398 INDEX Sleeping Sickness 182 Viral Encephalitis 40–41 Yellow
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Detection of Leishmania Aethiopica in Paraffin-Embedded Skin Biopsies Using the Polymerase Chain Reaction T
ZOBODAT - www.zobodat.at Zoologisch-Botanische Datenbank/Zoological-Botanical Database Digitale Literatur/Digital Literature Zeitschrift/Journal: Mitteilungen der Österreichischen Gesellschaft für Tropenmedizin und Parasitologie Jahr/Year: 1994 Band/Volume: 16 Autor(en)/Author(s): Laskay T., Miko T. L., Teferedegn H., Negesse Y., Rodgers M. R., Solbach W., Röllinghoff M., Frommel D. Artikel/Article: Onchozerkose-Kontrolle in Mali - Darstellung eines Kommunikationsdefizites und seine Entwicklung. 141-146 ©Österr. Ges. f. Tropenmedizin u. Parasitologie, download unter www.biologiezentrum.at Mitt. Österr. Ges. Armauer Hansen Research Institute (AHRI), Addis Ababa, Ethiopia (Director: Dr. D. Frommel) (1) Tropenmed. Parasitol. 16 (1994) All Africa Leprosy Rehabilitation and Training Center (ALERT), Addis Ababa, Ethiopia 141 - 146 (Managing Director: Mr. J. N. Alldred) (2) Department of Tropical Public Health, Harvard School of Public Health, Boston, MA (Head of Unit: Dr. Dyann Wirth) (3) Institute for Clinical Microbiology, Univerity of Erlangen-Nürnberg, Erlangen, F. R. G. (Director: Prof. Dr. M. Röllinghoff) (4) Detection of Leishmania aethiopica in paraffin-embedded skin biopsies using the polymerase chain reaction T. Laskay14, T. L. Miko1-2, H. Teferedegn1, Y. Negesse12, M. R. Rodgers3, W. Solbach4, M. Röllinghoff4, D. Frommel1 Introduction Cutaneous leishmaniasis (CL) is a serious public health problem in several areas of the world. Current reports indicate that the prevalence of the disease is increasing in many countries (4). One major focus of CL in the Old World is found in Ethiopia where the aetiological agent is Leishmania aethiopica (1, 2, 7). At present diagnosis relies on the detection of the parasite in smears or skin biopsy specimens by histopathological examination and/or by in vitro culture. -

First Case of Furuncular Myiasis Due to Cordylobia Anthropophaga in A
braz j infect dis 2 0 1 8;2 2(1):70–73 The Brazilian Journal of INFECTIOUS DISEASES www.elsevi er.com/locate/bjid Case report First case of Furuncular Myiasis due to Cordylobia anthropophaga in a Latin American resident returning from Central African Republic a b a c a,∗ Jóse A. Suárez , Argentina Ying , Luis A. Orillac , Israel Cedeno˜ , Néstor Sosa a Gorgas Memorial Institute, City of Panama, Panama b Universidad de Panama, Departamento de Parasitología, City of Panama, Panama c Ministry of Health of Panama, International Health Regulations, Epidemiological Surveillance Points of Entry, City of Panama, Panama a r t i c l e i n f o a b s t r a c t 1 Article history: Myiasis is a temporary infection of the skin or other organs with fly larvae. The lar- Received 7 November 2017 vae develop into boil-like lesions. Creeping sensations and pain are usually described by Accepted 22 December 2017 patients. Following the maturation of the larvae, spontaneous exiting and healing is expe- Available online 2 February 2018 rienced. Herein we present a case of a traveler returning from Central African Republic. She does not recall insect bites. She never took off her clothing for recreational bathing, nor did Keywords: she visit any rural areas. The lesions appeared on unexposed skin. The specific diagnosis was performed by morphologic characterization of the larvae, resulting in Cordylobia anthro- Cordylobia anthropophaga Furuncular myiasis pophaga, the dominant form of myiasis in Africa. To our knowledge, this is the first reported Tumbu-fly case of C. -

Artrópodos Como Agentes De Enfermedad
DEPARTAMENTO DE PARASITOLOGIA Y MICOLOGIA INVERTEBRADOS, CELOMADOS, CON SEGMENTACIÓN EXTERNA, PATAS Y APÉNDICES ARTICULADOS EXOESQUELETO QUITINOSO TUBO DIGESTIVO COMPLETO, APARATO CIRCULATORIO Y EXCRETOR ABIERTO. RESPIRACIÓN TRAQUEAL EL TIPO INTEGRA LAS CLASES DE IMPORTANCIA MÉDICA COMO AGENTES: ARACHNIDA, INSECTA CHILOPODA DIOCOS, CON FRECUENTE DIMORFISMO SEXUAL CICLOS EVOLUTIVOS DE VARIABLE COMPLEJIDAD (HUEVOS, LARVAS, NINFAS, ADULTOS). INSECTA. CARACTERES GENERALES. LA CLASE INTEGRA CON IMPORTANCIA MEDICA COMO AGENTES: PARÁSITOS, MICROPREDADORES E INOCULADORES DE PONZOÑA. CUERPO DIVIDIDO EN CABEZA, TÓRAX Y ABDOMEN APARATO BUCAL DE DIFERENTE TIPO. RESPIRACIÓN TRAQUEAL TRES PARES DE PATAS PRESENCIA DE ALAS Y ANTENAS METAMORFOSIS DE COMPLEJIDAD VARIABLE ARACHNIDA. CARACTERES GENERALES. LA CLASE INTEGRA CON IMPORTANCIA MEDICA COMO AGENTES ARAÑAS, ESCORPIONES, GARRAPATAS Y ÁCAROS. CUERPO DIVIDIDO EN CEFALOTÓRAX Y ABDOMEN. DIFERENTES TIPOS DE APÉNDICES PREORALES RESPIRACIÓN TRAQUEAL EN LA MAYORÍA CUATRO PARES DE PATAS PRESENCIA DE GLÁNDULA VENENOSAS EN MUCHOS. SIN ALAS Y SIN ANTENAS AGENTE CAUSA O ETIOLOGÍA DIRECTA DE UNA AFECCIÓN. ARTRÓPODOS COMO AGENTES DE ENFERMEDAD: *ARÁCNIDOS (ÁCAROS, ARAÑAS, ESCORPIONES) *MIRIÁPODOS (CIEMPIÉS, ESCOLOPENDRAS) *INSECTOS (PIOJOS, LARVAS DE MOSCAS, ABEJAS, ETC.) TIPOS DE AGENTES NOSOLÓGICOS : - PARÁSITOS (LARVAS O ADULTOS) - MICROPREDADORES - PONZOÑOSOS - ALERGENOS DESARROLLO DE PARASITISMO: - ECTOPARÁSITOS - MIASIS INOCULACIÓN O CONTAMINACIÓN CON PONZOÑAS (TÓXICOS ELABORADOS POR SERES VIVOS). -

Human Botfly (Dermatobia Hominis)
CLOSE ENCOUNTERS WITH THE ENVIRONMENT What’s Eating You? Human Botfly (Dermatobia hominis) Maryann Mikhail, MD; Barry L. Smith, MD Case Report A 12-year-old boy presented to dermatology with boils that had not responded to antibiotic therapy. The boy had been vacationing in Belize with his family and upon return noted 2 boils on his back. His pediatrician prescribed a 1-week course of cephalexin 250 mg 4 times daily. One lesion resolved while the second grew larger and was associated with stinging pain. The patient then went to the emergency depart- ment and was given a 1-week course of dicloxacil- lin 250 mg 4 times daily. Nevertheless, the lesion persisted, prompting the patient to return to the Figure 1. Clinical presentation of a round, nontender, emergency department, at which time the dermatol- 1.0-cm, erythematous furuncular lesion with an overlying ogy service was consulted. On physical examination, 0.5-cm, yellow-red, gelatinous cap with a central pore. there was a round, nontender, 1.0-cm, erythema- tous nodule with an overlying 0.5-cm, yellow-red, gelatinous cap with a central pore (Figure 1). The patient was afebrile and had no detectable lymphad- enopathy. Management consisted of injection of lidocaine with epinephrine around and into the base of the lesion for anesthesia, followed by insertion of a 4-mm tissue punch and gentle withdrawal of a botfly (Dermatobia hominis) larva with forceps through the defect it created (Figure 2). The area was then irri- gated and bandaged without suturing and the larva was sent for histopathologic evaluation (Figure 3). -

El Parasitismo En Cunicultura (1)
EL PARASITISMO EN CUNICULTURA (1) por el Dr. José-Oriol Rovellat Se conoce por parásito a todo organismo viviente, que alojado en otro ser vivo, realiza a expensas de éste, todas sus funciones vitales, ocasionándole algún perjuicio. AI organismo que vive a expensas del otro se le Ilama PARASITO y al que le da cobijo HOSPEDADOR. Según su localización en el organismo animal los parásitos se dividen en ectoparásitos, cuando viven sobre la superficie externa del cuerpo del hospedador o en cavidades que comunican con el exterior; los endoparásitos son los parásitos que viven dentro del cuerpo de los hospedadores, localizándose en el tubo digestivo, pulmones, hígado, otras vísceras, células, tejidos y cavidades corporales. Según el tiempo que habitan en el organismo del hospedador, se dividen en dos grandes grupos: los parásitos temporales que sólo buscan al hospedador para alimentarse y luego lo abandonan, y los parásitos estacionarios que permanecen dentro del cuerpo del hospedador un tiempo definido de su desarrollo o bien de una manera permanente. Dentro de los parásitos estacionarios, según pasen más o menos tiempo en el organismo del hospedador se subdividen en: Parásitos Periódicos que permanecen una parte de su vida en el hospe- dador y luego lo abandonan para continuar un tipo de vida no parasitaria. Los Parásitos Permanentes pasan toda su vida en el organismo del hospedador. Los parásitos accidentales son los que ocasional- mente aparecen en hospedadores anormales en condiciones normales. Los Parásitos erráticos o abe- rrantes son los que emigran a unos órganos que no son atacados normalmente dentro del organismo del hospedador. -

Experimental Infection of Dogs with Toscana Virus and Sandfly
microorganisms Article Experimental Infection of Dogs with Toscana Virus and Sandfly Fever Sicilian Virus to Determine Their Potential as Possible Vertebrate Hosts Clara Muñoz 1, Nazli Ayhan 2,3 , Maria Ortuño 1, Juana Ortiz 1, Ernest A. Gould 2, Carla Maia 4, Eduardo Berriatua 1 and Remi N. Charrel 2,* 1 Departamento de Sanidad Animal, Facultad de Veterinaria, Campus de Excelencia Internacional Regional “Campus Mare Nostrum”, Universidad de Murcia, 30100 Murcia, Spain; [email protected] (C.M.); [email protected] (M.O.); [email protected] (J.O.); [email protected] (E.B.) 2 Unite des Virus Emergents (UVE: Aix Marseille Univ, IRD 190, INSERM U1207, IHU Mediterranee Infection), 13005 Marseille, France; [email protected] (N.A.); [email protected] (E.A.G.) 3 EA7310, Laboratoire de Virologie, Université de Corse-Inserm, 20250 Corte, France 4 Global Health and Tropical Medicine, GHMT, Instituto de Higiene e Medicina Tropical, IHMT, Universidade Nova de Lisboa, UNL, Rua da Junqueira, 100, 1349-008 Lisboa, Portugal; [email protected] * Correspondence: [email protected] Received: 2 April 2020; Accepted: 19 April 2020; Published: 20 April 2020 Abstract: The sandfly-borne Toscana phlebovirus (TOSV), a close relative of the sandfly fever Sicilian phlebovirus (SFSV), is one of the most common causes of acute meningitis or meningoencephalitis in humans in the Mediterranean Basin. However, most of human phlebovirus infections in endemic areas either are asymptomatic or cause mild influenza-like illness. To date, a vertebrate reservoir for sandfly-borne phleboviruses has not been identified. Dogs are a prime target for blood-feeding phlebotomines and are the primary reservoir of human sandfly-borne Leishmania infantum. -

Molecular Characterization of Leishmania RNA Virus 2 in Leishmania Major from Uzbekistan
G C A T T A C G G C A T genes Article Molecular Characterization of Leishmania RNA virus 2 in Leishmania major from Uzbekistan 1, 2,3, 1,4 2 Yuliya Kleschenko y, Danyil Grybchuk y, Nadezhda S. Matveeva , Diego H. Macedo , Evgeny N. Ponirovsky 1, Alexander N. Lukashev 1 and Vyacheslav Yurchenko 1,2,* 1 Martsinovsky Institute of Medical Parasitology, Tropical and Vector Borne Diseases, Sechenov University, 119435 Moscow, Russia; [email protected] (Y.K.); [email protected] (N.S.M.); [email protected] (E.N.P.); [email protected] (A.N.L.) 2 Life Sciences Research Centre, Faculty of Science, University of Ostrava, 71000 Ostrava, Czech Republic; [email protected] (D.G.); [email protected] (D.H.M.) 3 CEITEC—Central European Institute of Technology, Masaryk University, 62500 Brno, Czech Republic 4 Department of Molecular Biology, Faculty of Biology, Moscow State University, 119991 Moscow, Russia * Correspondence: [email protected]; Tel.: +420-597092326 These authors contributed equally to this work. y Received: 19 September 2019; Accepted: 18 October 2019; Published: 21 October 2019 Abstract: Here we report sequence and phylogenetic analysis of two new isolates of Leishmania RNA virus 2 (LRV2) found in Leishmania major isolated from human patients with cutaneous leishmaniasis in south Uzbekistan. These new virus-infected flagellates were isolated in the same region of Uzbekistan and the viral sequences differed by only nineteen SNPs, all except one being silent mutations. Therefore, we concluded that they belong to a single LRV2 species. New viruses are closely related to the LRV2-Lmj-ASKH documented in Turkmenistan in 1995, which is congruent with their shared host (L. -

A Review on Biology, Epidemiology And
iolog ter y & c P a a B r f a o s i l Journal of Bacteriology and t o Dawit et al., J Bacteriol Parasitol 2013, 4:2 a l n o r g u DOI: 10.4172/2155-9597.1000166 y o J Parasitology ISSN: 2155-9597 Research Article Open Access A Review on Biology, Epidemiology and Public Health Significance of Leishmaniasis Dawit G1, Girma Z1 and Simenew K1,2* 1College of Veterinary Medicine and Agriculture, Addis Ababa University, Debre Zeit, Ethiopia 2College of Agricultural Sciences, Dilla University, Dilla, Ethiopia Abstract Leishmaniasis is a major vector-borne disease caused by obligate intramacrophage protozoa of the genus Leishmania, and transmitted by the bite of phlebotomine female sand flies of the genera Phlebotomus and Lutzomyia, in the old and new worlds, respectively. Among 20 well-recognized Leishmania species known to infect humans, 18 have zoonotic nature, which include agents of visceral, cutaneous, and mucocutaneous forms of the disease, in both the old and new worlds. Currently, leishmaniasis show a wider geographic distribution and increased global incidence. Environmental, demographic and human behaviors contribute to the changing landscape for zoonotic cutaneous and visceral leishmaniasis. The primary reservoir hosts of Leishmania are sylvatic mammals such as forest rodents, hyraxes and wild canids, and dogs are the most important species among domesticated animals in the epidemiology of this disease. These parasites have two basic life cycle stages: one extracellular stage within the invertebrate host (phlebotomine sand fly), and one intracellular stage within a vertebrate host. Co-infection with HIV intensifies the burden of visceral and cutaneous leishmaniasis by causing severe forms and more difficult to manage. -
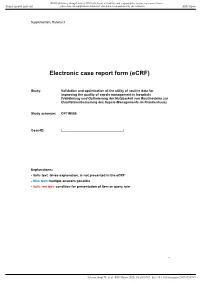
Electronic Case Report Form (Ecrf)
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open Supplementary Material 3 Electronic case report form (eCRF) Study: Validation and optimization of the utility of routine data for improving the quality of sepsis management in hospitals (Validierung und Optimierung der Nutzbarkeit von Routinedaten zur Qualitätsverbesserung des Sepsis-Managements im Krankenhaus) Study acronym: OPTIMISE Case-ID: |_________________________________| Explanations: - italic text: Gives explanation, is not presented in the eCRF - blue text: multiple answers possible - italic red text: condition for presentation of item or query rule 1 Schwarzkopf D, et al. BMJ Open 2020; 10:e035763. doi: 10.1136/bmjopen-2019-035763 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open Supplementary Material 3 A. Identification of patients with sepsis 1000 random cases per study centre need to be documented by trained study physicians 0. Admission and discharge dates a. Where several stays 0 no merged to one case for billing 1 yes reasons? If a = yes, ____ how many stays/cases have Query rule: N >= 2 been merged? b. Admission and discharge Admission date: |__|__|____ Discharge date: |__|__|____ dates Admission date: |__|__|____ Discharge date: |__|__|____ Admission date: |__|__|____ Discharge date: |__|__|____ Admission date: |__|__|____ Discharge date: |__|__|____ Query rule: discharge date after admission date c. -

INFECTIOUS DISEASES of ETHIOPIA Infectious Diseases of Ethiopia - 2011 Edition
INFECTIOUS DISEASES OF ETHIOPIA Infectious Diseases of Ethiopia - 2011 edition Infectious Diseases of Ethiopia - 2011 edition Stephen Berger, MD Copyright © 2011 by GIDEON Informatics, Inc. All rights reserved. Published by GIDEON Informatics, Inc, Los Angeles, California, USA. www.gideononline.com Cover design by GIDEON Informatics, Inc No part of this book may be reproduced or transmitted in any form or by any means without written permission from the publisher. Contact GIDEON Informatics at [email protected]. ISBN-13: 978-1-61755-068-3 ISBN-10: 1-61755-068-X Visit http://www.gideononline.com/ebooks/ for the up to date list of GIDEON ebooks. DISCLAIMER: Publisher assumes no liability to patients with respect to the actions of physicians, health care facilities and other users, and is not responsible for any injury, death or damage resulting from the use, misuse or interpretation of information obtained through this book. Therapeutic options listed are limited to published studies and reviews. Therapy should not be undertaken without a thorough assessment of the indications, contraindications and side effects of any prospective drug or intervention. Furthermore, the data for the book are largely derived from incidence and prevalence statistics whose accuracy will vary widely for individual diseases and countries. Changes in endemicity, incidence, and drugs of choice may occur. The list of drugs, infectious diseases and even country names will vary with time. Scope of Content: Disease designations may reflect a specific pathogen (ie, Adenovirus infection), generic pathology (Pneumonia – bacterial) or etiologic grouping(Coltiviruses – Old world). Such classification reflects the clinical approach to disease allocation in the Infectious Diseases Module of the GIDEON web application. -

Sandfly Fever
& My gy co lo lo ro g i y V Tufan and Tasyaran, Virol Mycol 2013, 2:1 Virology & Mycology DOI: 10.4172/2161-0517.1000109 ISSN: 2161-0517 Short Communication Open Access Sandfly Fever: A Mini Review Zeliha Kocak Tufan*, Mehmet A Tasyaran and Tumer Guven Faculty of Medicine, Department of Infectious Diseases and Clinical Microbiology, Ataturk Training and Research Hospital, Yildirim Beyazit University, Ankara, Turkey Introduction TOSV differs from others with its neurotropism and being an etiologic agent of central nervous system infection [24]. Although Sandfly fever, also known as Pappataci fever or phlebotomus fever the SFSV usually causes a self limited benign disease, there are some is an interesting disease mimicking other conditions which causes evidences that SFTV may lead to more severe disease, prolonged fever fever, myalgia and malaise along with abnormalities in liver enzymes and laboratory abnormalities even with neurological involvement and hematological test results [1]. Without suspicion of the disease [1,25]. itself or a presence of an epidemic, it is very hard to diagnose this disease in a non-endemic area, particularly if it is travel associated and The Mediterranean basin is the main area for sandfly fever. Reports if the anamnesis is not clear [1-5]. The differential diagnosis consists are increasingly published every day related with the presence of the of a very board spectrum list of diseases such as viral, parasitic and vector, the virus or the infection itself, from Spain to Croatia, from bacterial infections. Even hematologic malignancies and bone marrow Morocco to Iran, Italy, Portugal and Turkey [7-13,26,27]. -

Dermatobia Hominis Infestation Misdiagnosed As Abscesses in a Traveler to Spain
Acta Dermatovenerol Croat 2018;26(3):267-269 LETTER TO THE EDITOR Dermatobia Hominis Infestation Misdiagnosed as Abscesses in a Traveler to Spain Dear Editor, A 29-year-old woman presented with abscesses tral ring was noted. Ultrasonography identified oval, on her buttock and leg attributed to flea bites inflict- hypoechoic, and hypovascular structures with inner ed 5 days earlier on return to Spain after 2 months echoic lines corresponding to cavities with debris in Guinea-Bissau. Ciprofloxacin was ineffective after and/or larval remains. Larvae were extracted before 7 days, and she was referred for dermatologic evalu- ultrasonography (Figure 1, b). ation. Examination revealed 4 round, indurated, ery- Recommended treatment included topical anti- thematous-violet furunculoid lesions with a 1.5-2 mm septic, occlusion of the infected area with paraffin, central orifice draining serous material. She reported and 1% topical ivermectin; treatment resulted in in- seeing larvae exiting a lesion, and we extracted sever- complete resolution after 7 days. al more (Figure 1). Parasitology identifiedDermatobia Furunculoid myiasis is more common in develop- (D.) hominis (Figure 2). ing countries (1). Cases in Spain are usually imported, Biopsy revealed intense dermal eosinophilic in- since the flies that produce this type of myiasis are not flammatory infiltrate with a deep cystic appearance, found locally. The species most frequently involved surrounded by acute inflammatory infiltrate and are D. hominis from Central and South America (bot- necrotic material. Dermoscopy identified a foramen fly) and Cordylobia anthropophaga from the sub-Sa- surrounded by dilated blood vessels and desquama- haran region (tumbu fly) (2). We believe this was the tion.