Variations in Terminal Branches of the Popliteal Artery: Cadaveric Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Classification System of the Tibiofibular Syndesmosis Blood Supply and Its
www.nature.com/scientificreports OPEN Classifcation system of the tibiofbular syndesmosis blood supply and its clinical relevance Received: 16 February 2018 Izabela Mróz1, Piotr J. Bachul1,2, Krzysztof A. Tomaszewski1, Tomasz Bereza1, Krzysztof Gil3, Accepted: 7 June 2018 Jerzy A. Walocha1 & Artur Pasternak 1 Published: xx xx xxxx Due to the lack of anatomical studies concerning complexity of the tibiofbular syndesmosis blood supply, density of blood vessels with further organization of syndesmotic vascular variations is presented in clinically relevant classifcation system. The material for the study was obtained from cadaveric dissections. We dissected 50 human ankles observing diferent types of arterial blood supply. Our classifcation system is based on the vascular variations of the anterior aspect of tibiofbular syndesmosis and corresponds with vascular density. According to our study the mean vascular density of tibiofbular syndesmosis is relatively low (4.4%) and depends on the type of blood supply. The highest density was observed among ankles with complete vasculature and the lowest when lateral anterior malleolar artery was absent (5.8% vs. 3.5%, respectively). Awareness of various types of tibiofbular syndesmosis arterial blood supply is essential for orthopedic surgeons who operate in the ankle region and radiologists for the anatomic evaluation of this area. Knowledge about possible variations along with relatively low density of vessels may contribute to modifcation of treatment approach by the increase of the recommended time of syndesmotic screw stabilization in order to prevent healing complications. Tibiofbular syndesmosis is a fbrous connection localized between the fbular notch of the tibia and medial surface of the lateral ankle. -

Vessels and Circulation
CARDIOVASCULAR SYSTEM OUTLINE 23.1 Anatomy of Blood Vessels 684 23.1a Blood Vessel Tunics 684 23.1b Arteries 685 23.1c Capillaries 688 23 23.1d Veins 689 23.2 Blood Pressure 691 23.3 Systemic Circulation 692 Vessels and 23.3a General Arterial Flow Out of the Heart 693 23.3b General Venous Return to the Heart 693 23.3c Blood Flow Through the Head and Neck 693 23.3d Blood Flow Through the Thoracic and Abdominal Walls 697 23.3e Blood Flow Through the Thoracic Organs 700 Circulation 23.3f Blood Flow Through the Gastrointestinal Tract 701 23.3g Blood Flow Through the Posterior Abdominal Organs, Pelvis, and Perineum 705 23.3h Blood Flow Through the Upper Limb 705 23.3i Blood Flow Through the Lower Limb 709 23.4 Pulmonary Circulation 712 23.5 Review of Heart, Systemic, and Pulmonary Circulation 714 23.6 Aging and the Cardiovascular System 715 23.7 Blood Vessel Development 716 23.7a Artery Development 716 23.7b Vein Development 717 23.7c Comparison of Fetal and Postnatal Circulation 718 MODULE 9: CARDIOVASCULAR SYSTEM mck78097_ch23_683-723.indd 683 2/14/11 4:31 PM 684 Chapter Twenty-Three Vessels and Circulation lood vessels are analogous to highways—they are an efficient larger as they merge and come closer to the heart. The site where B mode of transport for oxygen, carbon dioxide, nutrients, hor- two or more arteries (or two or more veins) converge to supply the mones, and waste products to and from body tissues. The heart is same body region is called an anastomosis (ă-nas ′tō -mō′ sis; pl., the mechanical pump that propels the blood through the vessels. -

Vascular Anatomy of the Free Fibula Flap Including the Lateral Head of the Soleus Muscle Applied to Maxillo-Mandibular Reconstruction
Surgical and Radiologic Anatomy (2019) 41:447–454 https://doi.org/10.1007/s00276-018-2166-2 ORIGINAL ARTICLE Vascular anatomy of the free fibula flap including the lateral head of the soleus muscle applied to maxillo-mandibular reconstruction Lara Nokovitch1,2 · Julien Davrou2 · François Bidault4 · Bernard Devauchelle2 · Stéphanie Dakpé2 · Christian Vacher3,5 Received: 1 May 2018 / Accepted: 8 December 2018 / Published online: 14 December 2018 © Springer-Verlag France SAS, part of Springer Nature 2018 Abstract Purpose Initially described by Baudet in 1982, the fibula flap including the lateral head of the soleus muscle allows a one- stage reconstruction for large maxillo-mandibular defects. The aim of this study was to evaluate the number of muscular branches destined to the soleus muscle and their distance from the origin of the fibular artery, to assess the vascular anatomy of the free fibula flap including the lateral head of the soleus muscle applied to maxillo-mandibular reconstruction. Methods We performed a cadaveric anatomic study on ten lower limbs, and a CT angiography anatomic study on 38 legs. The number of soleus branches originating from the fibular artery, and the distance between the origin of the fibular artery and each of the identified branches were measured. Results The number of soleus branches destined to the lateral head of the soleus muscle is variable, with in our study 1–3 branches found. Soleus branches destined to the lateral head of the soleus muscle emerged at a distance ranging between 0 and 2.9 cm (mean value = 1.82 cm) from the origin of the fibular artery in 40% of cases, between 3 and 5.9 cm (mean value = 4.27 cm) from the origin of the fibular artery in 37% of cases, and was at a distance of 6 cm or more (mean value = 6.93 cm) from the origin of the fibular artery in 20% of cases. -
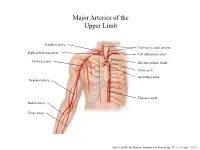
Major Arteries of the Upper Limb
Major Arteries of the Upper Limb Vertebral artery Common carotid arteries Right subclavian artery Left subclavian artery Axillary artery Brachiocephalic trunk Aortic arch Ascending aorta Brachial artery Thoracic aorta Radial artery Ulnar artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.23 Major Arteries of the Abdominal Region Renal artery Celiac trunk Abdominal aorta Superior mesenteric artery Gonadal artery Inferior mesenteric artery Common iliac artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.24 Common iliac artery Internal iliac artery Major Arteries of the External iliac artery Lower Limb Femoral artery Popliteal artery Anterior tibial artery Fibular artery Posterior tibial artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.25 Major Veins of the Upper Limb Internal jugular vein (left) Subclavian vein (right) External jugular vein (left) Axillary vein Brachiocephalic veins Cephalic vein Superior vena cava Brachial vein Basilic vein Median cubital vein Inferior vena cava Radial vein Ulnar vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.28 Major Veins of the Abdominal Cavity – Part 1 Hepatic veins Inferior vena cava Renal vein (left) Gonadal vein (left) Gonadal vein (right) Common iliac vein (left) Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Major Veins of the Abdominal Cavity – Part 2 (Hepatic portal circulation) Hepatic portal vein Splenic vein Inferior mesenteric vein Superior mesenteric vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Common iliac vein (left) Internal iliac vein Major Veins of the External iliac vein Lower Limb Great saphenous vein Femoral vein Popliteal vein Fibular vein Small saphenous vein Anterior tibial Posterior tibial vein vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.30 . -

Clinical Anatomy of the Lower Extremity
Государственное бюджетное образовательное учреждение высшего профессионального образования «Иркутский государственный медицинский университет» Министерства здравоохранения Российской Федерации Department of Operative Surgery and Topographic Anatomy Clinical anatomy of the lower extremity Teaching aid Иркутск ИГМУ 2016 УДК [617.58 + 611.728](075.8) ББК 54.578.4я73. К 49 Recommended by faculty methodological council of medical department of SBEI HE ISMU The Ministry of Health of The Russian Federation as a training manual for independent work of foreign students from medical faculty, faculty of pediatrics, faculty of dentistry, protocol № 01.02.2016. Authors: G.I. Songolov - associate professor, Head of Department of Operative Surgery and Topographic Anatomy, PhD, MD SBEI HE ISMU The Ministry of Health of The Russian Federation. O. P.Galeeva - associate professor of Department of Operative Surgery and Topographic Anatomy, MD, PhD SBEI HE ISMU The Ministry of Health of The Russian Federation. A.A. Yudin - assistant of department of Operative Surgery and Topographic Anatomy SBEI HE ISMU The Ministry of Health of The Russian Federation. S. N. Redkov – assistant of department of Operative Surgery and Topographic Anatomy SBEI HE ISMU THE Ministry of Health of The Russian Federation. Reviewers: E.V. Gvildis - head of department of foreign languages with the course of the Latin and Russian as foreign languages of SBEI HE ISMU The Ministry of Health of The Russian Federation, PhD, L.V. Sorokina - associate Professor of Department of Anesthesiology and Reanimation at ISMU, PhD, MD Songolov G.I K49 Clinical anatomy of lower extremity: teaching aid / Songolov G.I, Galeeva O.P, Redkov S.N, Yudin, A.A.; State budget educational institution of higher education of the Ministry of Health and Social Development of the Russian Federation; "Irkutsk State Medical University" of the Ministry of Health and Social Development of the Russian Federation Irkutsk ISMU, 2016, 45 p. -
Beyond Common Femoral Artery Access Exploring a Combined Approach for Treatment of Critical Limb Ischemia
BTK DISEASE Hybrid Procedures for CLI: Beyond Common Femoral Artery Access Exploring a combined approach for treatment of critical limb ischemia. By Jos C. van den Berg, MD, PhD atients with end-stage peripheral artery disease In cases of multilevel disease, the decision on how to typically demonstrate multilevel disease that can combine the three major treatment arms (endovas- extend from the aorta to the infragenicular arter- cular treatment, bypass surgery, and endarterectomy) ies. An evaluation of the lesion location (iliac, fem- should be made based on target lesion complexity Poropopliteal, or infrapopliteal segment) in patients who as well as the underlying condition.5 A hybrid proce- presented with critical limb ischemia (CLI) demonstrated dure can reduce the perioperative risk, especially in that the large majority has involvement of at least two older patients. Distal revascularization in patients with arterial segments.1 The lesion distribution combined with Rutherford category 5 and TASC D lesions, as well as in the concomitant comorbidities have implications for patients with major tissue loss will lead to better limb subsequent treatment, and oftentimes, a pure endovas- salvage, reintervention, and survival rates.6 The major- cular or open surgical procedure is not feasible. To treat ity of reports on the use of hybrid procedures involves the patient with complex multilevel disease in a single simultaneous treatment with endovascular treatment intervention that can provide an extensive revasculariza- of the aortoiliac segment -

Arteries of the Lower Limb
BLOOD SUPPLY OF LOWER LIMB Ali Fırat Esmer, MD Ankara University Faculty of Medicine Department of Anatomy Abdominal aorta Aortic bifurcation Right common iliac artery Left common iliac artery Right external Left external iliac artery iliac artery Rigt and left internal iliac arteries GLUTEAL REGION Structures passing through the suprapriform foramen Superior gluteal artery and vein Superior gluteal nerve Structures passing through the infrapriform foramen Inferior gluteal artery and vein Inferior gluteal nerve Sciatic nerve Posterior femoral cutaneous nerve Internal pudendal artery and vein Pudendal nerve • Femoral artery is the principal artery of the lower limb • Femoral artery is the continuation of the external iliac artery • External iliac artery becomes the femoral artery as it passes posterior to the inguinal ligament • Femoral artery, first enters the femoral triangle. Leaving the tirangle it passes through the adductor canal and then adductor hiatus and reaches to the popliteal fossa, where it becomes the popliteal artery Contents of the femoral triangle (from lateral to medial) • Femoral nerve (and its branches) • Saphenous nerve (sensory branch of the femoral nerve) • Femoral artery (and its several branches) • Deep femoral artery (deep artery of the thigh) and its branches in this region; medial and lateral circumflex femoral arteries and perforating branches • Femoral vein (and veins draining to its proximal part such as the great saphenous vein and deep femoral vein) • Deep inguinal lymph nodes MUSCULAR AND VASCULAR COMPARTMENTS -

Leg and Foot
Dr. Sangeeta Kotrannavar Assistant Professor Dept. of Anatomy USM-KLE IMP, Belagavi Describe the bony landmarks of tibia and fibula Describe the osteology of tibia, fibula, tarsals, metatarsals and phalanges State the anterior, posterior and lateral compartments of the leg Describe the attachments, actions and innervations of the muscles in each compartment Describe the blood supply and nerve supply in each compartment Describe the tarsal tunnel and its contents State the four layers of muscles in the sole of the foot Describe the blood supply and innervation of the sole of the foot Explain the arches of the foot and its significant Describe the applied anatomy of the foot Leg is between the knee and ankle joint – bones tibia & fibula Foot is distal to the ankle joint Lat. Medial Tibia is large, weight-bearing shin bone Medially placed, Long bone Equivalent to radius Parts Upper end, Lower end, Shaft • Upper end - med. & Lat. Condyles, intercondylar area (non articular), tibial tuberosity • Condyles articulates with condyles of femur. • Intercondylar area—attachment fro before backwards: Ant. Horn of med. Miniscus, ant. Cruciate lig., ant. Horn of lat. Miniscus. post. Horn of lat. Miniscus, post. Horn of med. Miniscus, post. Cruciate lig. • Med. Condyle - post - semimembranosus. Ant. - sartorius, gracilus, semitendinosus. • Tibial tuberosity - ligamentum patellae. • Lower end - medial malleolus – tip - deltoid lig. • Shaft - triangular. Borders - ant., med., lat • Shaft - Surfaces - anteromedial (subcutaneous), anterolat. -

A Rare Case of Posterior Tibial Artery Hypoplasia And
Folia Medica 61(3): 467-71 DOI: 10.3897/folmed.61.e39414 Case Report A Rare Case of Posterior Tibial Artery Hypoplasia and Fibular Artery Enlargement and their Impact on the Arterial Supply of Posterior Crural Region Maria Piagkou1, Stylianos Kapetanakis2, George Tsakotos1, Alexandros Samolis1, Nikolaos Anastasopoulos3, Konstantinos Natsis3 1 Department of Anatomy and Surgical Anatomy, School of Medicine, National and Kapodistrian University of Athens, Greece 2 Spine Department and Deformities, Interbalkan European Medical Center, Thessaloniki, Greece 3 Department of Anatomy and Surgical Anatomy, School of Medicine, Faculty of Health Sciences, Aristotle University of Thessaloniki, Greece Corresponding author: Stylianos Kapetanakis, Spine Department and Deformities, Interbalkan European Medical Center, Thessaloniki, 55535, Greece; E-mail: [email protected]; Tel: 00306972707384 Received: 05 Feb 2019 ♦ Accepted: 28 Mar 2019 ♦ Published: 30 Sep 2019 Citation: Piagkou M, Kapetanakis S, Tsakotos G, Samolis A, Anastasopoulos N, Natsis K. A rare case of posterior tibial artery hypopla- sia and fibular artery enlargement and their impact on the arterial supply of posterior crural region. Folia Med (Plovdiv) 2019; 61(3): 467–71. doi: 10.3897/folmed.61.e39414 Abstract Background: Detailed knowledge of the popliteal artery division and possible anatomical variants is of paramount importance for vascular surgery. Aim: The aim of the current study was to highlight a rare unilateral case of posterior tibial artery hypoplasia. Materials and methods: A dissection was performed at the posterior surface of the tibia in a 78-year-old Caucasian male cadaver of Greek origin. Results: The findings were consistent with unilateral posterior tibial artery hypoplasia and fibular artery enlargement. -

Dorsalis Pedis Artery As a Continuation of Peroneal Artery—Clinical and Embryological Aspects Seema Sehmi
CTDT Seema Sehmi 10.5005/jp-journals-10055-0036 CASE REPORT Dorsalis Pedis Artery as a Continuation of Peroneal Artery—Clinical and Embryological Aspects Seema Sehmi ABSTRACT The knowledge of these arterial variations are important as damage to them can be limb threatening. The DPA also Aim: To report a rare case of continuation of the peroneal known as a dorsal artery of the foot is the continuation artery as dorsalis pedis artery (DPA) in the foot. of the ATA at the talocrural joint just distal to the inferior Background: Peripheral arterial system of the lower limb retinaculum. It runs towards the first intermetatarsal especially the DPA is commonly used to diagnose the peripheral arterial diseases. space and divides into the first dorsal metatarsal artery and deep plantar artery which form deep plantar arch.2 Case report: During the routine dissection of a formalized right lower limb of a 52-year-old male cadaver the arterial system of Normally, the PA is the continuation of the femoral artery. the lower limb was dissected and studied. The popliteal artery It traverses the popliteal fossa, and it descends obliquely (PA) divided into anterior and posterior tibial arteries (PTA) at to the distal border of the popliteal muscle. It then divides the lower border of the popliteus muscle. The peroneal artery, into anterior and PTA. The ATA runs to the anterior com- branch from the posterior tibial artery was found larger than partment of the leg through an aperture in the proximal usual. It ran downward laterally and after piercing the lower part of the interosseous membrane and continues as part of interosseous membrane continued as dorsalis pedis artery on the dorsum of the foot. -

An Anatomic Study of Vascularized Fibular Grafts
Chinese Journal of Traumatology 2008; 11(5):279-282 . 279 . An anatomic study of vascularized fibular grafts ZHU Yue-liang 朱跃良*, XU Yong-qing 徐永清, YANG Jun 杨军, Li Jun 李军 and LAN Xiu-fu 兰秀夫 Objective: To study the applied anatomy of the vascu- arcuate arteries were constantly located between the distal lar and muscular innervations related to vascularized fibular half of the 1/4 segment and 2/4 segment of the fibula. The grafts. muscular branch of the superficial peroneal nerve passed Methods: Thirty-four cadaveric lower extremities were through the surface of the periosteum in the 2/4 segment of dissected for this study. The observations included fibular the fibula. length, fibular nutrient artery, arcuate arteries, and innerva- Conclusions: The most proximal osteotomy point lo- tion of fibular muscles. The fibulas were averagely divided cates at the midpoint of the 1/4 segment by which it ensure into four segments and the locations of relevant vessels the maximal potential for preserving the nutrient vessels. and nerves were ascertained. The muscular branch of the superficial peroneal nerve is Results: All specimens had 1 fibular nutrient artery fragile to injury at the 2/4 segment of the fibula. and 4-9 arcuate arteries except 1 specimen which had only 1 Key words: Fibula; Grafts; Anatomy; Artery; Nerves arcuate artery. The fibular nutrient artery and the first three Chin J Traumatol 2008; 11(5):279-282 ince Taylor1 firstly reported the vascularized tomical knowledge will be greatly helpful for surgeons fibular grafts, this technique has been widely to perform vascularized fibular graft operations. -

THE ANATOMICAL STUDY of POPLITEAL ARTERY and ITS VARIA- TIONS Soumya Philippose 1, J
International Journal of Anatomy and Research, Int J Anat Res 2017, Vol 5(4.3):4679-85. ISSN 2321-4287 Original Research Article DOI: https://dx.doi.org/10.16965/ijar.2017.435 THE ANATOMICAL STUDY OF POPLITEAL ARTERY AND ITS VARIA- TIONS Soumya Philippose 1, J. Sujitha Jacinth *2, V. Muniappan 3. 1 Assistant professor, Department of Anatomy, Amala Institute of Medical Sciences, Trichur, India. *2 Assistant professor, Department of Anatomy, RMMCH, Annamalai University, Chidambaram, India. 2 Professor and Head, Department of Anatomy, RMMCH, Annamalai University, Chidambaram, India. ABSTRACT Introduction & aim: Anatomical variations in the arterial system are very common. In spite of advanced invasive techniques, knowledge of variations still remains limited. One such artery showing variations is the popliteal artery. Limb-threatening sequelae ensue from its damage. The aim of the study encompasses gaining knowledge on the anatomy of Popliteal artery with respect to its commencement, termination, branching pattern & its relation with surrounding structures mainly the muscles in the Popliteal fossa with a view of helping surgeons from various fields while performing surgery in this region. Comparison with results from previous studies on the popliteal artery was also planned. Materials and Methods: The study was carried out in 50 lower limbs of 25 well embalmed cadavers of South Indian origin irrespective of age and sex. None of the limbs showed any evidence of previous knee surgery. Results: Popliteal artery was the continuation of femoral artery. The level of termination in relation to the Popliteus muscle was high in one case and in the middle in another case. Popliteal artery terminated into anterior tibial and posterior tibial arteries.