Leg and Foot
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ideal Medial Malleolar Screw Length Based on the Tibial Epiphyseal Scar Location in Weight Bearing CT’S Collin G
Ideal Medial Malleolar Screw Length Based on the Tibial Epiphyseal Scar Location in Weight Bearing CT’s Collin G. Messerly DPM, Keegan A. Duelfer DPM, Troy J. Boffeli DPM, FACFAS, Tyler K. Sorensen, DPM Regions Hospital / HealthPartners Institute for Education and Research - Saint Paul, MN Figure 1. Zone of Dense Bone in Medial Malleolar ORIF Figure 4. Measuring Distal – Most 5% to Medial Malleolus Table 2. Distance Between Epiphyseal Scar & Distal – Most 5% of RESULTS STATEMENT OF PURPOSE The epiphyseal scar is located in the distal The medial malleolus to distal – most 5% mark Tibia 97 WB ankle CT scans evaluated in uninjured ankles Medial malleolar fractures are one of the most common fracture types metaphysis of the tibia, and can oftentimes be was measured on the coronal WB CT slice with Measurement of interest Male: Mean ± SD Female: Mean ± SD (mm) In males < 60 years old there was a 12.75 mm zone of increased bone the widest medial malleolus. Screw threads observed in the ankle joint and have been long fixated with two screws; easily visualized on X-ray and CT scan (red line). (mm) density, as compared to 13.66 mm in those ≥ 60 which was not statistically The distal – most 5% of the tibia (distal to the beyond this point will purchase less dense bone however, the bone density of the distal tibia has potential for poor screw significant. purchase due to compromised bone density. This is especially true in elderly black line) contains dense bone with marked in the medullary canal with potential to not have Epiphyseal Scar to Medial Malleolus 12.75 ± 2.91 9.39 ± 2.38 In females < 60 years old there was 9.39 mm zone of increased bone populations with osteoporotic bone. -

Assessment, Management and Decision Making in the Treatment Of
Pediatric Ankle Fractures Anthony I. Riccio, MD Texas Scottish Rite Hospital for Children Update 07/2016 Pediatric Ankle Fractures The Ankle is the 2nd most Common Site of Physeal Injury in Children 10-25% of all Physeal Injuries Occur About the Ankle Pediatric Ankle Fractures Primary Concerns Are: • Anatomic Restoration of Articular Surface • Restoration of Symmetric Ankle Mortise • Preservation of Physeal Growth • Minimize Iatrogenic Physeal Injury • Avoid Fixation Across Physis in Younger Children Salter Harris Classification Prognosis and Treatment of Pediatric Ankle Fractures is Often Dictated by the Salter Harris Classification of Physeal Fractures Type I and II Fractures: Often Amenable to Closed Tx / Lower Risk of Physeal Arrest Type III and IV: More Likely to Require Operative Tx / Higher Risk of Physeal Arrest Herring JA, ed. Tachdjian’s Pediatric Orthopaedics, 5th Ed. 2014. Elsevier. Philadelphia, PA. ISOLATED DISTAL FIBULA FRACTURES Distal Fibula Fractures • The Physis is Weaker than the Lateral Ankle Ligaments – Children Often Fracture the Distal Fibula but…. – …ligamentous Injuries are Not Uncommon • Mechanism of Injury = Inversion of a Supinated Foot • SH I and II Fractures are Most Common – SH I Fractures: Average Age = 10 Years – SH II Fractures: Average Age = 12 Years Distal Fibula Fractures Lateral Ankle Tenderness SH I Distal Fibula Fracture vs. Lateral Ligamentous Injury (Sprain) Distal Fibula Fractures • Sankar et al (JPO 2008) – 37 Children – All with Open Physes, Lateral Ankle Tenderness + Normal Films – 18%: Periosteal -

Classification System of the Tibiofibular Syndesmosis Blood Supply and Its
www.nature.com/scientificreports OPEN Classifcation system of the tibiofbular syndesmosis blood supply and its clinical relevance Received: 16 February 2018 Izabela Mróz1, Piotr J. Bachul1,2, Krzysztof A. Tomaszewski1, Tomasz Bereza1, Krzysztof Gil3, Accepted: 7 June 2018 Jerzy A. Walocha1 & Artur Pasternak 1 Published: xx xx xxxx Due to the lack of anatomical studies concerning complexity of the tibiofbular syndesmosis blood supply, density of blood vessels with further organization of syndesmotic vascular variations is presented in clinically relevant classifcation system. The material for the study was obtained from cadaveric dissections. We dissected 50 human ankles observing diferent types of arterial blood supply. Our classifcation system is based on the vascular variations of the anterior aspect of tibiofbular syndesmosis and corresponds with vascular density. According to our study the mean vascular density of tibiofbular syndesmosis is relatively low (4.4%) and depends on the type of blood supply. The highest density was observed among ankles with complete vasculature and the lowest when lateral anterior malleolar artery was absent (5.8% vs. 3.5%, respectively). Awareness of various types of tibiofbular syndesmosis arterial blood supply is essential for orthopedic surgeons who operate in the ankle region and radiologists for the anatomic evaluation of this area. Knowledge about possible variations along with relatively low density of vessels may contribute to modifcation of treatment approach by the increase of the recommended time of syndesmotic screw stabilization in order to prevent healing complications. Tibiofbular syndesmosis is a fbrous connection localized between the fbular notch of the tibia and medial surface of the lateral ankle. -

Vessels and Circulation
CARDIOVASCULAR SYSTEM OUTLINE 23.1 Anatomy of Blood Vessels 684 23.1a Blood Vessel Tunics 684 23.1b Arteries 685 23.1c Capillaries 688 23 23.1d Veins 689 23.2 Blood Pressure 691 23.3 Systemic Circulation 692 Vessels and 23.3a General Arterial Flow Out of the Heart 693 23.3b General Venous Return to the Heart 693 23.3c Blood Flow Through the Head and Neck 693 23.3d Blood Flow Through the Thoracic and Abdominal Walls 697 23.3e Blood Flow Through the Thoracic Organs 700 Circulation 23.3f Blood Flow Through the Gastrointestinal Tract 701 23.3g Blood Flow Through the Posterior Abdominal Organs, Pelvis, and Perineum 705 23.3h Blood Flow Through the Upper Limb 705 23.3i Blood Flow Through the Lower Limb 709 23.4 Pulmonary Circulation 712 23.5 Review of Heart, Systemic, and Pulmonary Circulation 714 23.6 Aging and the Cardiovascular System 715 23.7 Blood Vessel Development 716 23.7a Artery Development 716 23.7b Vein Development 717 23.7c Comparison of Fetal and Postnatal Circulation 718 MODULE 9: CARDIOVASCULAR SYSTEM mck78097_ch23_683-723.indd 683 2/14/11 4:31 PM 684 Chapter Twenty-Three Vessels and Circulation lood vessels are analogous to highways—they are an efficient larger as they merge and come closer to the heart. The site where B mode of transport for oxygen, carbon dioxide, nutrients, hor- two or more arteries (or two or more veins) converge to supply the mones, and waste products to and from body tissues. The heart is same body region is called an anastomosis (ă-nas ′tō -mō′ sis; pl., the mechanical pump that propels the blood through the vessels. -

Vascular Anatomy of the Free Fibula Flap Including the Lateral Head of the Soleus Muscle Applied to Maxillo-Mandibular Reconstruction
Surgical and Radiologic Anatomy (2019) 41:447–454 https://doi.org/10.1007/s00276-018-2166-2 ORIGINAL ARTICLE Vascular anatomy of the free fibula flap including the lateral head of the soleus muscle applied to maxillo-mandibular reconstruction Lara Nokovitch1,2 · Julien Davrou2 · François Bidault4 · Bernard Devauchelle2 · Stéphanie Dakpé2 · Christian Vacher3,5 Received: 1 May 2018 / Accepted: 8 December 2018 / Published online: 14 December 2018 © Springer-Verlag France SAS, part of Springer Nature 2018 Abstract Purpose Initially described by Baudet in 1982, the fibula flap including the lateral head of the soleus muscle allows a one- stage reconstruction for large maxillo-mandibular defects. The aim of this study was to evaluate the number of muscular branches destined to the soleus muscle and their distance from the origin of the fibular artery, to assess the vascular anatomy of the free fibula flap including the lateral head of the soleus muscle applied to maxillo-mandibular reconstruction. Methods We performed a cadaveric anatomic study on ten lower limbs, and a CT angiography anatomic study on 38 legs. The number of soleus branches originating from the fibular artery, and the distance between the origin of the fibular artery and each of the identified branches were measured. Results The number of soleus branches destined to the lateral head of the soleus muscle is variable, with in our study 1–3 branches found. Soleus branches destined to the lateral head of the soleus muscle emerged at a distance ranging between 0 and 2.9 cm (mean value = 1.82 cm) from the origin of the fibular artery in 40% of cases, between 3 and 5.9 cm (mean value = 4.27 cm) from the origin of the fibular artery in 37% of cases, and was at a distance of 6 cm or more (mean value = 6.93 cm) from the origin of the fibular artery in 20% of cases. -

Compiled for Lower Limb
Updated: December, 9th, 2020 MSI ANATOMY LAB: STRUCTURE LIST Lower Extremity Lower Extremity Osteology Hip bone Tibia • Greater sciatic notch • Medial condyle • Lesser sciatic notch • Lateral condyle • Obturator foramen • Tibial plateau • Acetabulum o Medial tibial plateau o Lunate surface o Lateral tibial plateau o Acetabular notch o Intercondylar eminence • Ischiopubic ramus o Anterior intercondylar area o Posterior intercondylar area Pubic bone (pubis) • Pectineal line • Tibial tuberosity • Pubic tubercle • Medial malleolus • Body • Superior pubic ramus Patella • Inferior pubic ramus Fibula Ischium • Head • Body • Neck • Ramus • Lateral malleolus • Ischial tuberosity • Ischial spine Foot • Calcaneus Ilium o Calcaneal tuberosity • Iliac fossa o Sustentaculum tali (talar shelf) • Anterior superior iliac spine • Anterior inferior iliac spine • Talus o Head • Posterior superior iliac spine o Neck • Posterior inferior iliac spine • Arcuate line • Navicular • Iliac crest • Cuboid • Body • Cuneiforms: medial, intermediate, and lateral Femur • Metatarsals 1-5 • Greater trochanter • Phalanges 1-5 • Lesser trochanter o Proximal • Head o Middle • Neck o Distal • Linea aspera • L • Lateral condyle • L • Intercondylar fossa (notch) • L • Medial condyle • L • Lateral epicondyle • L • Medial epicondyle • L • Adductor tubercle • L • L • L • L • 1 Updated: December, 9th, 2020 Lab 3: Anterior and Medial Thigh Anterior Thigh Medial thigh General Structures Muscles • Fascia lata • Adductor longus m. • Anterior compartment • Adductor brevis m. • Medial compartment • Adductor magnus m. • Great saphenous vein o Adductor hiatus • Femoral sheath o Compartments and contents • Pectineus m. o Femoral canal and ring • Gracilis m. Muscles & Associated Tendons Nerves • Tensor fasciae lata • Obturator nerve • Iliotibial tract (band) • Femoral triangle: Boundaries Vessels o Inguinal ligament • Obturator artery o Sartorius m. • Femoral artery o Adductor longus m. -

Injuries to the Lower Extremity II
Injury to lower extremity InjuriesInjuries toto thethe lowerlower extremityextremity IIII Aree Tanavalee MD Associate Professor Department of Orthopaedics Faculty of Medicine Chulalongkorn University Injury to lower extremity TopicsTopics • Fracture of the shaft of the femur • Fractures around the knee • Knee dislocation and fracture dislocation • Fractures of tibia and fibular • Fractures around the ankle • Fracture and fracture dislocation of the foot Injury to lower extremity CommonCommon symptomssymptoms andand signssigns ofof fracturesfractures – Pain – Deformity – Shortening – Swelling – Ecchymosed – Loss of function – Open injury • Gross finding of fractures Injury to lower extremity RadiographicRadiographic evaluationevaluation forfor fracturesfractures • At least, 2 different planes of Fx site – Includes joint above and below – Some types of Fx, special views – Sometimes, 2 different times – Sometimes, calls second opinion Injury to lower extremity ComplicationsComplications ofof fracturesfractures • General – Delayed union – Nonunion – Malunion – Shortening – Infection • Severe – Neurovascular injuries – Compartment syndrome – Fat embolism – Adult respiratory distress syndrome (ARDS) Injury to lower extremity FatFat embolismembolism • Common in Fx of long bone and pelvis • Multiple Fxs >> single Fx • Respiratory insufficiency • Usually manifests within 48 hr • Clinical – Fever – Tachepnea – Tachycardia – Alters consciousness • Treatment – Respiratory support – Early Fx stabilization Injury to lower extremity CompartmentCompartment -

Back of Leg I
Back of Leg I Dr. Garima Sehgal Associate Professor “Only those who risk going too far, can possibly find King George’s Medical University out how far one can go.” UP, Lucknow — T.S. Elliot DISCLAIMER Presentation has been made only for educational purpose Images and data used in the presentation have been taken from various textbooks and other online resources Author of the presentation claims no ownership for this material Learning Objectives By the end of this teaching session on Back of leg – I all the MBBS 1st year students must be able to: • Enumerate the contents of superficial fascia of back of leg • Write a short note on small saphenous vein • Describe cutaneous innervation in the back of leg • Write a short note on sural nerve • Enumerate the boundaries of posterior compartment of leg • Enumerate the fascial compartments in back of leg & their contents • Write a short note on flexor retinaculum of leg- its attachments & structures passing underneath • Describe the origin, insertion nerve supply and actions of superficial muscles of the posterior compartment of leg Introduction- Back of Leg / Calf • Powerful superficial antigravity muscles • (gastrocnemius, soleus) • Muscles are large in size • Inserted into the heel • Raise the heel during walking Superficial fascia of Back of leg • Contains superficial veins- • small saphenous vein with its tributaries • part of course of great saphenous vein • Cutaneous nerves in the back of leg- 1. Saphenous nerve 2. Posterior division of medial cutaneous nerve of thigh 3. Posterior cutaneous -

Morphometric Study of Tibial Condylar Area in the North Indian Population. Ankit Srivastava1, Dr
JMSCR Volume||2||Issue||3||Page515-519||March 2014 2014 www.jmscr.igmpublication.org Impact Factcor-1.1147 ISSN (e)-2347-176x Morphometric Study of Tibial Condylar area in the North Indian Population. Ankit Srivastava1, Dr. Anjoo Yadav2, Prof. R.J. Thomas3, Ms. Neha Gupta4 1Tutor in AIIMS Bhopal. 2Lecturer in Govt. medical college, Kannauj. 3Professor in Govt. medical college, Kannauj. 4Tutor in Govt. medical college, Kannauj. Email: [email protected] Abstract: The upper end of tibia is expanded to form a mass that consists of two parts: lateral and medial condyles which articulate with the corresponding condylar surfaces of the femur. Separating these two condyles is the intercondylar area whose central part is raised to form the intercondylar eminence. The present study will give information of the exact dimensions and percentage covered by medial and lateral condyles out of total condylar area. This study was undertaken to collect metrical data about the medial and lateral condyles of tibia. The present study was performed on 150 dry tibia of north Indian subjects, Out of which 70 tibia belonged to right side and 80 were of left side. The age and sex of these bones were not known. The anteroposterior length of medial and lateral tibial condylar area was measured along with their transverse diameter. The data was statistically analyzed to hold comparisons between tibia of right and left side and also between medial and lateral tibial condyles of the same side. The area covered by MTC is 38.56% and by LTC is 35.97% out of total condylar area in right side. -
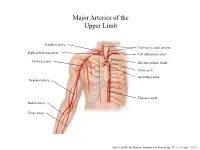
Major Arteries of the Upper Limb
Major Arteries of the Upper Limb Vertebral artery Common carotid arteries Right subclavian artery Left subclavian artery Axillary artery Brachiocephalic trunk Aortic arch Ascending aorta Brachial artery Thoracic aorta Radial artery Ulnar artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.23 Major Arteries of the Abdominal Region Renal artery Celiac trunk Abdominal aorta Superior mesenteric artery Gonadal artery Inferior mesenteric artery Common iliac artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.24 Common iliac artery Internal iliac artery Major Arteries of the External iliac artery Lower Limb Femoral artery Popliteal artery Anterior tibial artery Fibular artery Posterior tibial artery Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.25 Major Veins of the Upper Limb Internal jugular vein (left) Subclavian vein (right) External jugular vein (left) Axillary vein Brachiocephalic veins Cephalic vein Superior vena cava Brachial vein Basilic vein Median cubital vein Inferior vena cava Radial vein Ulnar vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.28 Major Veins of the Abdominal Cavity – Part 1 Hepatic veins Inferior vena cava Renal vein (left) Gonadal vein (left) Gonadal vein (right) Common iliac vein (left) Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Major Veins of the Abdominal Cavity – Part 2 (Hepatic portal circulation) Hepatic portal vein Splenic vein Inferior mesenteric vein Superior mesenteric vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.29 Common iliac vein (left) Internal iliac vein Major Veins of the External iliac vein Lower Limb Great saphenous vein Femoral vein Popliteal vein Fibular vein Small saphenous vein Anterior tibial Posterior tibial vein vein Marieb & Hoehn (Human Anatomy and Physiology, 9th ed.) – Figure 19.30 . -

Anatomy of the Foot and Ankle
Anatomy Of The Foot And Ankle Multimedia Health Education Disclaimer This movie is an educational resource only and should not be used to manage Orthopaedic Health. All decisions about management of the Foot and Ankle must be made in conjunction with your Physician or a licensed healthcare provider. Anatomy Of The Foot And Ankle Multimedia Health Education MULTIMEDIA HEALTH EDUCATION MANUAL TABLE OF CONTENTS SECTION CONTENT 1 . ANATOMY a. Ankle & Foot Anatomy b. Soft Tissue Anatomy 2 . BIOMECHANICS Anatomy Of The Foot And Ankle Multimedia Health Education Unit 1: Anatomy Introduction The foot and ankle in the human body work together to provide balance, stability, movement, and Propulsion. This complex anatomy consists of: 26 bones 33 joints Muscles Tendons Ligaments Blood vessels, nerves, and soft tissue In order to understand conditions that affect the foot and ankle, it is important to understand the normal anatomy of the foot and ankle. Ankle The ankle consists of three bones attached by muscles, tendons, and ligaments that connect the foot to the leg. In the lower leg are two bones called the tibia (shin bone) and the fibula. These bones articulate (connect) to the Talus or ankle bone at the tibiotalar joint (ankle joint) allowing the foot to move up and down. The bony protrusions that we can see and feel on the ankle are: Lateral Malleolus: this is the outer ankle bone formed by the distal end of the fibula. Medial Malleolus: this is the inner ankle bone formed by the distal end of the tibia. Tibia (shin bone) (Refer fig.1) Tibia -

Clinical Anatomy of the Lower Extremity
Государственное бюджетное образовательное учреждение высшего профессионального образования «Иркутский государственный медицинский университет» Министерства здравоохранения Российской Федерации Department of Operative Surgery and Topographic Anatomy Clinical anatomy of the lower extremity Teaching aid Иркутск ИГМУ 2016 УДК [617.58 + 611.728](075.8) ББК 54.578.4я73. К 49 Recommended by faculty methodological council of medical department of SBEI HE ISMU The Ministry of Health of The Russian Federation as a training manual for independent work of foreign students from medical faculty, faculty of pediatrics, faculty of dentistry, protocol № 01.02.2016. Authors: G.I. Songolov - associate professor, Head of Department of Operative Surgery and Topographic Anatomy, PhD, MD SBEI HE ISMU The Ministry of Health of The Russian Federation. O. P.Galeeva - associate professor of Department of Operative Surgery and Topographic Anatomy, MD, PhD SBEI HE ISMU The Ministry of Health of The Russian Federation. A.A. Yudin - assistant of department of Operative Surgery and Topographic Anatomy SBEI HE ISMU The Ministry of Health of The Russian Federation. S. N. Redkov – assistant of department of Operative Surgery and Topographic Anatomy SBEI HE ISMU THE Ministry of Health of The Russian Federation. Reviewers: E.V. Gvildis - head of department of foreign languages with the course of the Latin and Russian as foreign languages of SBEI HE ISMU The Ministry of Health of The Russian Federation, PhD, L.V. Sorokina - associate Professor of Department of Anesthesiology and Reanimation at ISMU, PhD, MD Songolov G.I K49 Clinical anatomy of lower extremity: teaching aid / Songolov G.I, Galeeva O.P, Redkov S.N, Yudin, A.A.; State budget educational institution of higher education of the Ministry of Health and Social Development of the Russian Federation; "Irkutsk State Medical University" of the Ministry of Health and Social Development of the Russian Federation Irkutsk ISMU, 2016, 45 p.