Annual Report and Accounts 2011/12
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Local Development Framework
Local Development Framework Bolton’s Core Strategy Development Plan Document Adopted 2 March 2011 Shaping the future of Bolton Shaping the future of Bolton 3 List of policies Policy Name Page H1 Healthy 23 A1 Achieving 25 P1 Employment 29 P2 Retail and leisure 31 P3 Waste 33 P4 Minerals 35 P5 Accessibility 37 S1 Safe 38 CG1 Cleaner and greener 41 CG2 Sustainable design and construction 44 CG3 The built environment 47 CG4 Compatible uses 48 SC1 Housing 51 SC2 Cultural and community provision 53 TC1 Civic and retail core 56 TC2 St Helena 57 TC3 St Peter’s 57 TC4 Trinity Gateway 58 TC5 Cultural Quarter 60 TC6 Knowledge Campus 61 TC7 Merchant ’s Quarter 62 TC8 Church Wharf 64 TC9 Little Bolton 64 TC10 Urban Village 65 TC11 Design in the town centre 66 RA1 Inner Bolton 69 RA2 Farnworth 71 RA3 Breightmet 73 M1 Horwich Loco Works 76 M2 Horwich Loco Works 76 M3 Broad location for employment development 78 M4 Middlebrook 79 M5 Parklands and the Lostock Industrial Area 80 M6 Wingates Industrial Estate 80 M7 The M61 corridor built environment 80 OA1 Horwich and Blackrod 83 OA2 Retail and leisure uses at Middlebrook 84 OA3 Westhoughton 85 OA4 West Bolton 86 OA5 North Bolton 88 OA6 Little Lever and Kearsley 90 LO1 Links to other areas 93 IPC1 Infrastructure and planning contributions 96 See also: Appendix 1 - Policy Summary 102 Bolton’s Core Strategy 4 Local Development Framework Contents Chapter 1 Introduction 6 Chapter 2 Spatial portrait and issues 9 Chapter 3 Spatial vision and objectives 17 Chapter 4 Strategic Policies 23 Healthy Bolton 23 Achieving -

Bolton NHS Foundation Trust Booklet
Welcome to Bolton NHS Foundation Trust Making the most of your Practice Learning Placement Royal Bolton Hospital, Minerva Road, Farnworth, Bolton BL4 0JR Tel: 01204 390390 Version 1. (February 2018) Page 1 of 25 Map of the Trust Pre-registration team office Collect ID and Car parking Education team & Library Version 1. (February 2018) Page 2 of 25 Contents Subject Page Number Introduction Page 3 An overview of the organisation and values Page 4 Placement Charter, placement pledges and learner Page 5 expectations Staff Structure-Recognising Staff Members Page 6 Placements running GM Synergy Page 7 Local Induction procedures, supernumerary status and Page 8 mandatory training Obtaining an ID badge & IT access Page 9 Car parking, Page 10 Library services How to place an emergency call How to use the bleep system Page11 Uniform Policy Infection control Sickness and Absence Reporting Page 12 Accompanying/Escorting a patient Page 12 Supporting cultural needs Page 12 Manual handling Page 13 Use of medical devices Page 13 Raising concerns Page 14 Support available on placement Page 15 Contacting support while on placement Page 16 Version 1. (February 2018) Page 3 of 25 Welcome to Bolton NHS Foundation Trust. We hope you enjoy your placement with us and make the most of the valuable learning opportunities that are offered to enable you to develop as a healthcare practitioner in your chosen field. This booklet is designed to offer you information, advice and guidance to enable you to: Access information and resources that will help induct and orientate you into your placement and the trust. -

School Bus Services in Bolton September 2019 to July 2020
7 School Bus Services in Bolton September 2019 to July 2020 Journeys in this leaflet operate on schooldays only, unless otherwise stated. Although provided primarily for school students, members of the public may use these services with the exception of Yellow School Buses. Services are listed alphabetically under school names. An introduction to School buses and concessionary fares for students in Greater Manchester Passengers can pay a fare to the driver for each journey shown on this timetable. However, students will need to show an IGO pass to travel at the concessionary (reduced) fare. If students do not have an IGO pass, they will have to pay a higher fare. Most of the journeys shown in this timetable are funded by Transport for Greater Manchester (TfGM). The majority of TfGM funded services charge a standard fare and also offer daily return tickets. In some cases, the return ticket can also be used for travel on other journeys which serve similar areas – even if it is provided by a different operator. On most services, students can also buy a weekly scholar’s ticket, which costs £7.40. These are ONLY valid on schooldays on school buses and are available from the bus driver on all services where they are applicable. To help the driver, please try to have the correct fare when buying your ticket. A summary of fares and ticketing information on all school services included in this timetable can be found at https://www.tfgm.com/tickets-and-passes/bus-school-bus-services There are also a small number of TfGM funded services where the operator sets the fares. -

521 All Journeys Are Now Run by Cumfybus 521
From 24 April Bus 521 All journeys are now run by Cumfybus 521 Easy access on all buses Little Lever Moses Gate Farnworth New Bury Royal Bolton Hospital Over Hulton Westhoughton Wingates Blackrod From 24 April 2017 For public transport information phone 0161 244 1000 7am – 8pm Mon to Fri 8am – 8pm Sat, Sun & public holidays This timetable is available online at www.tfgm.com Operated by PO Box 429, Manchester, M60 1HX Cumfybus ©Transport for Greater Manchester 17-0270–G521–3500–0217 Additional information Alternative format Operator details To ask for leaflets to be sent to you, or to request Cumfybus large print, Braille or recorded information 178A Cambridge Road, Southport phone 0161 244 1000 or visit www.tfgm.com PR9 7LW Telephone 01704 227321 Easy access on buses Journeys run with low floor buses have no Travelshops steps at the entrance, making getting on Bolton Bus Station and off easier. Where shown, low floor Mon to Fri 7am to 5.30pm buses have a ramp for access and a dedicated Saturday 8am to 5.30pm space for wheelchairs and pushchairs inside the Sunday* Closed bus. The bus operator will always try to provide *Including public holidays easy access services where these services are scheduled to run. Using this timetable Timetables show the direction of travel, bus numbers and the days of the week. Main stops on the route are listed on the left. Where no time is shown against a particular stop, the bus does not stop there on that journey. Check any letters which are shown in the timetable against the key at the bottom of the page. -

Team Bolton Magazine
JUNE 2020 COVID-19 EDITION #hereforyouBolton Thank you to our NHS and key workers // Inside this edition // Features Things to do online, support for May in Bolton - a roundup of the Team businesses, jobs and skills, looking after Bolton response to COVID-19 your wellbeing, money advice, staying Stay safe, have fun - online activity safe, your doctor is still open. to keep the whole family entertained www.bolton.gov.uk / JUNE 2020 1 Contents Welcome to 03 Humanitarian response the first edition 06 Primary Care of Team Bolton 07 Don’t delay We’ve put this publication together to give you and 08 Staying healthy your families some updates about what we have been doing to support the Bolton Family during these difficult times. 09 Looking after your wellbeing The team effort we have seen An incredible army of volunteers since the start of the coronavirus have also been doing their crisis has been incredible, so bit - supporting the council’s 10 May in Bolton thank you to everyone for pulling humanitarian response, and our together and supporting our work. NHS. 12 Our communities Sadly, since the outbreak began, We are all here for you, and are many people in Bolton have working tirelessly so Bolton can lost their lives or faced serious get through this crisis, control the 12 Money advice illness. And we are not out of the virus, and return to normal life as woods yet. In the coming months soon as possible. we must continue our efforts to 13 Benefits control the spread of the virus and Whilst there may still be some save lives. -

Membershipmatters
Membershipmatters THE NEWSLETTER FOR MEMBERS OF BOLTON NHS FOUNDATION TRUST | JANUARY 2017 Chairman’sMembership Letter matters A Time for Reflection We should also reflect on the fact that our £30 The Christmas period million investment programme is now well and truly is a special time for underway. Our plans to upgrade our IT platform everyone. It gives us was matched by investment in our estate and, all a chance to spend notwithstanding the temporary inconvenience time with the family, involved, I was delighted to see the builders on site catch up with relatives and beginning the process of transforming our aged and reflect on the building and supporting plant. It is a visible sign of year gone by. And it’s our determination to maintain Bolton as a great the reflection I want place for patients to receive treatment. to concentrate on. 2016 also saw a real commitment from our There were so many commissioners and our Council colleagues to work highlights it’s difficult collaboratively with us on thinking through how best to know where to start, but it won’t surprise you we can meet the huge pressures now faced by that I wish to highlight our Care Quality Commission health and social care in every corner of the UK. rating as a special moment. A special mention should go to our Clinical The build up to the CQC inspection was something Commissioners who agreed a new way of working to behold. The only analogy I can think of is a with us and this improved our ability to cope with military operation, we had so many terrific examples some extraordinary events together. -

Appendix 1.1 Tfgm Franchising Scheme Document
DRAFT TRANSPORT ACT 2000 The Greater Manchester Franchising Scheme for Buses [20 ] Made [ ] ARRANGEMENT OF THE SCHEME 1. CITATION AND COMMENCEMENT…………………………………………………………………………………1 2. INTERPRETATION………………………………………………………………………………………………….……...1 3. THE FRANCHISNIG SCHEME AREA AND SUB-AREAS……………………………………………………...2 4. ENTRY INTO LOCAL SERVICES CONTRACTS…………………………………………………………….……..2 5. SERVICES UNDER LOCAL SERVICE CONTRACTS……………………………………………………………..3 6. EXCEPTIONS FROM THE SCHEME……………………………………………………………………….………..3 7. SCHEME FACILITIES………………………………………………………………………………………………….…..3 8. PLAN FOR CONSULTING ON OPERATION OF THE SCHEME……………………………………………3 ANNEXES TO THE SCHEME………………………………………………………………………………………………………..5 ANNEX 1: SERVICES INCLUDED – ARTICLE 5…………………………………………………………………….………..5 ANNEX 2: SERVICES INCLUDED – ARTICLE 5.2.3………………………………………………………………………..12 ANNEX 3: EXCEPTED SERVICES – ARTICLE 6………………………………………………………………………………15 ANNEX 4: TEMPORARY EXCEPTIONS – ANNEX 3 PARAGARPHS 1.2 AND 1.3………………………………16 ANNEX 5: FRANCHISING SCHEME SUB-AREAS…………………………………………………………………………..27 Franchising Scheme Document FINAL DRAFT – COMMERCIAL IN CONFIDENCE 1 WHEREAS: A The Transport Act 2000 (as amended) ("2000 Act") makes provision for a franchising authority to make a franchising scheme covering the whole or any part of its area. The GMCA is a franchising authority as defined in the 2000 Act. B The GMCA gave notice of its intention to prepare an assessment of a proposed scheme in accordance with sections 123B and section 123C(4) of the 2000 Act on 30 June 2017. Having complied with the process as set out in the Act, the GMCA may determine to make the scheme in accordance with sections 123G and 123H of the 2000 Act. NOW, therefore, the GMCA, in exercise of the powers conferred on it by sections 123G and 123H of the 2000 Act, and of all other powers enabling it in that behalf, hereby MAKES THE FOLLOWING FRANCHISNG SCHEME (the "Scheme"): 1. -
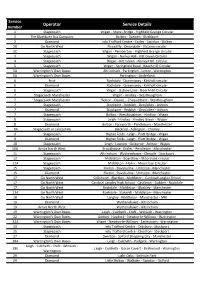
Operator Service Details
Service Operator Service Details number 1 Stagecoach Wigan - Marus Bridge - Highfield Grange Circular 1 The Blackburn Bus Company Bolton - Darwen - Blackburn 2 Diamond intu Trafford Centre - Eccles - Swinton - Bolton 2B Go North West Piccadilly - Deansgate - Victoria circular 2C Stagecoach Wigan - Pemberton - Highfield Grange circular 3 Stagecoach Wigan - Norley Hall - Kitt Green Circular 4 Stagecoach Wigan - Kitt Green - Norley Hall Circular 5 Stagecoach Wigan - Springfield Road - Beech Hill Circular 5A Warrington's Own Buses Altrincham - Partington - Lymm - Warrington 5A Warrington's Own Buses Partington - Sinderland 6 First Rochdale - Queensway - Kirkholt circular 6 Diamond Rochdale - Queensway - Kirkholt circular 6 Stagecoach Wigan - Gidlow Lane - Beech Hill Circular 7 Stagecoach Manchester Wigan - Hindley - Westhoughton 7 Stagecoach Manchester Bolton - Deane - Chequerbent - Westhoughton 7 Stagecoach Stockport - Reddish - Droylsden - Ashton 7 Diamond Stockport - Reddish - Droylsden - Ashton 7 Stagecoach Bolton - Westhoughton - Hindley - Wigan 8 Stagecoach Leigh - Hindley - Hindley Green - Wigan 8 Diamond Bolton - Farnworth - Pendlebury - Manchester 8A Stagecoach in Lancashire Blackrod - Adlington - Chorley 9 Stagecoach Higher Folds - Leigh - Platt Bridge - Wigan 9 Diamond Higher Folds - Leigh - Platt Bridge - Wigan 10 Stagecoach Leigh - Lowton - Golborne - Ashton - Wigan 10A Arriva North West Brookhouse - Eccles - Pendleton - Manchester 11 Stagecoach Altrincham - Wythenshawe - Cheadle - Stockport 12 Stagecoach Middleton - Boarshaw -

The Human Library
Challenging Prejudice in Healthcare – the Human Library Clare Inkster, Associate Dean, Health Education England, North West Team Lenny St Jean, Equality, Diversity and Inclusion Lead, Bolton NHS Foundation Trust Paula Elliott, Library Services Manager, Bolton NHS Foundation Trust Miriam Leach, Foundation Doctor, Bolton NHS Foundation Trust June 2016 Challenging Prejudice in Healthcare – the Human Library Contents Why Human Library? . 3 Who was involved? . 3 When and where did events take place? . 4 How were events organised? . 5 What were the outcomes? . 7 Book reviews . 8 Case studies . 12 Book questionnaires . 13 A word about values . 14 Staff evaluation . 15 Interest from external agencies . 15 What worked well? . 15 Lessons learned . 16 Overall . 17 Thanks to . 18 Resources . 18 Appendix 1 – Book list . 19 Appendix 2 – A nurse’s reflection on the experience . 21 Appendix 3 – Values questionnaire transcripts . 23 Appendix 4 – Staff comments . 32 2 Challenging Prejudice in Healthcare – the Human Library Why Human Library? Health care learners will spend their careers caring for people from all sectors of society. In order to deliver the highest quality care, it is important for them to understand principles of equality, diversity and inclusion in the real world. The Human Library supports this aim by promoting social inclusion through respectful conversation. It provides an opportunity for learners to get a better understanding of how an individual’s culture, social identity and expressed beliefs will impact on the decisions they make about their care and treatment. This is a key component in developing the ‘patient as partner’ approach that will improve both patient experience and outcomes. -

Bolton Health Information Partnership
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Bolton Institutional Repository (UBIR) IN DEPTH Bolton Health Information Partnership An increased emphasis on ensuring greater patient and public involvement within the health and social care agenda has created a greater need for information provision tailored towards the needs of patients and the wider public. Dawn Grundy, Paula Elliott and Amanda Stevens explain how a cross-sector partnership in Bol- ton is changing the way healthcare information is accessed. INFORMAL partnerships between health and information organisations in Bolton have been embraced and expanded with the formal creation of Bolton Health Informa- tion Partnership (BHIP). The following article looks at the formation and work of Dawn Grundy, that partnership over the last two years. Academic Librarian, Faculty of Health & Wellbeing, University Our origins of Bolton. The initial consortium formed in 2017, bringing together representatives from: l Bolton Library and Museum Services l Macmillan Cancer Information Services l Bolton NHS Foundation Trust Library Services l University of Bolton Library Paula Elliott, Library Manager, Bolton NHS Historically, informal partnerships between Foundation Trust Library Services. some of these organisations had resulted in library access agreements being set up and collaboration at events such as a Human Library and the annual Bolton Health Mela. However, by 2017 a new impetus to work together came with Health Information Week and the Knowledge for Healthcare initiative Amanda Stevens, Developing and building local networks and Library, Museum and partnerships which sought to bring together Information Services Team Leader, Bolton local library services across a range of organi- Library and Museum sations to provide health information. -

Farnworth (FNW).Indd 1 11/10/2018 10:32
Farnworth Station i Onward Travel Information Local area map Contains Ordnance Survey data © Crown copyright and database right 2018 & also map data © OpenStreetMap contributors, CC BY-SA Buses Main destinations by bus (Data correct at September 2018) DESTINATION BUS ROUTES BUS STOP Bolton ^ 2, 8, 37 F 512 A Bury 512, 513 E Great Lever 2 F 2 F Harper Green 512 B Highfi eld 501, 557 Bus Station 512 A Kearsley ^ 2, 8, 512, 513, 557 E Little Hulton 68 Bus Station Little Lever 521 Bus Station New Bury (Farnworth) 68, 521 Bus Station 512 A Outwood 512, 513 E Over Hulton 521 Bus Station Prestolee 557 E 512 A Radcliffe 512, 513 E 512 B Royal Bolton Hospital 501, 521 Bus Station 512 A Stoneclough/Ringley 512, 513 E Swinton 2, 37 E 68 Bus Station Walkden 37 E Whitefi eld 513 E For bus times and days of operation please see bus stop timetables or contact Traveline. Notes Rail replacement buses depart from bus stops Market Street. ^ Direct trains operate to this destination from this station. Farnworth station has no taxi rank or cab offi ce. Advance booking is Taxis essential, please consider using the following local operators: S and D Taxis Atlantis Private Hire Delta Private Hire (Inclusion of this number doesn’t represent any endorsement of the taxi fi rm) 01204 704 040 01204 577 777 01204 794 141 Further information about all onward travel www OnlineLocal Cycle Info www SustransNational Cycle Info Bus Times www PLUSBUS See timetable bolton.gov.uk sustrans.org.uk displays at bus Find the bus times for your stop. -

A Brief History of Bolton Art Circle
A Brief History of Bolton Art Circle Forward Artists have always played an important part in drawing attention to the different aspects of the world we live in. Bolton has been fortunate in the number of people with such a talent. This History chronicles over half a century of promoting art in Bolton and outlines the achievements, heartaches and various characters involved with Bolton Art Circle. Since the founding just after the Second World War, almost every Boltonian involved with visual arts has at some time been a member. However, just as our appreciation of art changes with time, so has Bolton Art Circle developed into a movement that opens its doors to everyone who has either a sporadic or longer-term practical interest in art. By staging an exciting International Art Competition and Exhibition in July 1996 to celebrate its half-century, the Circle offered the whole community an opportunity to become involved in its aspirations, which are to bring the appreciation of the visual arts into everyone’s life. The History was researched by the late Alan Brooks, who delved into the archives and taxed the memories of many long-standing members and produced a fascinating booklet, which was in great demand. The following is primarily Alan’s "Brief History", but has been edited and updated for this website by myself. Roland Arthur, Honorary Secretary October 2002 1. The Start The initial impetus for the formation of the Circle came from a discussion held in the Process Department of Tillotsons Ltd., (Bolton Evening News), where four people talked about the idea of forming a group for the practice and furtherance of art.