Hump-Nosed Viper Bite
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Article (Published Version)
Article Identifying the snake: First scoping review on practices of communities and healthcare providers confronted with snakebite across the world BOLON, Isabelle, et al. Abstract Background Snakebite envenoming is a major global health problem that kills or disables half a million people in the world’s poorest countries. Biting snake identification is key to understanding snakebite eco-epidemiology and optimizing its clinical management. The role of snakebite victims and healthcare providers in biting snake identification has not been studied globally. Objective This scoping review aims to identify and characterize the practices in biting snake identification across the globe. Methods Epidemiological studies of snakebite in humans that provide information on biting snake identification were systematically searched in Web of Science and Pubmed from inception to 2nd February 2019. This search was further extended by snowball search, hand searching literature reviews, and using Google Scholar. Two independent reviewers screened publications and charted the data. Results We analysed 150 publications reporting 33,827 snakebite cases across 35 countries. On average 70% of victims/bystanders spotted the snake responsible for the bite and 38% captured/killed it and brought it to the healthcare facility. [...] Reference BOLON, Isabelle, et al. Identifying the snake: First scoping review on practices of communities and healthcare providers confronted with snakebite across the world. PLOS ONE, 2020, vol. 15, no. 3, p. e0229989 PMID : 32134964 DOI : 10.1371/journal.pone.0229989 Available at: http://archive-ouverte.unige.ch/unige:132992 Disclaimer: layout of this document may differ from the published version. 1 / 1 PLOS ONE RESEARCH ARTICLE Identifying the snake: First scoping review on practices of communities and healthcare providers confronted with snakebite across the world 1 1 1 1,2 Isabelle BolonID *, Andrew M. -

A Phylogeny and Revised Classification of Squamata, Including 4161 Species of Lizards and Snakes
BMC Evolutionary Biology This Provisional PDF corresponds to the article as it appeared upon acceptance. Fully formatted PDF and full text (HTML) versions will be made available soon. A phylogeny and revised classification of Squamata, including 4161 species of lizards and snakes BMC Evolutionary Biology 2013, 13:93 doi:10.1186/1471-2148-13-93 Robert Alexander Pyron ([email protected]) Frank T Burbrink ([email protected]) John J Wiens ([email protected]) ISSN 1471-2148 Article type Research article Submission date 30 January 2013 Acceptance date 19 March 2013 Publication date 29 April 2013 Article URL http://www.biomedcentral.com/1471-2148/13/93 Like all articles in BMC journals, this peer-reviewed article can be downloaded, printed and distributed freely for any purposes (see copyright notice below). Articles in BMC journals are listed in PubMed and archived at PubMed Central. For information about publishing your research in BMC journals or any BioMed Central journal, go to http://www.biomedcentral.com/info/authors/ © 2013 Pyron et al. This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. A phylogeny and revised classification of Squamata, including 4161 species of lizards and snakes Robert Alexander Pyron 1* * Corresponding author Email: [email protected] Frank T Burbrink 2,3 Email: [email protected] John J Wiens 4 Email: [email protected] 1 Department of Biological Sciences, The George Washington University, 2023 G St. -

Tan Choo Hock Thesis Submitted in Fulfi
TOXINOLOGICAL CHARACTERIZATIONS OF THE VENOM OF HUMP-NOSED PIT VIPER (HYPNALE HYPNALE) TAN CHOO HOCK THESIS SUBMITTED IN FULFILMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY FACULTY OF MEDICINE UNIVERSITY OF MALAYA KUALA LUMPUR 2013 Abstract Hump-nosed pit viper (Hypnale hypnale) is a medically important snake in Sri Lanka and Western Ghats of India. Envenomation by this snake still lacks effective antivenom clinically. The species is also often misidentified, resulting in inappropriate treatment. The median lethal dose (LD50) of H. hypnale venom varies from 0.9 µg/g intravenously to 13.7 µg/g intramuscularly in mice. The venom shows procoagulant, hemorrhagic, necrotic, and various enzymatic activities including those of proteases, phospholipases A2 and L-amino acid oxidases which have been partially purified. The monovalent Malayan pit viper antivenom and Hemato polyvalent antivenom (HPA) from Thailand effectively cross-neutralized the venom’s lethality in vitro (median effective dose, ED50 = 0.89 and 1.52 mg venom/mL antivenom, respectively) and in vivo in mice, besides the procoagulant, hemorrhagic and necrotic effects. HPA also prevented acute kidney injury in mice following experimental envenomation. Therefore, HPA may be beneficial in the treatment of H. hypnale envenomation. H. hypnale-specific antiserum and IgG, produced from immunization in rabbits, effectively neutralized the venom’s lethality and various toxicities, indicating the feasibility to produce an effective specific antivenom with a common immunization regime. On indirect ELISA, the IgG cross-reacted extensively with Asiatic crotalid venoms, particularly that of Calloselasma rhodostoma (73.6%), suggesting that the two phylogenically related snakes share similar venoms antigenic properties. -

Zootaxa, a Taxonomic Revision of the South Asian Hump
Zootaxa 2232: 1–28 (2009) ISSN 1175-5326 (print edition) www.mapress.com/zootaxa/ Article ZOOTAXA Copyright © 2009 · Magnolia Press ISSN 1175-5334 (online edition) A taxonomic revision of the South Asian hump-nosed pit vipers (Squamata: Viperidae: Hypnale) KALANA MADUWAGE1,2, ANJANA SILVA2,3, KELUM MANAMENDRA-ARACHCHI2 & ROHAN PETHIYAGODA2,4 1Faculty of Medicine, University of Peradeniya, Peradeniya, Sri Lanka 2Wildlife Heritage Trust, P.O. Box 66, Mt Lavinia, Sri Lanka 3Faculty of Medicine and Allied Sciences, Rajarata University, Saliyapura, Anuradhapura, Sri Lanka 4Corresponding author. E-mail: [email protected] Abstract The hump-nosed pit vipers of the genus Hypnale are of substantial medical importance in Sri Lanka and India, being included among the five snakes most frequently associated with life-threatening envenoming in humans. The genus has hitherto been considered to comprise three species: H. hypnale, common to Sri Lanka and the Western Ghats of peninsular India; and H. nepa and H. walli, both of which are endemic to Sri Lanka. The latter two species have frequently been confused in the literature. Here, through a review of all extant name-bearing types in the genus, supplemented by examination of preserved specimens, we show that H. nepa is restricted to the higher elevations of Sri Lanka’s central mountains; that H. walli is a junior synonym of H. nepa; and that the endemic species widely distributed in the island’s south-western ‘wet-zone’ lowlands is H. zara. We also draw attention to a possibly new species known only from a single specimen collected near Galle in southern Sri Lanka. -

Hump-Nosed Pit Vipers and Their Bites in Sri Lanka
Hump-nosed pit vipers and their bites in Sri Lanka Hypnale hypnale (Merrem, 1820), H. nepa (Laurenti, 1768) and H. zara (Gray, 1849) Kolitha H. Sellahewa Introduction The hump-nosed pit viper (Hypnale hypnale, Merrem’s pit viper) is a snake widely distributed in Sri Lanka and the South Western coastal region of India. It is the commonest snake responsible for venomous snakebite in Sri Lanka, estimated to be between 22 to 77% of all snakebites (de Silva, 1981; Seneviratne, 2000). For centuries it was considered to be a relatively innocuous snake till in 1821, for the first time, swelling and bleeding due to bites by H. hypnale was reported in animals (Davy, 1821). Since then, apart from a few isolated case reports of renal injury and death, very little was published about the clinical features following its bites and the morbidity and mortality that resulted. H. hypnale, Merrem’s pit viper, was the species recognised to cause morbidity. However, clear detailed information about other species of hump-nosed vipers, and their clinical, toxinological and biological properties were not well studied nor documented till the turn of the twentieth century. Thereafter, many accurately documented papers about hump-nosed viper envenoming have appeared in the published literature. The hump-nosed viper is widely distributed in all the peneplanes of the country and is commonly found in coconut, rubber and tea plantations. Three species of hump-nosed vipers of the genus Hypnale are found in Sri Lanka. H. hypnale is widely distributed except in Jaffna. H. nepa is confined to the central hills and H. -

Presumptive Thrombotic Thrombocytopenic Purpura
Withana et al. Journal of Venomous Animals and Toxins including Tropical Diseases 2014, 20:26 http://www.jvat.org/content/20/1/26 CASE REPORT Open Access Presumptive thrombotic thrombocytopenic purpura following a hump-nosed viper (Hypnale hypnale) bite: a case report Milinda Withana1, Chaturaka Rodrigo2*, Ariaranee Gnanathasan2 and Lallindra Gooneratne3 Abstract Hump-nosed viper bites are frequent in southern India and Sri Lanka. However, the published literature on this snakebite is limited and its venom composition is not well characterized. In this case, we report a patient with thrombotic thrombocytopenic purpura-like syndrome following envenoming which, to the best of our knowledge, has not been reported in the literature before. A 55-year-old woman from southern Sri Lanka presented to the local hospital 12 hours after a hump-nosed viper (Hypnale hypnale) bite. Five days later, she developed a syndrome that was characteristic of thrombotic thrombocytopenic purpura with fever, thrombocytopenia, microangiopathic hemolysis, renal impairment and neurological dysfunction in the form of confusion and coma. Her clinical syndrome and relevant laboratory parameters improved after she was treated with therapeutic plasma exchange. We compared our observations on this patient with the current literature and concluded that thrombotic thrombocytopenic purpura is a theoretically plausible yet unreported manifestation of hump-nosed viper bite up to this moment. This study also provides an important message for clinicians to look out for this complication in hump-nosed viper bites since timely treatment can be lifesaving. Keywords: Thrombotic thrombocytopenic purpura, Hump-nosed viper, Thrombotic microangiopathy, Snakebite, Hemolytic uremic syndrome Background Since TTP has high mortality without prompt recogni- Hump-nosed vipers of the genus Hypnale have three tion and treatment, awareness about this potential com- species Hypnale hypnale (Figure 1), Hypnale nepa and plication associated with hump-nosed viper envenoming Hypnale zara [1]. -

2018 Sri Lanka Herps & Birds-Species List
Species List SRI LANKA - SEPTEMBER 2018 Leader: James Adams BIRDS Common Name Species Name Lesser Whistling Duck Dendrocygna javanica GALLIFORMES Phasianidae Grey Francolin Francolinus pondicerianus Sri Lanka Junglefowl Gallus lafayettii Indian Peafowl Pavo cristatus CICONIIFORMES Ciconiidae Painted Stork Mycteria leucocephala Asian Openbill Anastomus oscitans Woolly-necked Stork Ciconia episcopus Lesser Adjutant Leptoptilos javanicus PELECANIFORMES Threskiornithidae Black-headed Ibis Threskiornis melanocephalus Eurasian Spoonbill Platalea leucorodia PELECANIFORMES Ardeidae Black-crowned Night Heron Nycticorax nycticorax Striated Heron Butorides striata Indian Pond Heron Ardeola grayii Eastern Cattle Egret Bubulcus coromandus Grey Heron Ardea cinerea Purple Heron Ardea purpurea Great Egret Ardea alba Intermediate Egret Ardea intermedia Little Egret Egretta garzetta PELECANIFORMES Pelecanidae Spot-billed Pelican Pelecanus philippensis SULIFORMES Phalacrocoracidae Little Cormorant Microcarbo niger Indian Cormorant Phalacrocorax fuscicollis Great Cormorant Phalacrocorax carbo SULIFORMES Anhingidae Oriental Darter Anhinga melanogaster ACCIPITRIFORMES Accipitridae Crested Honey Buzzard Pernis ptilorhynchus Crested Serpent Eagle Spilornis cheela Changeable Hawk-Eagle Nisaetus cirrhatus Black Eagle Ictinaetus malaiensis Shikra Accipiter badius Besra Accipiter virgatus Black Kite Milvus migrans Brahminy Kite Haliastur indus White-bellied Sea Eagle Haliaeetus leucogaster Grey-headed Fish Eagle Haliaeetus ichthyaetus GRUIFORMES Rallidae White-breasted -

The Sri Lanka Medical Association Book Of
THE SRI LANKA MEDICAL ASSOCIATION 133rd Anniversary International Medical Congress BOOK OF ABSTRACTS “Professional Development for Quality Enhancement of Healthcare: Beyond the COVID-19 Pandemic” 24th – 26th July 2020 Sri Lanka Medical Association 133rd Anniversary International Medical Congress Oral Presentations List of Presentations Page 04-08 Abstracts Page 09-35 Poster Presentations List of Presentations Page 38-46 Abstracts Page 47-97 Sri Lanka Medical Association 133rd Anniversary International Medical Congress, 2020 ORAL PRESENTATIONS 3 ORAL PRESENTATIONS Sri Lanka Medical Association 133rd Anniversary International Medical Congress, 2020 LIST OF ORAL PRESENTATIONS OP 01 Practice and Socio-Demographic Determinants of Diabetes Self-Care among Patients with Type 2 Diabetes Mellitus Fernando SSW, Danansuriya MN OP 02 A Retrospective Comparative Study on the Outcomes of a Low Dose and High Dose Cyclophosphamide Regimen in the Management of Class III and IV Lupus Nephritis in Sri Lanka Wijayaratne DR, Atukorala I, Gunawardena NS, Wijesundara DA, Gunarathna K, Lanerolle RD OP 03 Clinico-Epidemiology of Hypnale zara (Hump-Nosed Viper) Envenoming in Sri Lanka Rathnayaka RMMKN, Ranathunga PEAN, Kularatne SAM OP 04 Use of Antibiotics among Office Workers in a Private Company Saneeja MAF, Sampath RW, Sampath PKI, Alagiyawanna D OP 05 EEG Patterns during Mindfulness Meditation Marasinghe MGCP, Tennakoon V, Mahawithanage STC OP 06 Efficacy and Safety of Oral Hydroxyurea in Patients with Transfusion Dependent β Thalassaemia: a Randomized Double-Blind -
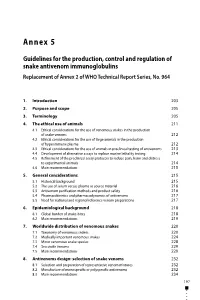
Guidelines for the Production, Control and Regulation of Snake Antivenom Immunoglobulins Replacement of Annex 2 of WHO Technical Report Series, No
Annex 5 Guidelines for the production, control and regulation of snake antivenom immunoglobulins Replacement of Annex 2 of WHO Technical Report Series, No. 964 1. Introduction 203 2. Purpose and scope 205 3. Terminology 205 4. The ethical use of animals 211 4.1 Ethical considerations for the use of venomous snakes in the production of snake venoms 212 4.2 Ethical considerations for the use of large animals in the production of hyperimmune plasma 212 4.3 Ethical considerations for the use of animals in preclinical testing of antivenoms 213 4.4 Development of alternative assays to replace murine lethality testing 214 4.5 Refinement of the preclinical assay protocols to reduce pain, harm and distress to experimental animals 214 4.6 Main recommendations 215 5. General considerations 215 5.1 Historical background 215 5.2 The use of serum versus plasma as source material 216 5.3 Antivenom purification methods and product safety 216 5.4 Pharmacokinetics and pharmacodynamics of antivenoms 217 5.5 Need for national and regional reference venom preparations 217 6. Epidemiological background 218 6.1 Global burden of snake-bites 218 6.2 Main recommendations 219 7. Worldwide distribution of venomous snakes 220 7.1 Taxonomy of venomous snakes 220 7.2 Medically important venomous snakes 224 7.3 Minor venomous snake species 228 7.4 Sea snake venoms 229 7.5 Main recommendations 229 8. Antivenoms design: selection of snake venoms 232 8.1 Selection and preparation of representative venom mixtures 232 8.2 Manufacture of monospecific or polyspecific antivenoms 232 8.3 Main recommendations 234 197 WHO Expert Committee on Biological Standardization Sixty-seventh report 9. -
Table S1. Genbank Accession and Voucher Numbers for Gene Sequences Used in Maximum Likelihood Analysis
Title A new subfamily of fossorial colubroid snakes from the Western Ghats of peninsular India Authors DEEPAK, V; Ruane, S; Gower, DJ Description Orcid: 0000-0002-1725-8863 Date Submitted 2019-12-09 Table S1. GenBank accession and voucher numbers for gene sequences used in Maximum Likelihood analysis. sno Species CYTB 16s ND4 CMOS BDNF RAG1 1 Acanthophis laevis AY340138 _ AY340167 _ _ _ 2 Acanthophis praelongus EU547063 EU547161 AY340164 EU546926 _ _ 3 Achalinus meiguensis FJ424614 FJ424614 FJ424614 _ _ _ 4 Acrantophis dumerili EU403574 EU419794 _ EU403581 AY988032 AY988066 5 Acrantophis madagascariensis U69736 AY336071 _ EU403578 FJ433973 _ 6 Acrochordus arafurae _ _ HM234056 _ _ HM234062 7 Acrochordus javanicus _ AF512745 HM234055 HM234058 AY988036 HM234061 8 Acutotyphlops kunuaensis _ _ _ GU902419 _ 9 Acutotyphlops subocularis JQ910524 KF993127 _ _ GU902418 _ 10 Adelophis foxi KF258652 _ KF258635 _ KF258601 _ 11 Adelphicos quadrivirgatus GQ895853 _ _ GQ895796 _ _ 12 Afronatrix anoscopus _ _ AF420076 AF471123 EU402622 EU402832 13 Afrotyphlops punctatus _ _ _ GU902395 _ 14 Agkistrodon contortrix EU483383 AF156566 AF156577 _ EU402623 EU402833 15 Agkistrodon piscivorus EU483436 AF057278 AF156578 AF471096 JQ599004 _ 16 Ahaetulla mycterizans KX660479 KX660205 KX660604 KX660345 _ _ 17 Ahaetulla pulverulenta KC347454 KC347339 KC347512 KC347378 _ KC347416 18 Aipysurus apraefrontalis KC014380 JX423420 JX002981 KC014288 _ _ 19 Aipysurus duboisii JX423393 JX423423 JX423411 FJ587163 _ _ 20 Alsophis anomalus _ FJ666092 _ _ _ _ 21 Alsophis antillensis -
The Evolution of Coral Snake Mimicry
University of Mississippi eGrove Electronic Theses and Dissertations Graduate School 1-1-2019 The Evolution Of Coral Snake Mimicry Renan Janke Bosque Follow this and additional works at: https://egrove.olemiss.edu/etd Part of the Biology Commons Recommended Citation Janke Bosque, Renan, "The Evolution Of Coral Snake Mimicry" (2019). Electronic Theses and Dissertations. 1927. https://egrove.olemiss.edu/etd/1927 This Dissertation is brought to you for free and open access by the Graduate School at eGrove. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of eGrove. For more information, please contact [email protected]. THE EVOLUTION OF CORAL SNAKE MIMICRY A dissertation Submitted to the graduate faculty in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Biology Department The University of Mississippi by Renan Janke Bosque, B.S; M.S. December 2019 Copyright © 2019 by Renan Janke Bosque All rights reserved. ABSTRACT Scientists have regarded mimicry as one of the most amazing examples of the power of natural selection. Early observations by naturalists of the mimetic association between venomous New World coral snakes of the genus Micrurus and harmless mimics has stimulated an intense debate about the causes and consequences of mimicry that persists today. Despite its medical, evolutionary and historical importance our understanding of evolution within the genus Micrurus is negligible. My dissertation explores the evolution of mimicry within South American coral snakes and their mimics using a multi-scale framework involving macroevolutionary (Chapter I), geographic/morphological concordance (Chapters II and III), behavioral (Chapter IV), and phylogeographic (Chapter V) approaches. -
Acute Myocardial Infarction Associated with Thrombotic Microangiopathy
de Silva et al. Journal of Medical Case Reports (2017) 11:305 DOI 10.1186/s13256-017-1484-z CASEREPORT Open Access Acute myocardial infarction associated with thrombotic microangiopathy following a hump-nosed viper bite: a case report Nipun Lakshitha de Silva1, Lalindra Gooneratne2 and Eranga Wijewickrama1,3* Abstract Background: Hump-nosed viper bite is the commonest cause of venomous snakebite in Sri Lanka. Despite initially being considered a moderately venomous snake more recent reports have revealed that it could cause significant systemic envenoming leading to coagulopathy and acute kidney injury. However, myocardial infarction was not reported except for a single case, which occurred immediately after the snakebite. Case presentation: A 50-year-old previously healthy Sri Lankan woman had a hump-nosed viper bite with no evidence of systemic envenoming during initial hospital stay. Five days later she presented with bite site cellulitis with hemorrhagic blisters, acute kidney injury, and evidence of microangiopathic hemolytic anemia and thrombocytopenia with normal coagulation studies. She was managed with supportive care that included intravenously administered antibiotics, blood transfusions, and hemodialysis; both her microangiopathic hemolytic anemia and thrombocytopenia improved without any specific intervention. On day 10 she developed: a non-ST elevation myocardial infarction complicated with acute left ventricular failure evidenced by acute shortness of breath with desaturation despite adequate ultrafiltration; new onset lateral lead T inversions in electrocardiogram; raised troponin I titer; and hypokinetic segments on echocardiogram. She was managed with low molecular weight heparin and antiplatelet drugs, which were later discontinued due to upper gastrointestinal bleeding. Her hospital stay was further complicated by hospital- acquired pneumonia and deep vein thrombosis involving her ileofemoral vein.