Anesthesia Cross Coder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Urological Trauma
Guidelines on Urological Trauma D. Lynch, L. Martinez-Piñeiro, E. Plas, E. Serafetinidis, L. Turkeri, R. Santucci, M. Hohenfellner © European Association of Urology 2007 TABLE OF CONTENTS PAGE 1. RENAL TRAUMA 5 1.1 Background 5 1.2 Mode of injury 5 1.2.1 Injury classification 5 1.3 Diagnosis: initial emergency assessment 6 1.3.1 History and physical examination 6 1.3.1.1 Guidelines on history and physical examination 7 1.3.2 Laboratory evaluation 7 1.3.2.1 Guidelines on laboratory evaluation 7 1.3.3 Imaging: criteria for radiographic assessment in adults 7 1.3.3.1 Ultrasonography 7 1.3.3.2 Standard intravenous pyelography (IVP) 8 1.3.3.3 One shot intraoperative intravenous pyelography (IVP) 8 1.3.3.4 Computed tomography (CT) 8 1.3.3.5 Magnetic resonance imaging (MRI) 9 1.3.3.6 Angiography 9 1.3.3.7 Radionuclide scans 9 1.3.3.8 Guidelines on radiographic assessment 9 1.4 Treatment 10 1.4.1 Indications for renal exploration 10 1.4.2 Operative findings and reconstruction 10 1.4.3 Non-operative management of renal injuries 11 1.4.4 Guidelines on management of renal trauma 11 1.4.5 Post-operative care and follow-up 11 1.4.5.1 Guidelines on post-operative management and follow-up 12 1.4.6 Complications 12 1.4.6.1 Guidelines on management of complications 12 1.4.7 Paediatric renal trauma 12 1.4.7.1 Guidelines on management of paediatric trauma 13 1.4.8 Renal injury in the polytrauma patient 13 1.4.8.1 Guidelines on management of polytrauma with associated renal injury 14 1.5 Suggestions for future research studies 14 1.6 Algorithms 14 1.7 References 17 2. -

Urology Services in the ASC
Urology Services in the ASC Brad D. Lerner, MD, FACS, CASC Medical Director Summit ASC President of Chesapeake Urology Associates Chief of Urology Union Memorial Hospital Urologic Consultant NFL Baltimore Ravens Learning Objectives: Describe the numerous basic and advanced urology cases/lines of service that can be provided in an ASC setting Discuss various opportunities regarding clinical, operational and financial aspects of urology lines of service in an ASC setting Why Offer Urology Services in Your ASC? Majority of urologic surgical services are already outpatient Many urologic procedures are high volume, short duration and low cost Increasing emphasis on movement of site of service for surgical cases from hospitals and insurance carriers to ASCs There are still some case types where patients are traditionally admitted or placed in extended recovery status that can be converted to strictly outpatient status and would be suitable for an ASC Potential core of fee-for-service case types (microsurgery, aesthetics, prosthetics, etc.) Increasing Population of Those Aged 65 and Over As of 2018, it was estimated that there were 51 million persons aged 65 and over (15.63% of total population) By 2030, it is expected that there will be 72.1 million persons aged 65 and over National ASC Statistics - 2017 Urology cases represented 6% of total case mix for ASCs Urology cases were 4th in median net revenue per case (approximately $2,400) – behind Orthopedics, ENT and Podiatry Urology comprised 3% of single specialty ASCs (5th behind -

Nuclear Medicine for Medical Students and Junior Doctors
NUCLEAR MEDICINE FOR MEDICAL STUDENTS AND JUNIOR DOCTORS Dr JOHN W FRANK M.Sc, FRCP, FRCR, FBIR PAST PRESIDENT, BRITISH NUCLEAR MEDICINE SOCIETY DEPARTMENT OF NUCLEAR MEDICINE, 1ST MEDICAL FACULTY, CHARLES UNIVERSITY, PRAGUE 2009 [1] ACKNOWLEDGEMENTS I would very much like to thank Prof Martin Šámal, Head of Department, for proposing this project, and the following colleagues for generously providing images and illustrations. Dr Sally Barrington, Dept of Nuclear Medicine, St Thomas’s Hospital, London Professor Otakar Bělohlávek, PET Centre, Na Homolce Hospital, Prague Dr Gary Cook, Dept of Nuclear Medicine, Royal Marsden Hospital, London Professor Greg Daniel, formerly at Dept of Veterinary Medicine, University of Tennessee, currently at Virginia Polytechnic Institute and State University (Virginia Tech), Past President, American College of Veterinary Radiology Dr Andrew Hilson, Dept of Nuclear Medicine, Royal Free Hospital, London, Past President, British Nuclear Medicine Society Dr Iva Kantorová, PET Centre, Na Homolce Hospital, Prague Dr Paul Kemp, Dept of Nuclear Medicine, Southampton University Hospital Dr Jozef Kubinyi, Institute of Nuclear Medicine, 1st Medical Faculty, Charles University Dr Tom Nunan, Dept of Nuclear Medicine, St Thomas’s Hospital, London Dr Kathelijne Peremans, Dept of Veterinary Medicine, University of Ghent Dr Teresa Szyszko, Dept of Nuclear Medicine, St Thomas’s Hospital, London Ms Wendy Wallis, Dept of Nuclear Medicine, Charing Cross Hospital, London Copyright notice The complete text and illustrations are copyright to the author, and this will be strictly enforced. Students, both undergraduate and postgraduate, may print one copy only for personal use. Any quotations from the text must be fully acknowledged. It is forbidden to incorporate any of the illustrations or diagrams into any other work, whether printed, electronic or for oral presentation. -
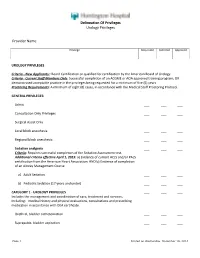
Delineation of Privileges Urology Privileges Provider Name
Delineation Of Privileges Urology Privileges Provider Name: Privilege Requested Deferred Approved UROLOGY PRIVILEGES Criteria - New Applicants:: Board Certification or qualified for certification by the American Board of Urology. Criteria - Current Staff Members Only: Successful completion of an ACGME or AOA approved training program; OR demonstrated acceptable practice in the privileges being requested for a minimum of five (5) years. Proctoring Requirements: A minimum of eight (8) cases, in accordance with the Medical Staff Proctoring Protocol. GENERAL PRIVILEGES: Admit ___ ___ ___ Consultation Only Privileges ___ ___ ___ Surgical Assist Only ___ ___ ___ Local block anesthesia ___ ___ ___ Regional block anesthesia ___ ___ ___ Sedation analgesia ___ ___ ___ Criteria: Requires successful completion of the Sedation Assessment test. Additional criteria effective April 1, 2015: a) Evidence of current ACLS and/or PALS certification from the American Heart Association; AND b) Evidence of completion of an Airway Management Course a) Adult Sedation ___ ___ ___ b) Pediatric Sedation (17 years and under) ___ ___ ___ CATEGORY 1 - UROLOGY PRIVILEGES ___ ___ ___ Includes the management and coordination of care, treatment and services, including: medical history and physical evaluations, consultations and prescribing medication in accordance with DEA certificate. Urethral, bladder catheterization ___ ___ ___ Suprapubic, bladder aspiration ___ ___ ___ Page 1 Printed on Wednesday, December 10, 2014 Delineation Of Privileges Urology Privileges Provider -

A Systematic Review of Graft Augmentation Urethroplasty Techniques for the Treatment of Anterior Urethral Strictures
EUROPEAN UROLOGY 59 (2011) 797–814 available at www.sciencedirect.com journal homepage: www.europeanurology.com Review – Reconstructive Urology A Systematic Review of Graft Augmentation Urethroplasty Techniques for the Treatment of Anterior Urethral Strictures Altaf Mangera *, Jacob M. Patterson, Christopher R. Chapple Royal Hallamshire Hospital, Sheffield, United Kingdom Article info Abstract Article history: Context: Reconstructive surgeons who perform urethroplasty have a variety of Accepted February 2, 2011 techniques in their armamentarium that may be used according to factors such as Published online ahead of aetiology, stricture position, and length. No one technique is recommended. print on February 11, 2011 Objective: Our aim was to assess the reported outcomes of the various techniques for graft augmentation urethroplasty according to site of surgery. Keywords: Evidence acquisition: We performed an updated systematic review of the Medline Augmentation urethroplasty literature from 1985 to date and classified the data according to the site of surgery Anterior urethral stricture and technique used. Data are also presented on the type of graft used and the Bulbar urethroplasty follow-up methodology used by each centre. Dorsal onlay bulbar Evidence synthesis: More than 2000 anterior urethroplasty procedures have been urethroplasty describedinthe literature.Whenconsidering the bulbar urethra there isnosignificant Ventral onlay bulbar difference between the average success rates of the dorsal and the ventral onlay urethroplasty procedures, 88.4% and 88.8% at42.2 and 34.4 moin 934 and 563 patients,respectively. Penile urethroplasty The lateral onlay technique has only been described in six patients and has a reported success rate of 83% at 77 mo. The Asopa and Palminteri techniques have been described in 89 and 53 patients with a success rate of 86.7% and 90.1% at 28.9 and 21.9 mo, respectively. -

Nuclear Pharmacy Quick Sample
12614-01_CH01-rev3.qxd 10/25/11 10:56 AM Page 1 CHAPTER 1 Radioisotopes Distribution for Not 1 12614-01_CH01-rev3.qxd 10/25/1110:56AMPage2 2 N TABLE 1-1 Radiopharmaceuticals Used in Nuclear Medicine UCLEAR Chemical Form and Typical Dosage P Distribution a b HARMACY Radionuclide Dosage Form Use (Adult ) Route Carbon C 11 Carbon monoxide Cardiac: Blood volume measurement 60–100 mCi Inhalation Carbon C 11 Flumazenil injection Brain: Benzodiazepine receptor imaging 20–30 mCi IV Q UICK Carbon C 11 Methionine injection Neoplastic disease evaluation in brain 10–20 mCi IV R Carbon C 11 forRaclopride injection Brain: Dopamine D2 receptor imaging 10–15 mCi IV EFERENCE Carbon C 11 Sodium acetate injection Cardiac: Marker of oxidative metabolism 12–40 mCi IV Carbon C 14 Urea Diagnosis of Helicobacter pylori infection 1 µCi PO Chromium Cr 51 Sodium chromate injection Labeling red blood cells (RBCs) for mea- 10–80 µCi IV suring RBC volume, survival, and splenic sequestration Cobalt Co 57 Cyanocobalamin capsules Diagnosis of pernicious anemia and 0.5 µCi PO Not defects of intestinal absorption Fluorine F 18 Fludeoxyglucose injection Glucose utilization in brain, cardiac, and 10–15 mCi IV neoplastic disease Fluorine F 18 Fluorodopa injection Dopamine neuronal decarboxylase activity 4–6 mCi IV in brain Fluorine F 18 Sodium fluoride injection Bone imaging 10 mCi IV Gallium Ga 67 Gallium citrate injection Hodgkin’s disease, lymphoma 8–10 mCi IV Acute inflammatory lesions 5 mCi IV Indium In 111 Capromab pendetide Metastatic imaging in patients with biopsy- -

General Catalogue GENERAL CATALOGUE
Coloplast develops products and services that make life easier for people with very personal and private medical conditions. Working closely with the people who use our products, we create solutions that are sensitive to their special needs. We call this intimate healthcare. Our business includes ostomy care, urology and continence care, wound and skin care. & Gynaecology Urology We operate globally and employ more than 10 000 employees. General Catalogue GENERAL CATALOGUE Urology & Gynaecology The Coloplast logo and Porgès logo are registered trademarks of Coloplast A/S. © [2016- 05.] All rights reserved. Coloplast A/S, 3050 Humlebaek, Denmark. 2016 - 000NGLOBALCATEN01 INTRODUCTION Introduction With a world class innovative spirit and the ultimate objective of always being able to make your life easier, Coloplast presents its latest dedicated Urology Care catalogue including all of our disposables and implants for urology and gynaecology. For over 120 years, we have supported the medical progress through the development of the latest techniques and devices in co-operation with our leading surgeon partners. Our know-how and high quality industrial processes permit us to offer you medical materials of the very highest standards with worldwide recognition and expertise. Within this catalogue you will find all of the latest products you will need for your daily operating practice: • Endourology : A wide range of disposable products for stone management like Dormia stone extractors, Ureteral stents, Access sheath (Retrace) and guidewires. We have extended our line with a new innovative digital solution to remove ureteral stents in one step: ISIRIS α . The product is a combination between a single use flexible cystoscope with an integrated grasper and a reusable portable device • Female Pelvic Health: slings (Altis, Aris), and lightweight meshes (Restorelle), to treat stress urinary incontinence and pelvic organ prolapses. -
Radical Cystectomy and Cutaneous Ureterostomy in 4 Dogs with Trigonal Transitional Cell Carcinoma: Description of Technique and Case Series
Received: 15 July 2015 | Accepted: 18 June 2016 DOI 10.1111/vsu.12583 ORIGINAL ARTICLE Radical Cystectomy and Cutaneous Ureterostomy in 4 Dogs with Trigonal Transitional Cell Carcinoma: Description of Technique and Case Series Rafael Ricardo Huppes1 | Leandro Z. Crivellenti2,3 | Andrigo Barboza De Nardi3 | Bruno Roque Lima4 | Cristiane Alves Cintra2 | Jorge Luiz Costa Castro5 | Christopher A. Adin6 1 Department of Veterinary Clinic and Abstract Surgery, Faculdade Uninga, Maringa, Brazil Objective: To describe radical cystectomy followed by cutaneous ureterostomy as a 2 Department of Veterinary Clinic and treatment of invasive bladder neoplasia in dogs. Surgery, Franca University Study Design: Retrospective study. (UNIFRAN), Franca, Brazil Animals: Client-owned dogs with transitional cell carcinoma of the bladder trigone 3 Department of Veterinary Clinic and (n54). Surgery, S~ao Paulo State University, Jaboticabal, Brazil Methods: Perioperative complications and long-term outcomes of dogs that under- 4 went cutaneous ureterostomy following radical cystectomy and lymphadenectomy Veterinary College, Universidade Unimontes, Santos, Brazil for transitional cell carcinoma of the urinary bladder trigone were reviewed. Both ure- ters were transected and anastomosed to the ventral abdominal skin. Polyvinyl 5 Veterinary College, Pontifícia chloride catheters were placed in the ureteral stomas and maintained for 5 days. After Universidade Catolica do Parana, catheter removal, dogs were managed with an absorbent diaper over the stomas. Curitiba, Brazil Long-term outcome and survival were documented by follow-up visits or phone 6 Department of Clinical Sciences, contact. College of Veterinary Medicine, North Carolina State University, Results: Median age at the time of surgery was 10.3 years (range, 8–12). Average Raleigh, North Carolina procedural time was 4.7 hours (range, 3.8–6.1). -

(Part 1): Management of Male Urethral Stricture Disease
EURURO-9412; No. of Pages 11 E U R O P E A N U R O L O G Y X X X ( 2 0 2 1 ) X X X – X X X ava ilable at www.sciencedirect.com journa l homepage: www.europeanurology.com Review – Reconstructive Urology European Association of Urology Guidelines on Urethral Stricture Disease (Part 1): Management of Male Urethral Stricture Disease a, b c d Nicolaas Lumen *, Felix Campos-Juanatey , Tamsin Greenwell , Francisco E. Martins , e f a c g Nadir I. Osman , Silke Riechardt , Marjan Waterloos , Rachel Barratt , Garson Chan , h i a j Francesco Esperto , Achilles Ploumidis , Wesley Verla , Konstantinos Dimitropoulos a b Division of Urology, Gent University Hospital, Gent, Belgium; Urology Department, Marques de Valdecilla University Hospital, Santander, Spain; c d Department of Urology, University College London Hospital, London, UK; Department of Urology, Santa Maria University Hospital, University of Lisbon, e f Lisbon, Portugal; Department of Urology, Sheffield Teaching Hospitals, Sheffield, UK; Department of Urology, University Medical Center Hamburg- g h Eppendorf, Hamburg, Germany; Division of Urology, University of Saskatchewan, Saskatoon, Canada; Department of Urology, Campus Biomedico i j University of Rome, Rome, Italy; Department of Urology, Athens Medical Centre, Athens, Greece; Aberdeen Royal Infirmary, Aberdeen, UK Article info Abstract Article history: Objective: To present a summary of the 2021 version of the European Association of Urology (EAU) guidelines on management of male urethral stricture disease. Accepted May 15, 2021 Evidence acquisition: The panel performed a literature review on these topics covering a time frame between 2008 and 2018, and used predefined inclusion and exclusion criteria Associate Editor: for the literature to be selected. -

Outcomes of Urethroplasty to Treat Urethral Strictures Arising from Artificial Urinary Sphincter Erosions and Rates of Subsequent Device Replacement
UCSF UC San Francisco Previously Published Works Title Outcomes of Urethroplasty to Treat Urethral Strictures Arising From Artificial Urinary Sphincter Erosions and Rates of Subsequent Device Replacement. Permalink https://escholarship.org/uc/item/4sk1p5g1 Authors Keihani, Sorena Chandrapal, Jason C Peterson, Andrew C et al. Publication Date 2017-09-01 DOI 10.1016/j.urology.2017.05.049 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Reconstructive Urology Outcomes of Urethroplasty to Treat Urethral Strictures Arising From Artificial Urinary Sphincter Erosions and Rates of Subsequent Device Replacement Sorena Keihani, Jason C. Chandrapal, Andrew C. Peterson, Joshua A. Broghammer, Nathan Chertack, Sean P. Elliott, Keith F. Rourke, Nejd F. Alsikafi, Jill C. Buckley, Benjamin N. Breyer, Thomas G. Smith III, Bryan B. Voelzke, Lee C. Zhao, William O. Brant, and Jeremy B. Myers, for the Trauma and Urologic Reconstruction Network of Surgeons (TURNS, TURNSresearch.org) OBJECTIVE To evaluate the success of urethroplasty for urethral strictures arising after erosion of an artificial urinary sphincter (AUS) and rates of subsequent AUS replacement. PATIENTS AND From 2009-2016, we identified patients from the Trauma and Urologic Reconstruction Network METHODS of Surgeons and several other centers. We included patients with urethral strictures arising from AUS erosion undergoing urethroplasty with or without subsequent AUS replacement. We ret- rospectively reviewed patient demographics, history, stricture characteristics, and outcomes. Vari- ables in patients with and without complications after AUS replacement were compared using chi-square test, independent samples t test, and Mann-Whitney U test when appropriate. RESULTS Thirty-one men were identified with the inclusion criteria. -

The Basics of a Radical Cystectomy and Ileal Conduits Dr. Alexander Kutikov
The Basics of A Radical Cystectomy and Ileal Conduits Dr. Alexander Kutikov: But we're here to really talk about cystectomy, and let's talk a little bit about anatomy. This is what's called the retroperitoneum, which is a fancy word for the organs that live behind the bowel sack. This is kind of the anatomy that we're used to seeing, and this lives behind it. These are the kidneys. These are the ureters, the tubes that go from the kidneys to the bladder. This is the bladder, and this is the prostate in the male. We'll talk about female urological anatomy in a minute. The inner lining of the bladder is the same as the inner lining of the ureters and the same as the inner lining of the kidneys. When we talk about urothelial carcinoma, which is basically the main type of cancer that bladder cancer patients have, that is the same lining that lines the ureters and the kidneys. So patients with bladder cancer are at risk of developing tumors along their ureters and inside of the kidney. It's very important for those people that are being monitored for bladder cancer, whether they had or didn't have a cystectomy, is to have routine imaging of their upper tract. The upper tract, we basically call the kidneys and the ureters. These blue and red pipes are the great vessels. This is the aorta that brings blood away from the heart and goes down to the legs. The blue are the veins. This is the iliac veins and the vena cava. -

And Long-Term Evaluation of Renal Function After Radical Cystectomy and Cutaneous Ureterostomy in High-Risk Patients
Journal of Clinical Medicine Article Short- and Long-Term Evaluation of Renal Function after Radical Cystectomy and Cutaneous Ureterostomy in High-Risk Patients Massimiliano Creta 1,*, Ferdinando Fusco 2, Roberto La Rocca 1, Marco Capece 1 , Giuseppe Celentano 1, Ciro Imbimbo 1, Vittorio Imperatore 3, Luigi Russo 4, Francesco Mangiapia 1, Vincenzo Mirone 1, Domenico Russo 5 and Nicola Longo 1 1 Urologic Section, Department of Neurosciences, Sciences of Reproduction, and Odontostomatology, University of Naples Federico II, 80131 Naples, Italy; [email protected] (R.L.R.); [email protected] (M.C.); [email protected] (G.C.); [email protected] (C.I.); [email protected] (F.M.); [email protected] (V.M.); [email protected] (N.L.) 2 Department of Urology, Luigi Vanvitelli University of Naples, 80131 Naples, Italy; [email protected] 3 Urology Unit, Buon Consiglio Fatebenefratelli Hospital, 80123 Naples, Italy; [email protected] 4 Nephrology Unit, Ospedale del Mare; 80131 Naples, Italy; [email protected] 5 Nephrology Unit, Department of Public Health; University of Naples Federico II, 80131 Naples, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-08-1746-2611; Fax: +39-08-1545-2959 Received: 24 April 2020; Accepted: 8 July 2020; Published: 11 July 2020 Abstract: Deterioration of renal function has been reported after radical cystectomy (RC) with urinary diversion. We investigated renal function changes in elderly bladder cancer (BCa) patients who underwent RC with cutaneous ureterostomy (CU) urinary diversion. We performed a retrospective, observational study. BCa patients aged 75 with an American Society of Anesthesiologists (ASA) ≥ class greater than II were included.