIZATION AND INTERACTIONS Sonchus yellow net virus (SYNV), Potato yellow dwarf virus (PYDV) and Lettuce Necrotic yellows virus (LNYV) are members of the Rhabdoviridae family that infect plants. SYNV and PYDV are Nucleorhabdoviruses that replicate in the nuclei of infected cells and LNYV is a Cytorhabdovirus that replicates in the cytoplasm. LNYV and SYNV share a similar genome organization with a gene order of Nucleoprotein (N), Phosphoprotein (P), putative movement protein (Mv), Matrix protein (M), Glycoprotein (G) and Polymerase protein (L). -

Genomic Characterisation of a Novel Avipoxvirus Isolated from an Endangered Yellow-Eyed Penguin (Megadyptes Antipodes)
viruses Article Genomic Characterisation of a Novel Avipoxvirus Isolated from an Endangered Yellow-Eyed Penguin (Megadyptes antipodes) Subir Sarker 1,* , Ajani Athukorala 1, Timothy R. Bowden 2,† and David B. Boyle 2 1 Department of Physiology, Anatomy and Microbiology, School of Life Sciences, La Trobe University, Melbourne, VIC 3086, Australia; [email protected] 2 CSIRO Livestock Industries, Australian Animal Health Laboratory, Geelong, VIC 3220, Australia; [email protected] (T.R.B.); [email protected] (D.B.B.) * Correspondence: [email protected]; Tel.: +61-3-9479-2317; Fax: +61-3-9479-1222 † Present address: CSIRO Australian Animal Health Laboratory, Australian Centre for Disease Preparedness, Geelong, VIC 3220, Australia. Abstract: Emerging viral diseases have become a significant concern due to their potential con- sequences for animal and environmental health. Over the past few decades, it has become clear that viruses emerging in wildlife may pose a major threat to vulnerable or endangered species. Diphtheritic stomatitis, likely to be caused by an avipoxvirus, has been recognised as a signifi- cant cause of mortality for the endangered yellow-eyed penguin (Megadyptes antipodes) in New Zealand. However, the avipoxvirus that infects yellow-eyed penguins has remained uncharacterised. Here, we report the complete genome of a novel avipoxvirus, penguinpox virus 2 (PEPV2), which was derived from a virus isolate obtained from a skin lesion of a yellow-eyed penguin. The PEPV2 genome is 349.8 kbp in length and contains 327 predicted genes; five of these genes were found to be unique, while a further two genes were absent compared to shearwaterpox virus 2 (SWPV2). -

25 May 7, 2014
Joint Pathology Center Veterinary Pathology Services Wednesday Slide Conference 2013-2014 Conference 25 May 7, 2014 ______________________________________________________________________________ CASE I: 3121206023 (JPC 4035610). Signalment: 5-week-old mixed breed piglet, (Sus domesticus). History: Two piglets from the faculty farm were found dead, and another piglet was weak and ataxic and, therefore, euthanized. Gross Pathology: The submitted piglet was in good body condition. It was icteric and had a diffusely pale liver. Additionally, petechial hemorrhages were found on the kidneys, and some fibrin was present covering the abdominal organs. Laboratory Results: The intestine was PCR positive for porcine circovirus (>9170000). Histopathologic Description: Mesenteric lymph node: Diffusely, there is severe lymphoid depletion with scattered karyorrhectic debris (necrosis). Also scattered throughout the section are large numbers of macrophages and eosinophils. The macrophages often contain botryoid basophilic glassy intracytoplasmic inclusion bodies. In fewer macrophages, intranuclear basophilic inclusions can be found. Liver: There is massive loss of hepatocytes, leaving disrupted liver lobules and dilated sinusoids engorged with erythrocytes. The remaining hepatocytes show severe swelling, with micro- and macrovesiculation of the cytoplasm and karyomegaly. Some swollen hepatocytes have basophilic intranuclear, irregular inclusions (degeneration). Throughout all parts of the liver there are scattered moderate to large numbers of macrophages (without inclusions). Within portal areas there is multifocally mild to moderate fibrosis and bile duct hyperplasia. Some bile duct epithelial cells show degeneration and necrosis, and there is infiltration of neutrophils within the lumen. The limiting plate is often obscured mainly by infiltrating macrophages and eosinophils, and fewer neutrophils, extending into the adjacent parenchyma. Scattered are small areas with extra medullary hematopoiesis. -

4 Introduction
4 Introduction In 1967, in Marburg an der Lahn and Frankfurt ‘subtypes’ of a novel agent named ‘Ebola virus’ am Main, Germany1, and in Belgrade, Yugoslavia after the small Ebola river in Zaire [412, 1000, (now Serbia), laboratory workers accepted shipments 2410]. Today these ‘subtypes’ are called Sudan of African green monkeys (Chlorocebus aethiops) ebolavirus (SEBOV) and Zaire ebolavirus (ZEBOV), from Uganda. As they had done many times before respectively [805]. Studies of periodic hemorrhagic with such animals, workers performed routine ex- fever outbreaks in African countries and in the aminations for apparent ailments and then prepared Philippines indicated that at least two more ebola- tissue cultures from the monkeys’ kidneys for the viruses exist, which are now known as the Coote^ development of poliomyelitis vaccines. A few days d’Ivoire ebolavirus (CIEBOV) and Reston ebola- later, several workers were reported ill and were virus (REBOV) [805]. Molecular and other studies admitted to local hospitals. A total of 32 people revealed the close relationship of MARV and the fell sick with an apparently new disease, of which ebolaviruses, which resulted in their classification seven died. A hitherto unknown virus was isolated in the same viral family, Filoviridae (the filo- from patients and human tissues [2396] and called viruses2) [805]. ‘Marburg virus’ (today Lake Victoria marburgvirus, A substantial interest in filoviruses has developed MARV) [805]. Over the subsequent three decades, among the general public, in part because of novels, only individual MARV infections were recorded. popular science stories, and Hollywood productions In 1998, the virus reappeared in the Democratic that portrayed the horrendous diseases they cause. -
Complete Sections As Applicable
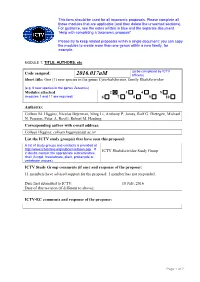
This form should be used for all taxonomic proposals. Please complete all those modules that are applicable (and then delete the unwanted sections). For guidance, see the notes written in blue and the separate document “Help with completing a taxonomic proposal” Please try to keep related proposals within a single document; you can copy the modules to create more than one genus within a new family, for example. MODULE 1: TITLE, AUTHORS, etc (to be completed by ICTV Code assigned: 2016.017aM officers) Short title: One (1) new species in the genus Cytorhabdovirus, family Rhabdoviridae (e.g. 6 new species in the genus Zetavirus) Modules attached 2 3 4 5 (modules 1 and 11 are required) 6 7 8 9 10 Author(s): Colleen M. Higgins, Nicolas Bejerman, Ming Li, Anthony P. James, Ralf G. Dietzgen, Michael N. Pearson, Peter A. Revill, Robert M. Harding Corresponding author with e-mail address: Colleen Higgins; [email protected] List the ICTV study group(s) that have seen this proposal: A list of study groups and contacts is provided at http://www.ictvonline.org/subcommittees.asp . If ICTV Rhabdoviridae Study Group in doubt, contact the appropriate subcommittee chair (fungal, invertebrate, plant, prokaryote or vertebrate viruses) ICTV Study Group comments (if any) and response of the proposer: 11 members have advised support for the proposal; 1 member has not responded. Date first submitted to ICTV: 18 July, 2016 Date of this revision (if different to above): ICTV-EC comments and response of the proposer: Page 1 of 7 MODULE 2: NEW SPECIES creating and naming one or more new species. -

Diversity and Evolution of Novel Invertebrate DNA Viruses Revealed by Meta-Transcriptomics
viruses Article Diversity and Evolution of Novel Invertebrate DNA Viruses Revealed by Meta-Transcriptomics Ashleigh F. Porter 1, Mang Shi 1, John-Sebastian Eden 1,2 , Yong-Zhen Zhang 3,4 and Edward C. Holmes 1,3,* 1 Marie Bashir Institute for Infectious Diseases and Biosecurity, Charles Perkins Centre, School of Life & Environmental Sciences and Sydney Medical School, The University of Sydney, Sydney, NSW 2006, Australia; [email protected] (A.F.P.); [email protected] (M.S.); [email protected] (J.-S.E.) 2 Centre for Virus Research, Westmead Institute for Medical Research, Westmead, NSW 2145, Australia 3 Shanghai Public Health Clinical Center and School of Public Health, Fudan University, Shanghai 201500, China; [email protected] 4 Department of Zoonosis, National Institute for Communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Changping, Beijing 102206, China * Correspondence: [email protected]; Tel.: +61-2-9351-5591 Received: 17 October 2019; Accepted: 23 November 2019; Published: 25 November 2019 Abstract: DNA viruses comprise a wide array of genome structures and infect diverse host species. To date, most studies of DNA viruses have focused on those with the strongest disease associations. Accordingly, there has been a marked lack of sampling of DNA viruses from invertebrates. Bulk RNA sequencing has resulted in the discovery of a myriad of novel RNA viruses, and herein we used this methodology to identify actively transcribing DNA viruses in meta-transcriptomic libraries of diverse invertebrate species. Our analysis revealed high levels of phylogenetic diversity in DNA viruses, including 13 species from the Parvoviridae, Circoviridae, and Genomoviridae families of single-stranded DNA virus families, and six double-stranded DNA virus species from the Nudiviridae, Polyomaviridae, and Herpesviridae, for which few invertebrate viruses have been identified to date. -

Diversity of Large DNA Viruses of Invertebrates ⇑ Trevor Williams A, Max Bergoin B, Monique M
Journal of Invertebrate Pathology 147 (2017) 4–22 Contents lists available at ScienceDirect Journal of Invertebrate Pathology journal homepage: www.elsevier.com/locate/jip Diversity of large DNA viruses of invertebrates ⇑ Trevor Williams a, Max Bergoin b, Monique M. van Oers c, a Instituto de Ecología AC, Xalapa, Veracruz 91070, Mexico b Laboratoire de Pathologie Comparée, Faculté des Sciences, Université Montpellier, Place Eugène Bataillon, 34095 Montpellier, France c Laboratory of Virology, Wageningen University, Droevendaalsesteeg 1, 6708 PB Wageningen, The Netherlands article info abstract Article history: In this review we provide an overview of the diversity of large DNA viruses known to be pathogenic for Received 22 June 2016 invertebrates. We present their taxonomical classification and describe the evolutionary relationships Revised 3 August 2016 among various groups of invertebrate-infecting viruses. We also indicate the relationships of the Accepted 4 August 2016 invertebrate viruses to viruses infecting mammals or other vertebrates. The shared characteristics of Available online 31 August 2016 the viruses within the various families are described, including the structure of the virus particle, genome properties, and gene expression strategies. Finally, we explain the transmission and mode of infection of Keywords: the most important viruses in these families and indicate, which orders of invertebrates are susceptible to Entomopoxvirus these pathogens. Iridovirus Ó Ascovirus 2016 Elsevier Inc. All rights reserved. Nudivirus Hytrosavirus Filamentous viruses of hymenopterans Mollusk-infecting herpesviruses 1. Introduction in the cytoplasm. This group comprises viruses in the families Poxviridae (subfamily Entomopoxvirinae) and Iridoviridae. The Invertebrate DNA viruses span several virus families, some of viruses in the family Ascoviridae are also discussed as part of which also include members that infect vertebrates, whereas other this group as their replication starts in the nucleus, which families are restricted to invertebrates. -

A Scoping Review of Viral Diseases in African Ungulates
veterinary sciences Review A Scoping Review of Viral Diseases in African Ungulates Hendrik Swanepoel 1,2, Jan Crafford 1 and Melvyn Quan 1,* 1 Vectors and Vector-Borne Diseases Research Programme, Department of Veterinary Tropical Disease, Faculty of Veterinary Science, University of Pretoria, Pretoria 0110, South Africa; [email protected] (H.S.); [email protected] (J.C.) 2 Department of Biomedical Sciences, Institute of Tropical Medicine, 2000 Antwerp, Belgium * Correspondence: [email protected]; Tel.: +27-12-529-8142 Abstract: (1) Background: Viral diseases are important as they can cause significant clinical disease in both wild and domestic animals, as well as in humans. They also make up a large proportion of emerging infectious diseases. (2) Methods: A scoping review of peer-reviewed publications was performed and based on the guidelines set out in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews. (3) Results: The final set of publications consisted of 145 publications. Thirty-two viruses were identified in the publications and 50 African ungulates were reported/diagnosed with viral infections. Eighteen countries had viruses diagnosed in wild ungulates reported in the literature. (4) Conclusions: A comprehensive review identified several areas where little information was available and recommendations were made. It is recommended that governments and research institutions offer more funding to investigate and report viral diseases of greater clinical and zoonotic significance. A further recommendation is for appropriate One Health approaches to be adopted for investigating, controlling, managing and preventing diseases. Diseases which may threaten the conservation of certain wildlife species also require focused attention.