Chromosome Syndromes Congenital Heart Defects
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dreaming in Patients with Temporal Lobe Epilepsy: a Focus on Bad Dreams and Nightmares Carmen Anderson Department of Psychology
1 Dreaming in Patients with Temporal Lobe Epilepsy: A Focus on Bad Dreams and Nightmares Carmen Anderson Department of Psychology University of Cape Town 29th October 2012 Supervisor: Prof. Mark Solms Co-supervisor: Warren King Word count: 7055 Abstract: 164 Main body: 6891 2 Abstract Nightmares and bad dreams occur more frequently in patients with temporal lobe epilepsy (TLE) than in normal individuals. This quantitative pilot study explored the relationship between seizure activity and dreaming in patients with TLE, compared to the dreams, bad dreams and nightmares of a control population. Groups were categorized by epilepsy variables (TLE and non-TLE) and gender. Patients with temporal lobe epilepsy completed self-report questionnaires concerning their epilepsy and dreaming, and this data was compared to dreaming data from the control group using ANCOVAs. The results showed that females have significantly higher scores than males on several variables, including dreams per week, bad dream distress and nightmare distress. However, no significant main effects or interactions were found for the variables bad dream frequency and nightmare frequency, which contradicts the study’s hypotheses. It is possible that this lack of differences was due to TLE patients being on antiepileptic drugs, which whilst controlling seizures, may have suppressed or eliminated the effects of bad dreams and nightmares. Keywords: temporal lobe epilepsy, dreaming, bad dreams, nightmares, gender differences. 3 Dreaming in Patients with Temporal Lobe Epilepsy: A Focus on Bad Dreams and Nightmares Nightmares and bad dreams occur more frequently in patients with temporal lobe epilepsy (TLE) than in normal individuals and in patients with generalized seizures (Silvestri & Bromfield, 2004). -

How to Recognize a Suspected Cardiac Defect in the Neonate
Neonatal Nursing Education Brief: How to Recognize a Suspected Cardiac Defect in the Neonate https://www.seattlechildrens.org/healthcare- professionals/education/continuing-medical-nursing-education/neonatal- nursing-education-briefs/ Cardiac defects are commonly seen and are the leading cause of death in the neonate. Prompt suspicion and recognition of congenital heart defects can improve outcomes. An ECHO is not needed to make a diagnosis. Cardiac defects, congenital heart defects, NICU, cardiac assessment How to Recognize a Suspected Cardiac Defect in the Neonate Purpose and Goal: CNEP # 2092 • Understand the signs of congenital heart defects in the neonate. • Learn to recognize and detect heart defects in the neonate. None of the planners, faculty or content specialists has any conflict of interest or will be presenting any off-label product use. This presentation has no commercial support or sponsorship, nor is it co-sponsored. Requirements for successful completion: • Successfully complete the post-test • Complete the evaluation form Date • December 2018 – December 2020 Learning Objectives • Describe the risk factors for congenital heart defects. • Describe the clinical features of suspected heart defects. • Identify 2 approaches for recognizing congenital heart defects. Introduction • Congenital heart defects may be seen at birth • They are the most common congenital defect • They are the leading cause of neonatal death • Many neonates present with symptoms at birth • Some may present after discharge • Early recognition of CHD -

Anemias Supportive Module 4 "Essentials of Diagnosis, Treatment and Prevention of Major Hematologic Diseases"
2016/2017 Spring Semester Anemias Supportive module 4 "Essentials of diagnosis, treatment and prevention of major hematologic diseases" LECTURE IN INTERNAL MEDICINE FOR IV COURSE STUDENTS M. Yabluchansky, L. Bogun, L. Martymianova, O. Bychkova, N. Lysenko, N. Makienko V.N. Karazin National University Medical School’ Internal Medicine Dept. Plan of the lecture • Definition • Epidemiology • Etiology • Mechanisms • Adaptation to anemia • Classification • Clinical investigation • Diagnosis • Treatment • Prognosis • Prophylaxis • Abbreviations • Diagnostic guidelines http://anemiaofchronicdisease.com/wp-content/uploads/2012/08/anemia-of-chronic-disease1.jpg Definition Anemia is a disease and/or a clinical syndrome that consist in lowered ability of the blood to carry oxygen (hypoxia) due to decrease quantity and functional capacity and/or structural disturbances of red blood cells (RBCs) or decrease hemoglobin concentration or hematocrit in the blood A severe form of anemia, in which the hematocrit is below 10%, is called the hyperanemia WHO criteria is Hb < 13 g/dL in men and Hb < 12 g/dL in women (revised criteria for patient’s with malignancy Hb < 14 g/dL in men and Hb < 12g/dL in women) Epidemiology 1 https://www.k4health.org/sites/default/files/anemia-map_updated.png Epidemiology 2 http://img.medscape.com/fullsize/migrated/editorial/conferences/2006/4839/spivak.fig1.jpg Epidemiology 3 http://www.omicsonline.org/2161-1165/images/2161-1165-2-118-g001.gif Etiology 1 (basic forms) Basic forms • Blood loss • Deficient erythropoiesis • Excessive -
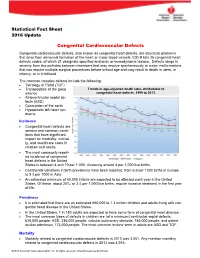
Congenital Cardiovascular Defects
Statistical Fact Sheet 2016 Update Congenital Cardiovascular Defects Congenital cardiovascular defects, also known as congenital heart defects, are structural problems that arise from abnormal formation of the heart or major blood vessels. ICD-9 lists 25 congenital heart defects codes, of which 21 designate specified anatomic or hemodynamic lesions. Defects range in severity from tiny pinholes between chambers that may resolve spontaneously to major malformations that can require multiple surgical procedures before school age and may result in death in utero, in infancy, or in childhood. The common complex defects include the following: Tetralogy of Fallot (TOF) Transposition of the great Trends in age-adjusted death rates attributable to arteries congenital heart defects, 1999 to 2013. Atrioventricular septal de- fects (ASD) Coarctation of the aorta Hypoplastic left heart syn- drome Incidence Congenital heart defects are serious and common condi- tions that have significant impact on morbidity, mortali- ty, and healthcare costs in children and adults. The most commonly report- ed incidence of congenital heart defects in the United States is between 4 and 10 per 1,000, clustering around 8 per 1,000 live births. Continental variations in birth prevalence have been reported, from 6.9 per 1000 births in Europe to 9.3 per 1000 in Asia. An estimated minimum of 40,000 infants are expected to be affected each year in the United States. Of these, about 25%, or 2.4 per 1,000 live births, require invasive treatment in the first year of life. Prevalence It is estimated that there are an estimated 650,000 to 1.3 million children and adults living with con- genital heart disease in the United States. -

Congenital Heart Disease Parent FAQ
Congenital Heart Disease Parent FAQ achd.stanfordchildrens.org | achd.stanfordhealthcare.org About Congenital Heart Disease What is congenital heart disease? Congenital heart disease, also called congenital heart defect (CHD), is a heart problem that a baby is born with. When the heart forms in the womb, it develops incorrectly and does not work properly, which changes how the blood flows through the heart. What causes congenital heart defects? In most cases, there is no clear cause. It can be linked to something out of the ordinary happening during gestation, including a viral infection or exposure to environmental factors. Or, it may be linked to a single gene defect or chromosome abnormalities. How common is CHD in the United States among children? Congenital heart defects are the most common birth defects in children in the United States. Approximately 1 in 100 babies are born with a heart defect. What are the most common types of congenital heart defects in children? In general, CHDs disrupt the flow of blood in the heart as it passes to the lungs or to the body. The most common congenital heart defects are abnormalities in the heart valves or a hole between the chambers of the heart (ventricles). Examples include ventricular septal defect (VSD), atrial septal defect (ASD), and bicuspid aortic valve. At the Betty Irene Moore Children’s Heart Center at Stanford Children’s Health, we are known across the nation and world for treating some of the most complex congenital heart defects with outstanding outcomes. Congenital Heart Disease Parent FAQ | 2 Is CHD preventable? In some cases, it could be preventable. -

Pulmonary-Atresia-Mapcas-Pavsdmapcas.Pdf
Normal Heart © 2012 The Children’s Heart Clinic NOTES: Children’s Heart Clinic, P.A., 2530 Chicago Avenue S, Ste 500, Minneapolis, MN 55404 West Metro: 612-813-8800 * East Metro: 651-220-8800 * Toll Free: 1-800-938-0301 * Fax: 612-813-8825 Children’s Minnesota, 2525 Chicago Avenue S, Minneapolis, MN 55404 West Metro: 612-813-6000 * East Metro: 651-220-6000 © 2012 The Children’s Heart Clinic Reviewed March 2019 Pulmonary Atresia, Ventricular Septal Defect and Major Aortopulmonary Collateral Arteries (PA/VSD/MAPCAs) Pulmonary atresia (PA), ventricular septal defect (VSD) and major aortopulmonary collateral arteries (MAPCAs) is a rare type of congenital heart defect, also referred to as Tetralogy of Fallot with PA/MAPCAs. Tetralogy of Fallot (TOF) is the most common cyanotic heart defect and occurs in 5-10% of all children with congenital heart disease. The classic description of TOF includes four cardiac abnormalities: overriding aorta, right ventricular hypertrophy (RVH), large perimembranous ventricular septal defect (VSD), and right ventricular outflow tract obstruction (RVOTO). About 20% of patients with TOF have PA at the infundibular or valvar level, which results in severe right ventricular outflow tract obstruction. PA means that the pulmonary valve is closed and not developed. When PA occurs, blood can not flow through the pulmonary arteries to the lungs. Instead, the child is dependent on a patent ductus arteriosus (PDA) or multiple systemic collateral vessels (MAPCAs) to deliver blood to the lungs for oxygenation. These MAPCAs usually arise from the de- scending aorta and subclavian arteries. Commonly, the pulmonary arteries are abnormal, with hypoplastic (small and underdeveloped) central and branch pulmonary arteries and/ or non-confluent central pulmonary arteries. -

Predicting Chemotherapy-Induced Febrile Neutropenia Outcomes in Adult Cancer Patients: an Evidence-Based Prognostic Model
Predicting Chemotherapy-Induced Febrile Neutropenia Outcomes in Adult Cancer Patients: An Evidence-Based Prognostic Model Yee Mei, Lee Cert Nursing (S’pore), RN, Adv. Dip. (Oncology) in Nursing (S’pore), Bsc of Nursing (Monash), Master of Nursing (S’pore) Thesis submitted for the Doctor of Philosophy School of Translational Health Science The University of Adelaide Adelaide, South Australia Australia November 2013 Table of Contents TABLE OF CONTENTS -------------------------------------------------------------------- II LIST OF TABLES ------------------------------------------------------------------------ VII LIST OF FIGURES ---------------------------------------------------------------------- VIII LIST OF ABBREVIATIONS --------------------------------------------------------------- XI ABSTRACT ----------------------------------------------------------------------------- XII DECLARATION ----------------------------------------------------------------------- XIIII ACKNOWLEDGEMENTS-- ------------------------------------------------------------ IXV PUBLICATIONS ------------------------------------------------------------------------ XV 1 INTRODUCTION TO THE THESIS ---------------------------------------------------- 15 1.1 CLINICAL CONTEXT -------------------------------------------------------------------------------- 15 1.2 CLINICAL IMPACT OF CHEMOTHERAPY-INDUCED FEBRILE NEUTROPENIA -------------------- 16 1.3 ECONOMIC IMPLICATIONS OF CHEMOTHERAPY-INDUCED FEBRILE NEUTROPENIA ---------- 18 1.4 EVOLVING PRACTICE IN THE MANAGEMENT OF FEBRILE -

Download Dr. Qureshi's CV
Brief Synopsis Nazer H. Qureshi, M.D, D.Stat, M.Sc, DABNS, FAANS. Graduated from Medical School with top honors and first position in Anatomy and Histology in board examinations. Pursued surgical training in Europe including neurosurgery at the National Center for Neurosurgery affiliated with The Royal College of Surgeons of Ireland. In 1994 started as a junior faculty member at University of Dublin teaching medical students while pursuing his own research on “Interleukin-1 binding and expression in brain” towards Masters in Science. During that year also attained a Diploma in Statistics from University of Dublin. In summer of 1995 was a visiting fellow at University of Toronto working on use- dependent inhibitory depression in epilepsy models. In 1996 migrated to US and completed a research fellowship in gene therapy for brain tumors at Harvard Medical School/Massachusetts General Hospital. The work on gene therapy that included testing efficacy and toxicity of different viral vectors and & designing a novel method of gene delivery to human brain tumors culminated into a clinical trial. In 1999 completed a neurosurgery fellowship at University of Arizona. Completed 2 years of accredited General Surgery residency at Tuft’s University and Thomas Jefferson University followed by Neurosurgery Residency in June 2008 from University of Arkansas for Medical Sciences with “Prof. Iftikhar A. Raja Humanity in Medicine Award.” Diplomate American Board of Neurological Surgeons and Fellow of the American Board of Neurological Surgeons. Worked as an attending neurosurgeon at Baptist Hospital Medical Center in Little Rock the chief of brain and spine tumor service at Baptist Health Medical Center, North Little Rock. -

Iron Deficiency Anemia (Ida) Recommendations
IRON DEFICIENCY ANEMIA (IDA) Clinical Practice Guideline | March 2018 OBJECTIVE Alberta clinicians (specifically primary care and emergency department physicians) will be able to diagnose iron deficiency anemia (IDA), treat using oral and parenteral iron supplementation and provide ongoing management; will understand why red blood cell transfusion (RBC) may be harmful and is only occasionally required for the treatment of IDA. TARGET POPULATION Patients >5 years of age, hemodynamically stable, seen in emergency departments and primary care settings EXCLUSIONS Patients <5 years of age, all patients who are hemodynamically unstable, chronic kidney disease, rare genetic causes of and treatment of IDA, other types of iron deficiency, and the pre-latent stage of iron deficiency RECOMMENDATIONS ASSESSMENT INVESTIGATION FOR IDA Identify patients at risk for iron deficiency anemia Table 1: Possible Features, Signs and Symptoms of IDA ADULTS AND ADOLESCENTS Anticipated ongoing bleeding (e.g., menstruation, gastrointestinal) Head and neck manifestations including pallor (e.g., facial, conjunctival or palmar), blue sclerae, atrophic glossitis or loss of tongue papillae, angular cheilitis, alopecia Koilonychia (spoon nails) Restless leg syndrome Fatigue, shortness of breath, chest pain, lightheaded, syncope weakness, headache Irritability and/or depression Pica (craving/consumption of non-food substances e.g., dirt, clay, chalk) and pagophagia (ice craving) Decreased exercise tolerance Regular blood donors, particularly females donating more than twice a year and males donating more than three or four times a year SCHOOL-AGED CHILDREN (e.g., >5 to <18 years old) Tiredness, restlessness, irritability Pica and pagophagia Growth retardation Cognitive and intellectual impairment Signs of attention-deficit/hyperactivity disorder (ADHD) Breath-holding spells These recommendations are systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances. -

Local Anesthetic Agents Infiltration: Role of the Nurse
Doug Ducey Joey Ridenour Governor Executive Director Arizona State Board of Nursing 1740 W Adams Street, Suite 2000 Phoenix. AZ 85007 Phone (602) 771-7800 Home Page: http://www.azbn.gov OPINION: INFILTRATION OF LOCAL An advisory opinion adopted by AZBN is an interpretation of what the law requires. While an ANESTHETIC AGENTS: THE ROLE OF THE advisory opinion is not law, it is more than a recommendation. In other words, an advisory opinion NURSE is an official opinion of AZBN regarding the practice of nursing as it relates to the functions of APPROVED DATE: 3/2015 nursing. Facility policies may restrict practice further in their setting and/or require additional REVISED DATE: 7/2018 expectations related to competency, validation, training, and supervision to assure the safety of their patient population and or decrease risk. ORIGINATING COMMITTEE: SCOPE OF PRACTICE COMMITTEE Within the Scope of Practice of X RN x LPN ADVISORY OPINION LOCAL ANESTHETIC AGENTS INFILTRATION: ROLE OF THE NURSE It is within the scope of practice of a registered nurse (RN) and a licensed practical nurse (LPN) to administer certain local anesthetic agents intradermal, subcutaneous, and submucosal for the purposes of analgesia and/or anesthesia prior to potentially painful procedures. Tumescent lidocaine infiltration for ambulatory procedures, such as but not limited to, the treatment of hyperhidrosis, ambulatory phlebectomy and laser facial resurfacings would be within the RN scope under the direction of an licensed independent practitioner (LIP) and when certain criteria is met within this advisory opinion. The licensed nurse must meet the general requirements and course of instruction listed in parts I and II. -

Transcatheter Device Closure of Atrial Septal Defect in Dextrocardia with Situs Inversus Totalis
Case Report Nepalese Heart Journal 2019; Vol 16(1), 51-53 Transcatheter device closure of atrial septal defect in dextrocardia with situs inversus totalis Kiran Prasad Acharya1, Chandra Mani Adhikari1, Aarjan Khanal2, Sachin Dhungel1, Amrit Bogati1, Manish Shrestha3, Deewakar Sharma1 1 Department of Cardiology, Shahid Gangalal National Heart Centre, Kathmandu, Nepal 2 Department of Internal Medicine, Kathmandu Medical College, Kathmandu,Nepal 3 Department of Pediatric Cardiology, Shahid Gangalal National Heart Centre, Kathmandu, Nepal Corresponding Author: Chandra Mani Adhikari Department of Cardiology Shahid Gangalal National Heart Centre Kathmandu, Nepal Email: [email protected] Cite this article as: Acharya K P, Adhikari C M, Khanal A, et al. Transcatheter device closure of atrial septal defect in dextrocardia with situs inversus totalis. Nepalese Heart Journal 2019; Vol 16(1), 51-53 Received date: 17th February 2019 Accepted date: 16th April 2019 Abstract Only few cases of Device closure of atrial septal defect in dextrocardia with situs inversus totalis has been reported previously. We present a case of a 36 years old male, who had secundum type of atrial septal defect in dextrocardia with situs inversus totalis. ASD device closure was successfully done. However, we encountered few technical difficulties in this case which are discussed in this case review. Keywords: atrial septal defect; dextrocardia; transcatheter device closure, DOI: https://doi.org/10.3126/njh.v16i1.23901 Introduction There are only two case reported of closure of secundum An atrial septal defect (ASD) is an opening in the atrial ASD associated in patients with dextrocardia and situs inversus septum, excluding a patent foramen ovale.1 ASD is a common totalis. -

Tetralogy of Fallot.” These Podcasts Are Designed to Give Medical Students an Overview of Key Topics in Pediatrics
PedsCases Podcast Scripts This is a text version of a podcast from Pedscases.com on “Tetralogy of Fallot.” These podcasts are designed to give medical students an overview of key topics in pediatrics. The audio versions are accessible on iTunes or at www.pedcases.com/podcasts. Tetralogy of Fallot Developed by Katie Girgulis, Dr. Andrew Mackie, and Dr. Karen Forbes for PedsCases.com. April 14, 2017 Introduction Hello, my name is Katie Girgulis and I am a medical student at the University of Alberta. This podcast was developed with the help of Dr. Andrew Mackie and Dr. Karen Forbes. Dr. Mackie is a pediatric cardiologist at the Stollery Children’s Hospital, and Dr. Forbes is a pediatrician and medical educator at the Stollery Children’s Hospital. This podcast is about the cardiac condition Tetralogy of Fallot (ToF). For teaching on the general approach to pediatric heart murmurs, please check out the ‘Evaluation of a Heart Murmur’ podcast on Pedscases.com. Slide 2 Learning Objectives By the end of this podcast, the learner will be able to: 1) Recognize the clinical presentations of ToF 2) Describe the four anatomical characteristics of ToF 3) Describe the pathophysiology of the murmur in ToF 4) Formulate initial steps when ToF is suspected 5) Delineate the treatment of hypercyanotic episodes 6) Summarize the definitive treatment for ToF Slide 3 Case – Baby Josh Let’s start with a clinical case: You are working with Dr. Smith, a family physician, during your family medicine rotation. Josh is a 4-month-old infant who is here for a well-baby check.