Nutrition Update
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Somalia Hunger Crisis Response.Indd
WORLD VISION SOMALIA HUNGER RESPONSE SITUATION REPORT 5 March 2017 RESPONSE HIGHLIGHTS 17,784 people received primary health care 66,256 people provided with KEY MESSAGES 24,150,700 litres of safe drinking water • Drought has led to increased displacement education. In Somaliland more than 118 of people in Somalia. In February 2017 schools were closed as a result of the alone, UNHCR estimates that up to looming famine. 121,000 people were displaced. • Urgent action at this stage has a high • There is a sharp increase in the number of chance of saving over 300,000 children Acute Water Diarrhoea (AWD/cholera) who are acutely malnourished as well cases. From January to March, 875 AWD as over 6 million people facing possible cases and 78 deaths were recorded in starvation across the country. 22,644 Puntland, Somaliland and Jubaland. • Despite encouraging donor contributions, • There is an urgent need to scale up the Somalia humanitarian operational people provided with support for health interventions in the plan is less than 20% funded (UNOCHA, South West State (SWS) especially FTS, 7th March 2017). Approximately 5,917 in districts that have been hard hit by US$825 million is required to reach 5.5 NFI kits outbreaks of Acute Watery Diarrhoea million Somalis facing possible famine until (AWD). Only few agencies have funding June 2017. to support access to health care services. • More than 6 million people or over 50% • According to Somaliland MOH, high of Somalia’s population remain in crisis cases of measles, diarrhea and pneumonia and face possible famine if aid does not have been reported since November as match the scale of need between now main health complications caused by the and June 2017. -
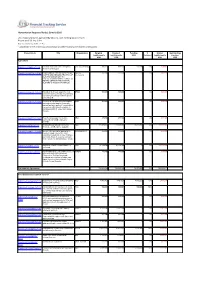
With Funding Status of Each Report As
Humanitarian Response Plan(s): Somalia 2016 List of appeal projects (grouped by Cluster), with funding status of each Report as of 23-Sep-2021 http://fts.unocha.org (Table ref: R3) Compiled by OCHA on the basis of information provided by donors and recipient organizations. Project Code Title Organization Original Revised Funding % Unmet Outstanding requirements requirements USD Covered requirements pledges USD USD USD USD Agriculture SOM-16/A/84942/5110 Puntland and Lower Juba Emergency VSF (Switzerland) 998,222 998,222 588,380 59% 409,842 0 Animal Health Support SOM-16/A/86501/15092 PROVISION OF FISHING INPUTS FOR SAFUK- 352,409 352,409 0 0% 352,409 0 YOUTHS AND MEN AND TRAINING OF International MEN AND WOMEN ON FISH PRODUCTION AND MAINTENANCE OF FISHING GEARS IN THE COASTAL REGIONS OF MUDUG IN SOMALIA. SOM-16/A/86701/14592 Integrated livelihoods support to most BRDO 500,000 500,000 0 0% 500,000 0 vulnerable conflict affected 2850 farming and fishing households in Marka district Lower Shabelle. SOM-16/A/86746/14852 Provision of essential livelihood support HOD 500,000 500,000 0 0% 500,000 0 and resilience building for Vulnerable pastoral and agro pastoral households in emergency, crisis and stress phase in Kismaayo district of Lower Juba region, Somalia SOM-16/A/86775/17412 Food Security support for destitute NRO 499,900 499,900 0 0% 499,900 0 communities in Middle and Lower Shabelle SOM-16/A/87833/123 Building Household and Community FAO 111,805,090 111,805,090 15,981,708 14% 95,823,382 0 Resilience and Response Capacity SOM-16/A/88141/17597 Access to live-saving for population in SHARDO Relief 494,554 494,554 0 0% 494,554 0 emergency and crises of the most vulnerable households in lower Shabelle and middle Shabelle regions, and build their resilience to withstand future shocks. -
Transition Initiatives for Stabilization Plus (Tis+) Program Year Three – Annual Work Plan
TRANSITION INITIATIVES FOR STABILIZATION PLUS (TIS+) PROGRAM YEAR THREE – ANNUAL WORK PLAN (OCTOBER 1, 2017 – SEPTEMBER 30, 2018) Revised November 2017 This publication was produced for review by the United States Agency for International Development. It was prepared by AECOM. Annual Work plan | Transition Initiatives for Stabilization Plus (TIS+) Program i TRANSITION INITIATIVES FOR STABILIZATION PLUS (TIS+) PROGRAM YEAR THREE – ANNUAL WORK PLAN (OCTOBER 1, 2017 – SEPTEMBER 30, 2018) Contract No: AID-623-C-15-00001 Submitted to: USAID | Somalia Prepared by: AECOM International Development DISCLAIMER: The authors’ views expressed in this document do not necessarily reflect the views of the United States Agency for International Development or the United States Government. Year Three - Annual Work Plan | Transition Initiatives for Stabilization Plus (TIS+) Program i TABLE OF CONTENTS Table of Contents ........................................................................................................................................ ii Acronym List .............................................................................................................................................. iii Stabilization Context .................................................................................................................................. 5 Goals and Objectives of USAID and TIS+ ............................................................................................... 6 Methodology ........................................................................................................................................ -

Fråga-Svar Staden Gaalkacyo I Regionen Mudug Samt Gränsen
2011-10-28 Landinformationsenheten Fråga-svar Staden Gaalkacyo i regionen Mudug samt gränsen mellan Puntland och centrala Somalia Fråga Information önskas om staden Gaalkacyo i Somalia. Gaalkacyo en delad stad där en del tillhör Puntland och den andra de södra och centrala delarna av landet. Vilka delar av staden Gaalkacyo tillhör Puntland? Information önskas även om de olika stadsdelarna i Gaalkacyo. Svar Puntland Development Research Center (PDRC) (2010) skriver om gränsen mellan Puntland och södra/centrala Somalia och Somaliland. District and regional administrative jurisdictions of Puntland are lacking clear delineations; yet even the State’s borders with its neighbours from the north and southcentral are still undefined, as a participant from Galkayo recalled: “Let alone the lack of internal jurisdictions, Puntland borders with south-central and Somaliland are not clear. You don’t know where your jurisdiction ends as a State and where the other one starts.” (s. 18) Galkayo – an important crossroads Another area requiring careful attention is the complexity and volatility of Galkayo town and its administrative and social interactions among the various communities living or transiting in this important junction. Galkayo constitutes the epicentre of much of the social, economical and political troubles in the Mudug region as two distinct and often feuding administrations exist. (s. 34) 2 Food Security and Nutrition Analysis Unit- Somalia (FSNAU) (2010) ger i sin rapport en detaljerad beskrivning av Gaalkacyo (norra och södra Gaalkacyo) vad gäller olika samhällsfunktioner i staden såsom skolor, vägar, sjukhus, skolor och marknader m.m. Information finns också till viss del om i vilken del av staden en viss plats eller byggnad finns. -
UN Joint Programme on Local Governance and Decentralized Service Delivery (JPLG)
UNITED NATIONS SOMALIA UN Joint Programme on Local Governance and Decentralized Service Delivery (JPLG) 2nd Quarterly Report 2010 June 2010 UN Joint Programme on Local Governance and Decentralised Service Delivery JPLG 2nd Quarterly Report April – June 2010 Participating UN UN Habitat, UNDP, UNICEF, ILO Cluster/Priority United Nations Transitional Plan for Organization(s): and UNCDF. Area: Somalia 2008 -2010 Outcome Two Implementing Ministries of Interior in Somaliland, Puntland and the Transitional Federal Government and target Partner(s): District Councils. Joint Programme Title: UN Joint Programme on Local Governance and Decentralized Service Delivery (JPLG) Total Approved Joint US$ 37,187,000 Programme Budget: Location: Somaliland, Puntland and south central Somalia SC Approval Date: April 2008 Joint Programme Phase One – 2008 – 2010 and Starting Completion 31/12/ 01/04/2008 Duration: Phase Two 2010 - 2012 Date: Date: 2012 2009 -2010 Through JP pass through with UNDP as AA: Donor Donor Currency USD SIDA 30,000,000 SK 3,378,378 DFID 1,875,000 GBP 2,705,620 NORWAY 6,000,000 NOK 936,622 Through JP and bilateral to UNDP EU 5,000,000 Euro 7,350,000 Parallel Funds 2009 % of Funds Committed: UNDP Italy: $1,800,00; 1,800,000 52% USAID: $458,840 458,840 Approved: DK:$693,823 693,823 Norway: $723,606 723,606 UNDP TRAC: $100,000 100,000 SIDA: $132,000; 132,000 BPCR: $132,930 132,930 Parallel Funds 2009 -2010 4,041,199 UNCDF $832,000 TOTAL APPROVED 2009 – 2010 19,243,819 *SIDA – first tranche = $1,240,695 (transferred from UNDP as AA - % of 18 th March 09). -

2020: Human Rights Report
SOMALIA 2020 HUMAN RIGHTS REPORT EXECUTIVE SUMMARY Somalia is a federal parliamentary republic led by President Mohamed Abdullahi Mohamed “Farmaajo,” whom the bicameral parliament elected in 2017. Farmaajo is the country’s second president since the Federal Government of Somalia was founded in 2012. The federal parliament consists of the 275-member House of the People and the 54-member Upper House. The country’s last parliamentary elections took place from October 2016 to January 2017. Caucuses selected House of the People members, with seats distributed according to clan affiliation and a power-sharing formula. State assemblies elected Upper House members. The parliamentary electoral process was widely viewed as marred by corruption, but the two houses of parliament elected President Farmaajo in a process viewed as fair and transparent. The government of the self-declared Republic of Somaliland controlled its jurisdiction. The 2012 provisional federal constitution states federal police, overseen by civilian leadership in the Ministry of Internal Security, have responsibility for law enforcement and maintenance of order within the country. Many parts of the country remained outside government control, with the insurgent Islamist group al- Shabaab contesting government control. The African Union Mission in Somalia, under civilian African Union leadership, and the Somali National Army, under civilian leadership in the Ministry of Defense, are the primary internal security providers. Civilian authorities did not always maintain effective -
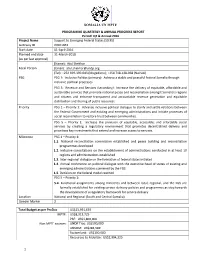
SOMALIA UN MPTF PROGRAMME QUARTERLY & ANNUAL PROGRESS REPORT Period
SOMALIA UN MPTF PROGRAMME QUARTERLY & ANNUAL PROGRESS REPORT Period: Q4 & Annual 2016 Project Name Support to Emerging Federal States (StEFS) Gateway ID 00101061 Start date 01-April-2016 Planned end date 31-March-2018 (as per last approval) (Name): Atul Shekhar Focal Person (Email): [email protected] (Tel): +252 699-390-043 (Mogadishu); +254 718-128-068 (Nairobi) PSG PSG 1: Inclusive Politics (primary): Achieve a stable and peaceful federal Somalia through inclusive political processes PSG 5: Revenue and Services (secondary): Increase the delivery of equitable, affordable and sustainable services that promote national peace and reconciliation amongst Somalia’s regions and citizens and enhance transparent and accountable revenue generation and equitable distribution and sharing of public resources Priority PSG 1 – Priority 1: Advance inclusive political dialogue to clarify and settle relations between the Federal Government and existing and emerging administrations and initiate processes of social reconciliation to restore trust between communities. PSG 5 – Priority 1: Increase the provision of equitable, accessible, and affordable social services by creating a regulatory environment that promotes decentralized delivery and prioritizes key investments that extend and increase access to services. Milestone PSG 1 – Priority 1: 1.1. National reconciliation commission established and peace building and reconciliation programmes developed 1.2. Inclusive consultations on the establishment of administrations conducted in at least 10 regions and administrations established 1.3. Inter-regional dialogue on the formation of federal states initiated 1.4. Annual conference on political dialogue with the executive head of states of existing and emerging administrations convened by the FGS 1.5. Decision on the federal model reached PSG 5 – Priority 1: 5.4. -

SOMALIA Seasonal Monitor June 14, 2019
SOMALIA Seasonal Monitor June 14, 2019 FEWS NET publishes a Seasonal Monitor for Somalia every 10 days (dekad) through the end of the current April to June Gu rainy season. The purpose of this document is to provide updated information on the progress of the Gu season to facilitate contingency and response planning. This Somalia Seasonal Monitor is valid through June 20, 2019 and is produced in collaboration with U.S. Geological Survey (USGS), the Food Security and Nutrition Analysis Unit (FSNAU) Somalia, the Somali Water and Land Information System (SWALIM), a number of other agencies, and several Somali nongovernmental organizations(NGOs). Light to moderate rainfall in south-central Somalia; moderate to heavy rainfall in the North Between June 1 and 10, light rainfall was reported in many parts of the South, but ground information indicates Gedo, Bakool, Bay, and Hiiraan regions received little to no rainfall. Apart from some localized areas, little to no rainfall was reported in Somalia’s central regions. Conversely, the North received moderate to heavy rains in most areas, but rainfall performance was relatively poor in some pastoral areas of Aluula, Bandarbeyla, and Iskushuban districts of Bari region and some pastoral and agropastoral areas of Awdal and Woqooyi Galbeed regions. In south-central areas that received rain, satellite-derived rainfall estimate data (CHIRPS preliminary) recorded precipitation amounts of up to 25 millimeters. In the North, precipitation amounts were recorded at up to 25 mm in most areas, with localized areas receiving up to 50 mm (Figure 1). According to CHIRPS preliminary data, rainfall was generally climatologically average. -

SOMALIË Veiligheidssituatie in Somaliland En Puntland
COMMISSARIAAT-GENERAAL VOOR DE VLUCHTELINGEN EN DE STAATLOZEN COI Focus SOMALIË Veiligheidssituatie in Somaliland en Puntland 18 juni 2017 (update) Cedoca Oorspronkelijke taal: Nederlands DISCLAIMER: Dit COI-product is geschreven door de documentatie- en researchdienst This COI-product has been written by Cedoca, the Documentation and Cedoca van het CGVS en geeft informatie voor de behandeling van Research Department of the CGRS, and it provides information for the individuele asielaanvragen. Het document bevat geen beleidsrichtlijnen of processing of individual asylum applications. The document does not contain opinies en oordeelt niet over de waarde van de asielaanvraag. Het volgt de policy guidelines or opinions and does not pass judgment on the merits of richtlijnen van de Europese Unie voor de behandeling van informatie over the asylum application. It follows the Common EU Guidelines for processing herkomstlanden van april 2008 en is opgesteld conform de van kracht zijnde country of origin information (April 2008) and is written in accordance with wettelijke bepalingen. the statutory legal provisions. De auteur heeft de tekst gebaseerd op een zo ruim mogelijk aanbod aan The author has based the text on a wide range of public information selected zorgvuldig geselecteerde publieke informatie en heeft de bronnen aan elkaar with care and with a permanent concern for crosschecking sources. Even getoetst. Het document probeert alle relevante aspecten van het onderwerp though the document tries to cover all the relevant aspects of the subject, the te behandelen, maar is niet noodzakelijk exhaustief. Als bepaalde text is not necessarily exhaustive. If certain events, people or organisations gebeurtenissen, personen of organisaties niet vernoemd worden, betekent are not mentioned, this does not mean that they did not exist. -

Pillars of Peace
International Peacebuilding Alliance Garowe, Puntland Alliance internationale pour la consolidation de la paix Phone: (+252 5) 84 4480 • Thuraya: +88 216 4333 8170 Alianza Internacional para la Consolidación de la Paz Galkayo Satellite Office Interpeace Regional Office for Eastern and Central Africa Phone: (+252 5) 85 4200 • Thuraya: +88 216 43341184 T +254(0) 20 3862 840/ 2 • F +254(0) 20 3862 845 P.O.Box 14520 – Nairobi, Kenya 00800 [email protected] www.interpeace.org www.pdrcsomalia.org PILLARS OF PEACE SOMALI PROGRAMME In partnership with the United Nations Puntland Note: Mapping the Foundations of Peace Puntland Note: This publication was made possible through the generous contributions and support from: Puntland Note: Mapping the Foundations of Peace Challenges to Security and Rule of Law, Democratisation Process and Devolution of Power to Local Authorities Denmark Schweizerische Eidgenossenschaft Confederation suisse Confédérazione Svizzera Confederaziun svizra Swiss Confederation European Commission Garowe, November 2010 P ILLARS OF P EACE Somali Programme Puntland Note: Mapping the Foundations of Peace Challenges to Security and Rule of Law, Democratisation Process and Devolution of Power to Local Authorities Garowe, November 2010 i Pillars of Peace - Somali Programme Puntland Note: Mapping the Foundations of Peace Pillars of Peace - Somali Programme ii Acknowledgements This research document was made possible by the joint effort and partnership of the Puntland Development Research Center (PDRC) and the International Peacebuilding Alliance (Interpeace). PDRC would like to thank the Puntland stakeholders who actively participated and substantially contributed to the discussions, interviews, community consultations and analysis of the research output. Special thanks also go to the peer reviewers who, looking at the document from the outside, constructively and attentively reviewed the content and form of this document. -

EC DEVELOPMENT PROGRAMME in SOMALIA Ongoing Projects April 2014 Funding Source Contract No. Title Description
EC DEVELOPMENT PROGRAMME IN SOMALIA April 2014 ongoing projects Funding EC Project Woqooyi Galgaduu Lower Middle Lower Middle Source Contract No. Title Description (specific purpose) Start Date End Date Duration EC contribution Implementing partner Manager Location (districts) Awdal Galbeed Togdheer Sanaag Sool Bari Nugaal Mudug d Hiraan Bakool Bay Gedo Juba Juba Shabelle Banadir Shabelle Education Strengthening Capacity of Civil Society Organisations to provide Life skills and Vocational Training for the 1 DCI-NSAPVD DCI-NSAPVD/2011/260-381 Youth The reduction of Youth Unemployment in Somaliland and Puntland. 28-Nov-2011 27-May-2014 30 months 600,000 OXFAM-NOVIB M. MITSCHKE Somaliland & Puntland 120,000 120,000 120,000 120,000 120,000 to contribute towards poverty reduction and MDGs 2 (universal Enhancing Access to Education and education) and 3 (gender equality) by enhancing the education, skills Somaliland & south 2 DCI-NSAPVD DCI-NSAPVD/2012/284-157 Training for persons with Disabilities and status of people with disabilities (PWD) in Somalia. 19-Oct-2012 18-Oct-2015 36 months 337,500 AET - UK M. SABUL Central Somalia 24,107 24,107 24,107 24,107 24,107 24,107 24,107 24,107 24,107 24,107 24,107 24,107 24,108 24,108 Support to Enhanced Participation of to contribute to inclusive development by empowering women with 3 DCI-NSAPVD DCI-NSAPVD/2012/284-246 Women in Somalia (STEP-WINS) capacity to claim their rights in Somalia. 16-Oct-2012 15-Feb-2015 28 months 540,000 ADRA M. MITSCHKE Puntland 135,000 135,000 135,000 135,000 Somaliland Education Sector Support Programme (SESSP) "Hormarinta Elmiga" (Education for Empowerment through Cohesive and Harmonised To contribute to a sustainable, cohesive education system offering 4 EDF FED/2012/ 295-645 System) relevant services to the majority of the relevant age groups in Somaliland 15-Nov-2012 14-Nov-2015 36 months 10,125,000 SC-Denmark M. -
Factor Contributing the Sub-Optimal Uptake of Vaccination in Galkacyo District, Somalia
Factor Contributing the Sub-optimal uptake of vaccination in Galkacyo District, Somalia Author: -Mohamed Farah Abdullahi Author’s department/unit/University: - PUST Somali Supervisor, University: - Dr Sadik Mohamud Aden, Puntland University of Science and Technology. Swedish Supervisor, University: - Dr John Kinsman, Umea University. 1 | P a g e Table of Contents Abstract ......................................................................................................................................................... 4 1. Introduction .......................................................................................................................................... 5 2. Methodology ......................................................................................................................................... 7 Study setting and population .................................................................................................................... 7 General view ......................................................................................................................................... 7 Vaccination Services ................................................................................................................................. 9 Study Design ........................................................................................................................................... 10 Method of Data collection .....................................................................................................................