Compartment Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Skinny Puppy Éÿ³æ¨‚Å°ˆè¼¯ ĸ²È¡Œ (ĸ“Ⱦ‘ & Æ—¶É—´È¡¨)
Skinny Puppy 音樂專輯 串行 (专辑 & 时间表) Weapon https://zh.listvote.com/lists/music/albums/weapon-7978041/songs The Process https://zh.listvote.com/lists/music/albums/the-process-7758446/songs VIVIsectVI https://zh.listvote.com/lists/music/albums/vivisectvi-7907100/songs The Greater Wrong of the Right https://zh.listvote.com/lists/music/albums/the-greater-wrong-of-the-right-1761720/songs Rabies https://zh.listvote.com/lists/music/albums/rabies-7278724/songs The Greater Wrong of the Right https://zh.listvote.com/lists/music/albums/the-greater-wrong-of-the-right-live-7738017/songs Live Remix Dystemper https://zh.listvote.com/lists/music/albums/remix-dystemper-7311955/songs Bootlegged, Broke, and In Solvent https://zh.listvote.com/lists/music/albums/bootlegged%2C-broke%2C-and-in-solvent-seas- Seas 16244609/songs https://zh.listvote.com/lists/music/albums/mind%3A-the-perpetual-intercourse- Mind: The Perpetual Intercourse 10585691/songs Twelve Inch Anthology https://zh.listvote.com/lists/music/albums/twelve-inch-anthology-7857610/songs The Singles Collect https://zh.listvote.com/lists/music/albums/the-singles-collect-7764468/songs Remission & Bites https://zh.listvote.com/lists/music/albums/remission-%26-bites-7311918/songs B-Sides Collect https://zh.listvote.com/lists/music/albums/b-sides-collect-4833705/songs https://zh.listvote.com/lists/music/albums/doomsday-%28skinny-puppy-album%29- Doomsday (Skinny Puppy album) 3714061/songs Bites https://zh.listvote.com/lists/music/albums/bites-1761169/songs Cleanse Fold and Manipulate https://zh.listvote.com/lists/music/albums/cleanse-fold-and-manipulate-5130586/songs -

1 T H E T Akes C< in N Ontrol E T,. L Over I Hong Kong
1 ■T h e T i n n e t , . T WKJ : T w in Falls, Idaho,hQ/92nd year. N o. 18282________________ Tuesday, J 50 ccnts 'G o o d m oiRNING r ■ G j h i n a t ^akes c<ontroll over HongI Kong W e a t h e r Today: Partly cloudyr withw: a slight r. chance of showers thrchrough BBritish end coli)lonial mle aminid celebrationns, pageantry: MH tonight. West winds; nearne 15 mph. le Atioclated Preii_____________ ' th e worl3rid stage, although Prince:e Highs in the low 70s.5. LowsL near ~ 7 U.S. attltudt u d e - A 5 ;s. along with Chris Patten.n. 45. Page A2 ^ ^ '4 HONG KONG ~ With aJ n iid - th e la sIt t, British governor, m an ag ed:d H ^nj|5<3RlK l niglight change of flags, an anXiiiXioui, ' What's lienfieXt - A7 to turnn 1their retreat into a digni-li- jV/MHSIffin - Xcited Hong Kong ended itsIS :1 5 6 - _________________^_____________________ fied, restsstniined spectacle of Britisiiill ear British colonial era < ;ism. ■ M a g i c V a l l e y “ “".‘I mdconTV.ntlminisinistered the coup Ht EY W m mbarked Tuesdoy on a uncen Hong Kong’s 6.3 million peo-0- i-century colonial- - , ew'age under the sovereignc: S '” ' '» le biggest question was still11 d of an era: - . ism arid erased wh».chinmwl .B o n1 ee X u lta n t C om m unist China. ivered: Can a free capitalist ur genera- The few pro-democracy protiri.csK »lw»ss rcsardcd as 0 fimdamentol „dctysr survive in the embrace of a nd the humiliation — Bnts.mam’s seizure of Xommur tnsofstu- K n H BBST ■ "'erere sparse and peaceful, and ■unist p o w er, e v e n o n e th aIt t jpimc. -
UNIVERSITY of CALIFORNIA SANTA CRUZ EVERYDAY IMAGININGS UNDER the LION ROCK: an ANALYSIS of IDENTITY FORMATION in HONG KONG a Di
UNIVERSITY OF CALIFORNIA SANTA CRUZ EVERYDAY IMAGININGS UNDER THE LION ROCK: AN ANALYSIS OF IDENTITY FORMATION IN HONG KONG A dissertation submitted in partial satisfaction of the requirements for the degree of DOCTOR OF PHILOSOPHY in POLITICS by Sarah Y.T. Mak March 2013 The Dissertation of Sarah Y.T. Mak is approved: _______________________________ Professor Megan Thomas, Chair ________________________________ Professor Ben Read ________________________________ Professor Michael Urban ________________________________ Professor Lisa Rofel ______________________________________ Tyrus Miller Vice Provost and Dean of Graduate Studies Copyright © by Sarah Y.T. Mak 2013 TABLE OF CONTENTS List of Figures ..................................................................................................................... v Abstract ...............................................................................................................................vi Acknowledgments.........................................................................................................viii CHAPTER ONE: INTRODUCTION ..............................................................................................1 I. SETTING THE SCENE .......................................................................................................1 II. THE HONG KONG CASE ............................................................................................. 15 III. THEORETICAL STARTING POINTS ........................................................................... -

An Exploration of How Schools Cope Psychologically with a Critical
AN EXPLORATION OF HOW SCHOOLS COPE PSYCHOLOGICALLY WITH A CRITICAL INCIDENT, CONSIDERING SUPPORT PROCESSES, WITH PARTICULAR REFERENCE TO DECISION-MAKING REGARDING OUTSIDE SUPPORT, ESPECIALLY SUPPORT AVAILABLE FROM A LOCAL AUTHORITY C.I.R.T. (CRITICAL INCIDENT RESPONSE TEAM) by Anthony O’Brien Atwell A thesis submitted to The University of Birmingham in part fulfilment for the degree of Professional Doctorate in Educational Psychology Ed Psych D School of Education College of Social Sciences University of Birmingham October 2016 University of Birmingham Research Archive e-theses repository This unpublished thesis/dissertation is copyright of the author and/or third parties. The intellectual property rights of the author or third parties in respect of this work are as defined by The Copyright Designs and Patents Act 1988 or as modified by any successor legislation. Any use made of information contained in this thesis/dissertation must be in accordance with that legislation and must be properly acknowledged. Further distribution or reproduction in any format is prohibited without the permission of the copyright holder. Abstract A Critical Incident (C.I.) is a traumatic event which typically occurs suddenly and unexpectedly, often resulting in serious injury or a death. This thesis explores how schools cope psychologically with a C.I. from the perspectives of the school decision-makers. It considers support strategies in the short, medium and long-term and at a whole-school, group and individual level. The process of support is interpreted in terms of its role towards enabling normalisation. The exploration makes particular reference to decision-making factors for schools regarding outside support post-Critical Incident, especially that which is available from a Local Authority Critical Incident Response Team (C.I.R.T.). -

The Necemoon Album | Volume 1
Volume 1 1 The NeceMoon Album, Page 1 The NeceMoon Album Technologies and Strategies to Keep Moving Forward By Necemon Yai First edition Published by Evasium ® April 2018 London, UK TheAlbum.NeceMoon.com The contents of this file are protected under the UK Copyright, Designs and Patents Act 1988. License This file is free to distribute and give away to as many people as you would like. I only ask that you do not sell it or publish the content onto any website. If you use any quotes from this document, give me credit and link to the original file. If you write a book and I quote you, I will give you credit and links too. © Necemon Yai [email protected] www.necemonyai.com All Rights Reserved. Version 1.0.7.235 To the ones I lost, to the ones I got back For each one that gets lost, ten get laid back Volume 1 | 4 Table of Contents Introduction ....................................................................................................................................................... 7 For All Practical Purposes ................................................................................................................................ 10 Volume 1: Moon Light (Softcore) ............................................................................................ 11 Chapter 1: Strategy and Tactics ......................................................................................................... 12 Words to Live By (by Monty Oum) ................................................................................................................. -

Skinny Puppy Album Weapon
Skinny puppy album weapon click here to download Weapon by Skinny Puppy, released 28 May 1. wornin' 2. illisiT 3. and voicing a stance on the issues of our times, the new album, Weapon, is no exception. Find a Skinny Puppy - Weapon first pressing or reissue. Complete your Skinny Puppy collection. Shop Vinyl and CDs. Weapon is a stand out album in Skinny Puppy's career. It is an appropriate evolution from The Process > GWOTR > Mythmaker > Handover > Weapon. Weapon. Skinny Puppy - Weapon [limited Edition Lp Vinyl] - www.doorway.ru Music. The first taste of the upcoming album is Last Dance. A six track EP featuring four new. Weapon, the twelfth studio album from Skinny Puppy, is not your older brother's Skinny Puppy. Well, it is and it isn't. Those of us of a certain age. Skinny Puppy - Weapon Album, Illisit, Official Music Video. taken from the album WEAPON www.doorway.ru?prodnum=MET+ Skinny Puppy 'Weapon' (Metropolis Records) CD/DL Available now. Shocking. A new Skinny Puppy album and they sound more like Portion. Skinny Puppy - Weapon review: Skinny Puppy inject a bit of 80s Skinny Puppy have never really released the same album twice, but up. A Brutal Resonance review of Skinny Puppy - Weapon (Industrial) I'm just going to review this album like any other and hopefully you'll listen. Speaking as a put-off old school fan, Skinny Puppy's "Weapon" is actually refreshing, and I highly recommend this album to my jaded peers. Skinny Puppy is one of those bands that are not afraid to change and evolve. -
Pdf/How-Charter-Cities-Could- Transform-The-Developing-World-April-2012.Pdf (03/03/2015)
Fabio Armao Inside War Understanding the Evolution of Organised Violence in the Global Era Fabio Armao Inside War Understanding the Evolution of Organised Violence in the Global Era Managing Editor: Magdalena Randall-Schab Langueage Editor: Adam Tod Leverton Translated by Kora E. Bättig von Wittelsbach and Emilia Bianca Pisani Published by De Gruyter Open Ltd, Warsaw/Berlin Part of Walter de Gruyter GmbH, Berlin/Munich/Boston This work is licensed under the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 license, which means that the text may be used for non-commercial purposes, provided credit is given to the author. For details go to http://creativecommons.org/licenses/by-nc-nd/3.0/. Copyright © 2015 Fabio Armao ISBN: 978-3-11-047119-9 e-ISBN: 978-3-11-047124-3 Bibliographic information published by the Deutsche Nationalbibliothek The Deutsche Nationalbibliothek lists this publication in the Deutsche Nationalbibliografie; detailed bibliographic data are available in the Internet at http://dnb.dnb.de. Managing Editor: Magdalena Randall-Schab Langueage Editor: Adam Tod Leverton www.degruyteropen.com Cover illustration: © Fabio Armao Contents Introduction X Acknowledgments XVII Part I 1 Old Wars, New Wars 2 1.1 A Trick of Nature 3 1.2 The Role of ‘American Social Science’ 5 1.3 The Foundations of a New Paradigm 8 1.3.1 Ontology 8 1.3.2 Epistemology 11 1.3.3 Methodology 14 1.4 The Post-Cold War Scenario 16 1.4.1 The End and the Beginning 17 1.4.2 The De-construction of the State 19 1.4.3 The Revenge of the Peripheries 20 1.4.4 The -

Compartment Syndrome
Compartment Syndrome A Guide to Diagnosis and Management Cyril Mauffrey David J. Hak Murphy P. Martin III Editors Compartment Syndrome Cyril Mauffrey • David J. Hak Murphy P. Martin III Editors Compartment Syndrome A Guide to Diagnosis and Management Editors Cyril Mauffrey , MD, FACS, FRCS David J. Hak, MD, MBA, FACS Professor of Orthopedic Surgery Central Florida Regional Hospital Interim Director of Service Hughston Orthopedic Trauma Group Department of Orthopedics Sanford, FL Denver Health Medical Center USA Denver, CO USA Murphy P. Martin III, MD Assistant Professor Department of Orthopedic Surgery Tulane University School of Medicine New Orleans, LA USA This book is an open access publication. ISBN 978-3-030-22330-4 ISBN 978-3-030-22331-1 (eBook) https://doi.org/10.1007/978-3-030-22331-1 © The Editor(s) (if applicable) and The Author(s) 2019 Open Access This book is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made. The images or other third party material in this book are included in the book’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the book's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. -

Here Is a Photograph That Is Marked As Copyright to Its Creator, Which Was Used with Permission and May Not Be Included in Derivative Works
issue #(1.5) graceless a journal of the radical gothic 1 GRACELESS Issue (One point Five) published in May 2012, a special zine format preview for the upcoming full Issue Two Contributors and Editors: Enola Dismay, Holger Karas & Jenly (WWW.SEVENTH-SIN.DE), Margaret Killjoy (WWW.BIRDSBEFORETHESTORM.NET), and Robert Inhuman. Cover photo: Beatrice Schleyer WWW.JUJU-MECHANIX.COM Graceless can be contacted at: WWW.GRACELESS.INFOGRACELESS [email protected] !is work is licensed under the Creative Commons Attribution- NonCommercial-ShareAlike 3.0 Unported License. To view acopy of this license, visit HTTP://CREATIVECOMMONS.ORG/LICENSES/BY-NC-SA/3.0/ or send a letter to: Creative Commons, 171 Second Street, Suite 300 San Francisco, California, 94105USA What this license means is that you are free (and encouraged) to take any content from Graceless and re-use it in part or whole, or make your own work that incorporates ours, as long as you: attribute the creator of the work, share the work with the same license, and are using the product non- commercially. Note that there is a photograph that is marked as copyright to its creator, which was used with permission and may not be included in derivative works. We have chosen a Creative Commons licensing because we believe in free cultural exchange but intend to limit the power of capi- talism to co-opt our work for its twisted ends. Adobe Garamond Pro is our body font. Colwell HPLHS serves for our most of our headers. Century Gothic is used for bylines, footers, and some subheads.. 2 RADICAL GOTHIC Radical When we say “radical,” we are not speaking of a speci"c ideology, but we’re also not talking about politics like who’s gonna vote for whom. -

Human Rights Watch
HUMAN RIGHTS WATCH WORLD REPOR T | 2013 EVENTS OF 2012 H U M A N R I G H T S WATCH WORLD REPORT 2013 EVENTS OF 2012 Copyright © 2013 Human Rights Watch All rights reserved. Printed in the United States of America ISBN-13: 978-1-60980-389-6 Front cover photo: Syria – A mother and son anguished over the loss of her other two sons, killed by a mortar attack launched by the Syrian army. Homs province, February 20, 2012. © 2012 Alessio Romenzi Back cover photo: Greece – Ali Mohammadi, a 25-year-old Afghan asylum seeker who was attacked by thugs in Athens, Greece, in March 2011. © 2011 Zalmaï for Human Rights Watch Cover and book design by Rafael Jiménez www.hrw.org Human Rights Watch is dedicated to protecting the human rights of people around the world. We stand with victims and activists to prevent discrimination, to uphold political freedom, to protect people from inhumane conduct in wartime, and to bring offenders to justice. We investigate and expose human rights violations and hold abusers accountable. We challenge governments and those who hold power to end abusive practices and respect international human rights law. We enlist the public and the international community to support the cause of human rights for all. WORLD REPORT 2013 HUMAN RIGHTS WATCH Human Rights Watch is one of the world’s leading independent organizations dedicated to defending and protecting human rights. By focusing international attention where human rights are violated, we give voice to the oppressed and hold oppressors accountable for their crimes. -

Unabridged AFM Product Guide + Stills
AFM PRODUCTPRODUCTwww.thebusinessoffilmdaily.com/AFM2012ProductGuide/AFMProductGuide.pdfGUIDEGUIDE Hillridge (Parker Posey), the head of the high school soccer team’s two week trip Director: Alex de la Iglesia 108 MEDIA hospital’s charity foundation, reluctantly to Italy. Dynamic friendships, rivalries Writer: Alex de la Iglesia decides to take Adan into her home for a and personal secrets compete in this tale Key Cast: José Mota, Salma Hayek CORPORATION few days. Through his ongoing and of one boy’s stirring coming of age in a Delivery Status: Screening 108 Media Corporation, 225 sometimes inappropriate slogans, Adan foreign land. Year of Production: 2011 Country of Commissioners St., Suite 204,, Toronto, slowly begins to affect Karen and the Origin: Spain Ontario Canada, Tel: 1.637.837.3312, MYN BALA: WARRIORS OF THE dysfunctional relationship she has with In this hilarious comedy, Alex de la http://www.108mediacorp.com, STEPPE her daughter Meghan. Epic Adventure (125 min) Iglesia makes fun of lack of today's [email protected] Director: Akan Satayev morals in media and depiction of Sales Agent, Producer BUFFALO GIRLS Documentary (66min) Kazakhstan, 1729: A ferocious Mongol financial crisis through the eyes of an At AFM: Abhi Rastogi (CEO) Buffalo Girls tells the story of two 8- tribe sweeps across the steppes, and unemployed advertising executive who Office: Loews Hotel Suite 601 year-old-girls, Stam and Pet, both Kazakh sultans leave their people to fend decides to take advantage of an accident AUTUMN BLOOD Director: Reed Morano (Frozen River) professional Muay Thai prizefighters. Set for themselves. Young Sartai and other he has after yet another humiliating work Writer: Stephen Barton and Markus in small villages throughout rural survivors flee to the mountains. -
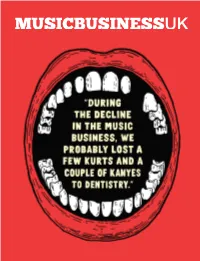
Q1 2020 Q1 2020 Lewis Lewis Capaldi Mabel Dav E Celeste Billie Eilish
Q1 2020 Q1 2020 CONGRATULATIONS ON YOUR BRIT YOUR ON CONGRATULATIONS FROM EVERYONE AT UNIVERSAL MUSIC UNIVERSAL AT EVERYONE FROM s SUCCESS LEWIS LEWIS CAPALDI MABEL DAV E CELESTE BILLIE EILISH 11 WELCOME EDITOR’S LETTER In this issue... The popular modern maxim to ‘speak my truth’ Tim Ingham long it will take, or how much ownership they tacitly yet proudly argues there is always more are giving up. Then, they compete for attention 10 YouTube Music than one retelling of any event – bending every and resources that are already spread thin. It’s a Dan Chalmers & Lyor Cohen occurrence into a fiction-splashed narrative fight for creative and financial freedom.” onto which our own subjective viewpoint can, This attack on traditional label advances is the and should, be impressed. It adds to a collective latest broadside to be thrown on a voluminous 22 Kyn Entertainment erosion of the idea of the gospel – whether pile. Elsewhere, rapper Mase recently castigated Sonny Takhar religious, journalistic or anecdotal – furthering Puff Daddy on Instagram regarding a historical a rabid culture of self-trust. It is malleable, and publishing deal between the pair. Mase said that therefore open to manipulation, ego and error. Puff “purposely starved your artist”, adding: “For 28 The BRIT Awards It is the definition of Trump’s America. example, u still got my publishing from 24 years How did we end up in this situation, where ago in which u gave me $20k.” one person’s reality – no matter how warped by What is lost in both Rabkin Lewis and Mase’s self-serving myopia – has become more valued salvos here is a rounded view – the rapidly- 38 Nick Burgess & Mark Mitchell Parlophone than art, and more trusted than evidence? vanishing gift of being taught all sides of the I mean, it can’t all be down to TikTok.