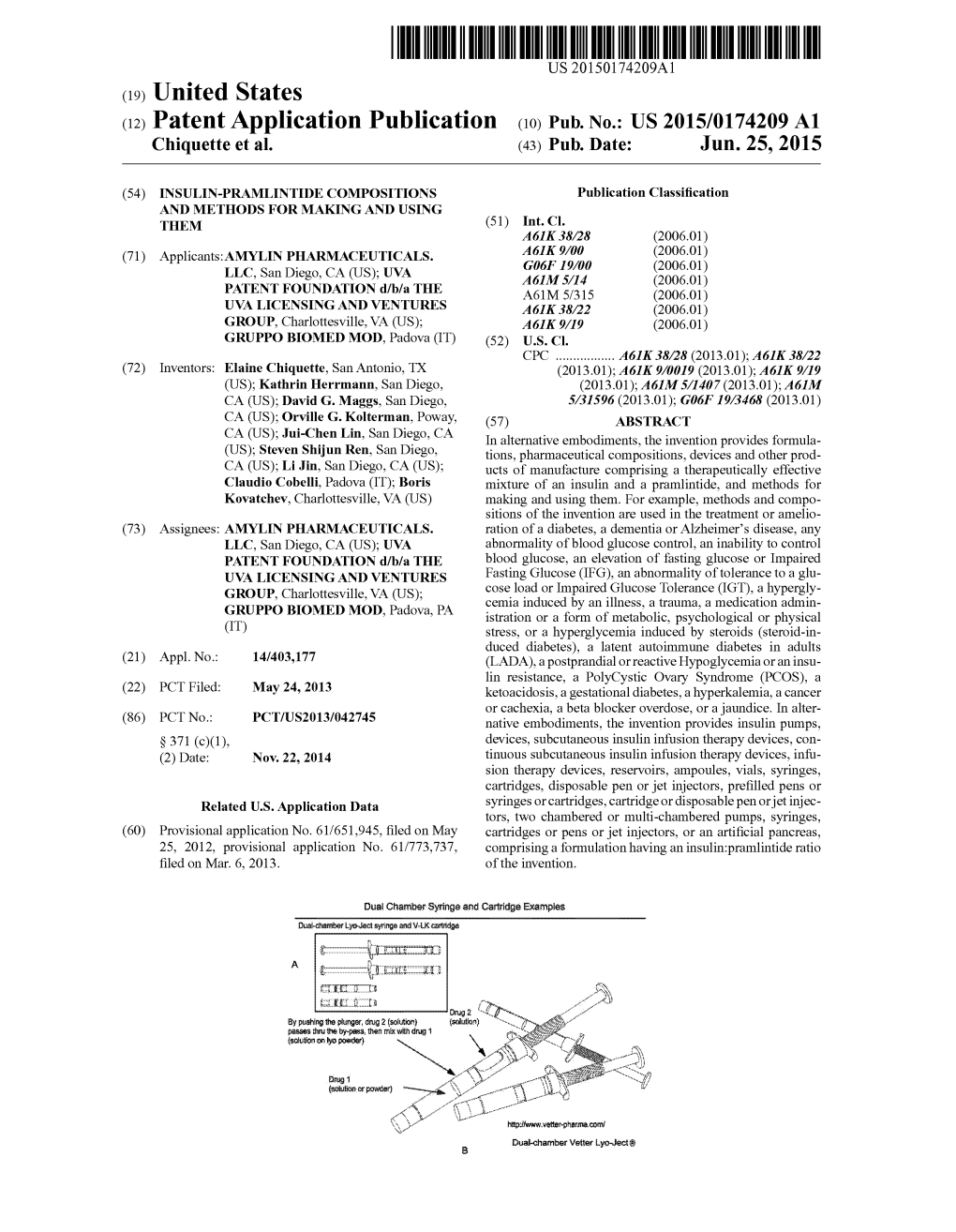
(12) Patent Application Publication (10) Pub. No.: US 2015/0174209 A1 Chiquette Et Al
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Study on Recent Implication of Nanotechnology in Drug Delivery Systems
Available online a t www.scholarsresearchlibrary.com Scholars Research Library Der Pharmacia Lettre, 2015, 7 (7):213-220 (http://scholarsresearchlibrary.com/archive.html) ISSN 0975-5071 USA CODEN: DPLEB4 A study on recent implication of nanotechnology in drug delivery systems Mahendra Pratap Singh 1, Parjanya Kumar Shukla 1,2* , Amita Verma 2 and Ramesh Patel 1 1Krishnarpit Institute of Pharmacy, Allahabad 2Department of Pharmaceutical Sciences, Faculty of Health Science, Sam Higginbottom Institute of Agriculture, Technology & Sciences, Allahabad, India _____________________________________________________________________________________________ ABSTRACT Efficient drug targeting to diseases by circumventing all the shortcomings of conventional drug delivery systems can be achieved by the significant approach of advances in nanotechnology. Nanotechnology will affect our lives tremendously over the next decade in very different fields, including medicine and pharmaceutical Sciences. Most of the available drugs now are lipophilic in nature and this stands as challenging aspect faced for scientists to formulate and deliver for better efficacy, so nanoparticles, nanosuspension, nanocapsules are used now days to deliver these drugs with greater bioavailability and also have been adopted to improve the solubility of poorly soluble drugs. The use of nanoparticles is an universal formulation approach to increase the therapeutic performance of drugs in any route of administration. This review article describes the preparation methods, physicochemical -

A Gellan-Based Fluid Gel Carrier for Spray Delivery
AGELLAN-BASEDFLUIDGELCARRIERFOR SPRAY DELIVERY by BRITT TER HORST Athesissubmittedto The University of Birmingham for the degree of DOCTOR OF PHILOSOPHY School of Chemical Engineering College of Engineering and Physical Sciences The University of Birmingham May 2019 UNIVERSITYDF BIRMINGHAM University of Birmingham Research Archive e-theses repository This unpublished thesis/dissertation is copyright of the author and/or third parties. The intellectual property rights of the author or third parties in respect of this work are as defined by The Copyright Designs and Patents Act 1988 or as modified by any successor legislation. Any use made of information contained in this thesis/dissertation must be in accordance with that legislation and must be properly acknowledged. Further distribution or reproduction in any format is prohibited without the permission of the copyright holder. Abstract Autologous cell transplantation is a promising approach to enhance burn wound re- epithelialisation. It was introduced to clinical practice decades ago with current delivery techniques involving spraying autologous cultured or uncultured cells in low-viscosity sus- pensions. This delivery method is limited since it results in an uneven distribution on the wound bed and cell loss as the liquid is not retained on the skin surface. In this thesis, a sprayable gel that solidifies on the surface of the skin has been developed to circumvent this problem. A gellan-based fluid gel system was developed with flexible viscoelastic properties that can be tuned by a biocompatible polymer concentration and ionic strength to facilitate spray delivery. The material liquefies at high shear during spraying with self-healing properties of the gel causing it to solidify on the receiving sur- face. -

Powders Are Intimate Mixtures of Dry, Finely Divided Drugs And/Or Chemicals That May Be Intended for Internal Or External Use
Powders are intimate mixtures of dry, finely divided drugs and/or chemicals that may be intended for internal or external use. Advantages/Disadvantages flexibility in compounding good chemical stability Ease of administration time-consuming not well-suited to dispense unpleasant tasting, hygroscopic or deliquescent drugs inaccuracy of dose Types Medicated Aerosol Preparation Weighing of ingredients Comminuting Blending or mixing Weighing of individual dose Materials Active ingredients Packaging Types of material used to pack/dispense divided powders Foil plastic bag used for volatile vegetable parchment thin, semiopaque, moisture-resistant white bond without moisture-resistant properties Glassine glazed, transparent, moisture-resistant paper used for volatile to a certain extent Waxed transparent-water-proof paper used for hygroscopic and volatile drugs Seidlitz powder is the name with which is commonly known a medication composed by a mixture of tartaric acid, sodium bicarbonate, and potassium sodium tartrate, used as a mild cathartic by dissolving in water and drinking. After ingestion, the powder combines with gastric juices developing intestinal gases which are somewhat helpful in evacuating the bowels. This medication's name comes from the Seidlitz Saline Springs of Bohemia (now Sedlčany in the Czech Republic), which were rather famous in Europe at the time this medication was first marketed in the late 19th century, even though the foregoing laxative constituents do not represent those of the springs named. Use of Each ingredient – act as acid and base which react in the presence of water to cause effervescence Use of Preparation - mild cathartic/laxative Appearance – white powder Storage – store in air tight containers Granules are prepared agglomerates of powdered materials, may be used per se for the medicinal value of their content or they may be used for pharmaceutical purposes, as in making tablets. -

Glioblastoma Treatments: an Account of Recent Industrial Developments
REVIEW published: 13 September 2018 doi: 10.3389/fphar.2018.00879 Glioblastoma Treatments: An Account of Recent Industrial Developments Edouard Alphandéry 1,2* 1 Institut de Minéralogie, de Physique des Matériaux et de Cosmochimie, UMR 7590 CNRS, Sorbonne Universités, UPMC, University Paris 06, Paris, France, 2 Nanobacterie SARL, Paris, France The different drugs and medical devices, which are commercialized or under industrial development for glioblastoma treatment, are reviewed. Their different modes of action are analyzed with a distinction being made between the effects of radiation, the targeting of specific parts of glioma cells, and immunotherapy. Most of them are still at a too early stage of development to firmly conclude about their efficacy. Optune, which triggers antitumor activity by blocking the mitosis of glioma cells under the application of an alternating electric field, seems to be the only recently developed therapy with some efficacy reported on a large number of GBM patients. The need for early GBM diagnosis is emphasized since it could enable the treatment of GBM tumors of small sizes, possibly easier to eradicate than larger tumors. Ways to improve clinical protocols by strengthening preclinical studies using of a broader range of different animal and tumor models are also underlined. Issues related with efficient drug delivery and crossing of Edited by: blood brain barrier are discussed. Finally societal and economic aspects are described François E. Paris, University of Nantes, France with a presentation of the orphan drug status that can accelerate the development of Reviewed by: GBM therapies, patents protecting various GBM treatments, the different actors tackling Tullio Florio, GBM disease, the cost of GBM treatments, GBM market figures, and a financial analysis Università di Genova, Italy of the different companies involved in the development of GBM therapies. -
Lipid-Polymer Hybrid Nanoparticles As a Next-Generation Drug Delivery
Providence St. Joseph Health Providence St. Joseph Health Digital Commons Articles, Abstracts, and Reports 1-1-2019 Lipid-polymer hybrid nanoparticles as a next- generation drug delivery platform: state of the art, emerging technologies, and perspectives. Anubhab Mukherjee Department of Translational Neurosciences and Neurotherapeutics, John Wayne Cancer Institute, Pacific euN roscience Institute, Providence Saint John's Health Center, Santa Monica, CA Ariana K Waters Department of Translational Neurosciences and Neurotherapeutics, John Wayne Cancer Institute, Pacific euN roscience Institute, Providence Saint John's Health Center, Santa Monica, CA Pranav Kalyan Achal Singh Achrol Department of Neurosurgery and Neurosciences, John Wayne Cancer Institute and Pacific euN roscience Institute, Santa Monica, CA, USA Santosh Kesari Department of Translational Neuro-Oncology and Neurotherapeutics, John Wayne Cancer Institute at Providence Saint John's Health Center FSeoe nelloxtw pa thige fors aaddndition addal aitutionhorsal works at: https://digitalcommons.psjhealth.org/publications Part of the Oncology Commons Recommended Citation Mukherjee, Anubhab; Waters, Ariana K; Kalyan, Pranav; Achrol, Achal Singh; Kesari, Santosh; and Yenugonda, Venkata, "Lipid- polymer hybrid nanoparticles as a next-generation drug delivery platform: state of the art, emerging technologies, and perspectives." (2019). Articles, Abstracts, and Reports. 1504. https://digitalcommons.psjhealth.org/publications/1504 This Article is brought to you for free and open access by Providence St. Joseph Health Digital Commons. It has been accepted for inclusion in Articles, Abstracts, and Reports by an authorized administrator of Providence St. Joseph Health Digital Commons. For more information, please contact [email protected]. Authors Anubhab Mukherjee, Ariana K Waters, Pranav Kalyan, Achal Singh Achrol, Santosh Kesari, and Venkata Yenugonda This article is available at Providence St. -

Nanomaterials and Nanotechnology
nanomaterials and nanotechnology Collection of Selected Papers | 2013 | issn 1847-9804 © Vasil Vasilev/Shutterstock © Vasil Editor-in-Chief Paola Prete Institute for Microelectronics and Microsystems, National Research Council, Lecce, Italy Editorial Board C. N. R. Rao Fellow of the Royal Society, National Research Professor, Linus Pauling Research Professor and President of Jawaharlal Nehru Centre for Advanced Scientific Research, Bangalore, India Toshiaki Enoki Tokyo Institute of Technology, Japan Stephen O’Brien Department of Chemistry, The City College of New York, USA Juan Ramon Morante Catalonia Institute for Energy Research and University of Barcelona, Spain Stephen Pearton Department of Material Science and Engineering, University of Florida, USA Wolfgang Richter University of Rome Tor Vergata, Italy and Technischen Universität Berlin, Germany Federico Rosei Institut National de la Recherche Scientifique, Universite du Quebec, Varennes, Canada Jonathan E. Spanier Department of Materials Science and Engineering, Drexel University, Philadelphia, USA Leander Tapfer Technical Unit of Materials Technologies Brindisi, ENEA, Italy Reshef Tenne Department of Materials and Interfaces, Weizmann Institute of Science, Rehovot, Israel Fabrice Vallee CNRS and Université Claude Bernard Lyon, France Nanomater. nanotechnol., 2013, Collection of Selected Papers free online editions of InTech Books and Journals can be found at www.intechopen.com Nanomaterials and Nanotechnology Collection of Selected Papers, 2013 Abstracted/Indexed in IET Inspec, Ulrich’s Periodical Directory, Scirus, EBSCO - A-to-Z, WorldCat, BASE - Bielefeld Academic Search Engine, DOAJ - Directory of Open Access Journals, Electronic Journals Library, Google Scholar, CAS - Chemical Abstracts Service, Hrcak Published by InTech Janeza Trdine 9, 51000 Rijeka, Croatia Identification Statement Online ISSN 1847-9804 Abbreviated key title: Nanomater. -

Role of Prostaglandin E2 in Tissue Repair and Regeneration
Role of prostaglandin E2 in tissue repair and regeneration Hui Cheng1, 2, 3, Haoyan Huang1, 2, Zhikun Guo4, Ying Chang3*, Zongjin Li1,2,3, 4,5* 1Nankai University School of Medicine, Tianjin, China; 2The Key Laboratory of Bioactive Materials, Ministry of Education, Nankai University, the College of Life Sciences, Tianjin, China; 3Tianjin Key Laboratory of Human Development and Reproductive Regulation, Nankai University Affiliated Hospital of Obstetrics and Gynecology, Tianjin, China; 4Henan Key Laboratory of Medical Tissue Regeneration, Xinxiang Medical University, Xinxiang, China; 5State Key Laboratory of Kidney Diseases, Chinese PLA General Hospital, Beijing, China *Correspondence: Zongjin Li, Email: [email protected]; or Ying Chang, Email: [email protected] 1 Abstract Tissue regeneration following injury from disease or medical treatment still represents a challenge in regeneration medicine. Prostaglandin E2 (PGE2), which involves diverse physiological processes via E-type prostanoid (EP) receptor family, favors the regeneration of various organ systems following injury for its capabilities such as activation of endogenous stem cells, immune regulation, and angiogenesis. Understanding how PGE2 modulates tissue regeneration and then exploring how to elevate the regenerative efficiency of PGE2 will provide key insights into the tissue repair and regeneration processes by PGE2. In this review, we summarized the application of PGE2 to guide the regeneration of different tissues, including skin, heart, liver, kidney, intestine, bone, skeletal muscle, and hematopoietic stem cell regeneration. Moreover, we introduced PGE2-based therapeutic strategies to accelerate the recovery of impaired tissue or organs, including 15-hydroxyprostaglandin dehydrogenase (15- PGDH) inhibitors boosting endogenous PGE2 levels and biomaterial scaffolds to control PGE2 release. Keywords: Prostaglandin E2; Stem cell; Tissue repair; Regeneration; Inflammation 2 Graphical Abstract 3 1. -

(12) Patent Application Publication (10) Pub. No.: US 2007/0053845 A1 Sengupta Et Al
US 2007.0053845A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2007/0053845 A1 Sengupta et al. (43) Pub. Date: Mar. 8, 2007 (54) NANOCELL DRUG DELIVERY SYSTEM Publication Classification (76) Inventors: Shiladitya Sengupta, Waltham, MA (51) Int. Cl. (US); Ganlin Zhao, Arlington, MA A6IR 9/14 (2006.01) (US); Ishan Capila, Ashland, MA (US); A6IL 9/04 (2006.01) David Eavarone, North Quincy, MA (52) U.S. Cl. ................................................................ 424/46 (US); Ram Sasisekharan, Bedford, MA (57) ABSTRACT (US) Nanocells allow the sequential delivery of two different Correspondence Address: therapeutic agents with different modes of action or different CHOATE, HALL & STEWART LLP pharmacokinetics. A nanocell is formed by encapsulating a TWO INTERNATIONAL PLACE nanocore with a first agent inside a lipid vesicle containing BOSTON, MA 02110 (US) a second agent. The agent in the outer lipid compartment is released first and may exert its effect before the agent in the (21) Appl. No.: 11/495,947 nanocore is released. The nanocell delivery system may be formulated in pharmaceutical composition for delivery to (22) Filed: Jul. 28, 2006 patients Suffering from diseases such as cancer, inflamma tory diseases Such as asthma, autoimmune diseases such as Related U.S. Application Data rheumatoid arthritis, infectious diseases, and neurological diseases Such as epilepsy. In treating cancer, a traditional (63) Continuation-in-part of application No. 11/070,731, antineoplastic agent is contained in the outer lipid vesicle of filed on Mar. 2, 2005. the nanocell, and an antiangiogenic agent is loaded into the nanocore. This arrangement allows the antineoplastic agent (60) Provisional application No. -
Market Access Right Product, Right Patient, Tight Price, Tighter Reimbursement
invivo.pharmamedtechbi.com NOVEMBER 2016 Invol. 34 ❚ no. 10 Vivopharma intelligence ❚ informa Market Access Right product, right patient, tight price, tighter reimbursement Value Frameworks Price Transparency Real-World Evidence Outcomes-Based Reimbursement invivo.pharmamedtechbi.com CONTENTS ❚ In Vivo Pharma intelligence | November 2016 26 Curative Regenerative Medicines: Preparing Health Care Systems For The Coming Wave FARAZ ALI, TED SLOCOMB AND MICHAEL WERNER We may be at the dawn of a new era of curative regenerative therapies, but their very nature may create barriers to adoption. The Alliance for Regenerative Medicine frames the opportunities and challenges for the industry, arguing that policy makers must begin to understand THE MARKET ACCESS ISSUE the ways that these therapies represent value for money. 10 22 States Fight For Drug Price US Outcomes-Based 1 Transparency Contracts: Big Uptick In ED SILVERMAN Interest, But Not Execution California’s Proposition 61 and a number CATHY KELLY of other state-led measures to control The promise of outcomes-based drug prices failed to gain traction in contracts for biopharmaceuticals has 2016. But states are likely to remain a yet to be realized in the US. Although battleground in the war against costs in precise numbers are hard to come by, a pharma-friendly Trump administration. payers and manufacturers agree the field is still nascent. However, they 16 don’t seem to be giving up on the idea. Is The UK Still Open 34 For Medtech Innovation Reimbursement? Real-World Evidence ASHLEY YEO And The Quest For Confusing and ineffective channels of European Market Access innovation adoption and a lack of FRANcescA BRUce funding hamper the UK’s reputation as Real-world evidence promises to solve one of the world’s health care capitals many problems inherent in getting a and a driver of care excellence – in spite drug to patients at a good price. -

(12) Patent Application Publication (10) Pub. No.: US 2016/0146783 A1 CHERESH Et Al
US 2016O146783A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2016/0146783 A1 CHERESH et al. (43) Pub. Date: May 26, 2016 (54) COMPOSITIONS AND METHODS FOR Publication Classification TREATING CANCER AND DISEASES AND CONDITIONS RESPONSIVE TO CELL (51) Int. C. GROWTH INHIBITION GOIN33/50 (2006.01) (52) U.S. C. (71) Applicant: THE REGENTS OF THE CPC. G0IN33/5011 (2013.01); G0IN 2333/4724 UNIVERSITY OF CALIFORNLA, (2013.01); G0IN 2333/70557 (2013.01) Oakland, CA (US) (57) ABSTRACT (72) Inventors: David CHERESH, Encinitas, CA (US); In alternative embodiments, the invention provides composi Laetitia SEGUIN, San Diego, CA (US); tions and methods for overcoming or diminishing or prevent Sudarshan ANAND, San Diego, CA ing Growth Factor Inhibitor resistance in a cell, or, a method (US) for increasing the growth-inhibiting effectiveness of a Growth Factor inhibitor on a cell, or, a method for re-sensi (21) Appl. No.: 14/883,398 tizing a cell to a Growth Factor Inhibitor, comprising for example, administration of a combination of a TBK1 inhibi tor and an RTK inhibitor. In alternative embodiments, the cell (22) Filed: Oct. 14, 2015 is a tumor cell, a cancer cell or a dysfunctional cell. In alter native embodiments, the invention provides compositions Related U.S. Application Data and methods for determining: whether an individual or a patient would benefit from or respond to administration of a (63) Continuation of application No. 14/325,288, filed on Growth Factor Inhibitor, or, which individuals or patients Jul. 7, 2014, which is a continuation-in-part of appli would benefit from a combinatorial approach comprising cation No. -

New Trends in Bio-Based Aerogels
pharmaceutics Review New Trends in Bio-Based Aerogels Loredana Elena Nita, Alina Ghilan, Alina Gabriela Rusu, Iordana Neamtu and Aurica P. Chiriac * “Petru Poni” Institute of Macromolecular Chemistry, Grigore Ghica Voda Alley 41-A, RO-700487 Iasi, Romania; [email protected] (L.E.N.); [email protected] (A.G.); [email protected] (A.G.R.); [email protected] (I.N.) * Correspondence: [email protected]; Tel.: +40-232-454417 Received: 6 April 2020; Accepted: 11 May 2020; Published: 13 May 2020 Abstract: (1) Background: The fascinating properties of currently synthesized aerogels associated with the flexible approach of sol-gel chemistry play an important role in the emergence of special biomedical applications. Although it is increasingly known and mentioned, the potential of aerogels in the medical field is not sufficiently explored. Interest in aerogels has increased greatly in recent decades due to their special properties, such as high surface area, excellent thermal and acoustic properties, low density and thermal conductivity, high porosity, flame resistance and humidity, and low refractive index and dielectric constant. On the other hand, high manufacturing costs and poor mechanical strength limit the growth of the market. (2) Results: In this paper, we analyze more than 180 articles from recent literature studies focused on the dynamics of aerogels research to summarize the technologies used in manufacturing and the properties of materials based on natural polymers from renewable sources. Biomedical applications of these bio-based materials are also introduced. (3) Conclusions: Due to their complementary functionalities (bioactivity, biocompatibility, biodegradability, and unique chemistry), bio-based materials provide a vast capability for utilization in the field of interdisciplinary and multidisciplinary scientific research. -

What's Inside
Newsletter A publication of the Controlled Release Society Volume 34 • Number 2 • 2017 What’s Inside Formulation and Delivery of Mono-N-Oxide Vinblastine Liposomal Formulation for Targeting Non-Small Cell Lung Cancer with Hypoxic Environments In Vitro and In Vivo Evaluation of Controlled Payload Release Using Acoustically Responsive Scaffolds CRS Annual Meeting DDTR Update Science. People. Products. Connect and collaborate with delivery science and technology leaders from academia and industry, under one roof at #CRSboston Join us in Boston, Massachusetts, U.S.A. from July 16–19 for the 2017 Controlled Release Society Annual Meeting & Exposition. Registration is now open! Visit controlledreleasesociety.org/CRSboston for details. 2 Newsletter Ryan Donnelly Vol. 34 • No. 2 • 2017 Editor > TABLE OF CONTENTS 4 From the Editor 5 2017 Controlled Release Society Annual Meeting & Exposition Steven Giannos 7 Scientifically Speaking Editor Formulation and Delivery of Mono-N-Oxide Vinblastine Liposomal Formulation for Targeting Non-Small Cell Lung Cancer with Hypoxic Environments 10 Scientifically Speaking In Vitro and In Vivo Evaluation of Controlled Payload Release Using Acoustically Responsive Scaffolds 13 DDTR Update Drug Delivery and Translational Research Update Medha Joshi Editor 14 People in the News 15 Companies in the News Cover image: Malignant effusion: Pleural fluid cytology of lung (pulmonary) papillary adenocarcinoma, a type of non small cell carcinoma. Pap stain. David Litman / Shutterstock.com Arlene McDowell Editor Bozena Michniak-Kohn Editor Rod Walker Editor 3 > FROM THE EDITOR Editors Ryan Donnelly Steven Giannos Steven Giannos Medha Joshi University of Texas Medical Branch Arlene McDowell Galveston, TX, U.S.A. Bozena Michniak-Kohn Rod Walker The CRS Newsletter is the official Please Come to Boston newsletter of the Controlled Release Society.