Coding for Respiratory Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Management of Empysema
Surgical Management of Empysema John A Odell MB ChB, FRCS(Ed), FACS Emeritus Professor of Surgery Mayo Clinic College of Medicine Previously Surgical Director Lung Transplantation ©2013 MFMER | slide-1 Problem case. How would you manage? • 64yr male • Previous RLL bullectomy. • Recent left pneumothorax managed elsewhere with chest tube placement. • Because of continued air-leak talc pleurodesis. • Air-leak continues. ©2013 MFMER | slide-2 • On nasal oxygen. Dyspneic on walking • Significant air-leak. More dyspneic when suction applied to chest drain. • FEV1 40% predicted. DLCO 12% predicted. Options? • Thoracotomy and close air leak surgically • Videothoracoscopy and closure of air-leak • Thoracotomy and decortication • Remove chest drain • List for transplantation Historical Treatment of Emphysema • Abdominal compression belts. The stimulus was the observation that emphysematous patients lean forward when breathing. • Pneumoperitoneum. In an attempt to restore diaphragmatic curvature. • Lungs too large for the chest – costochondrectomy or transverse sternotomy to provide more room. Multiple wedge excisions. • Chest grown too large – thoracoplasty • Pleurodesis. Emphysema results from alveolar wall ischemia. • Phrenectomy. Overvigerous inspiration was ripping alveolar walls. • Hilar denervation. To decrease bronchoconstriction and mucous production mediated by the parasympathetic nervous system. • Whole lung irradiation. To increase elastic recoil by inducing fibrosis. ©2013 MFMER | slide-7 Variants of Emphysema that may be Surgically -

Effect of an Indwelling Pleural Catheter Vs Talc Pleurodesis On
This supplement contains the following items: 1. Original protocol, final protocol, summary of changes. 2. Original statistical analysis plan. There were no further changes to the original statistical analysis plan. Downloaded From: https://jamanetwork.com/ on 10/02/2021 The Australasian Malignant Pleural Effusion Trial (AMPLE) A Multicentre Randomized Study Comparing Indwelling Pleural Catheter vs Talc Pleurodesis in Patients with Malignant Pleural Effusions Ethics Registration number 2012-005 Protocol version number 1.0 Protocol date 10/01/2012 Authorised by: Name: Prof YC Gary Lee Role: Chief Investigator Signature: Date: 10/01/2012 Downloaded From: https://jamanetwork.com/ on 10/02/2021 General Information This document describes the Western Australian Randomised Malignant Effusion trial for the purpose of submission for review by the relevant human research and ethics committees. It provides information about procedures for entering patients into the trial and this protocol should not be used as a guide for the treatment of other patients; every care was taken in its drafting, but corrections or amendments may be necessary. Questions or problems relating to this study should be referred to the Chief Investigator or Trial Coordinator. Compliance The trial will be conducted in compliance with this protocol, the National Statement on Ethical Conduct in Human Research, data protection laws and other guidelines as appropriate. It will be registered with the Australia and New Zealand Clinical Trials Registry, once ethical approval is secured. -

Management of Parapneumonic Effusion and Empyema Sarvinder Singh, Santosh Kumar Singh, Ajai Kumar Tentu
[Downloaded free from http://www.jacpjournal.org on Friday, November 29, 2019, IP: 176.240.166.40] Review Article Management of parapneumonic effusion and empyema Sarvinder Singh, Santosh Kumar Singh, Ajai Kumar Tentu Military Hospital, Namkum, Parapneumonic effusions are pleural effusions that occur in the pleural space adjacent Ranchi, Jharkhand, India to a bacterial pneumonia. When bacteria invade the pleural space, a complicated parapneumonic effusion or empyema may result. Empyema is collection of pus in BSTRACT pleural cavity. If left untreated, complicated parapneumonic effusion/empyema leads A to chronic encasement and pleural thickening. Simple parapneumonic effusions can be managed conservatively with appropriate antibiotics, but complicated parapneumonic effusions often require some kind of drainage along with antibiotics. Delay in treatment is associated with high morbidity and mortality. Clinically it is diagnosed with persistent fever, stony dull tender percussion, and absent breath sounds. Majority of cases are due to anaerobic infection. Gram-positive as well as Gram-negative organisms are also implicated. Many cases may have mixed organisms. Tuberculosis should be suspected if no organism is grown in empyema. Chest skiagram, thoracic ultrasound, and CT scan help in localization of effusion and detection of loculations. Confirmation is done by thoracocentesis and pleural fluid analysis, which shows exudate with polymorphonuclear leukocytosis. Management includes well-selected antibiotics and drainage by tube thoracostomy. Intrapleural fibrinolytics have been used in multiloculated complicated parapneumonic effusions with success. Advent of thoracoscopy and VATS has left very few cases requiring surgical decortication. Properly treated parapneumonic effusions have good prognosis. KEYWORDS: Pleural effusion, empyema, chest tube thoracostomy, intrapleural Received: 1 December 2018 Accepted: 27 March 2019 fibrinolysis, VATS INTRODUCTION intrapleural debridement in parapneumonic empyema in [4] arapneumonic effusions are pleural effusions that 1950. -

Tracheal Intubation Following Traumatic Injury)
CLINICAL MANAGEMENT UPDATE The Journal of TRAUMA Injury, Infection, and Critical Care Guidelines for Emergency Tracheal Intubation Immediately after Traumatic Injury C. Michael Dunham, MD, Robert D. Barraco, MD, David E. Clark, MD, Brian J. Daley, MD, Frank E. Davis III, MD, Michael A. Gibbs, MD, Thomas Knuth, MD, Peter B. Letarte, MD, Fred A. Luchette, MD, Laurel Omert, MD, Leonard J. Weireter, MD, and Charles E. Wiles III, MD for the EAST Practice Management Guidelines Work Group J Trauma. 2003;55:162–179. REFERRALS TO THE EAST WEB SITE and impaired laryngeal reflexes are nonhypercarbic hypox- Because of the large size of the guidelines, specific emia and aspiration, respectively. Airway obstruction can sections have been deleted from this article, but are available occur with cervical spine injury, severe cognitive impairment on the Eastern Association for the Surgery of Trauma (EAST) (Glasgow Coma Scale [GCS] score Յ 8), severe neck injury, Web site (www.east.org/trauma practice guidelines/Emergency severe maxillofacial injury, or smoke inhalation. Hypoventi- Tracheal Intubation Following Traumatic Injury). lation can be found with airway obstruction, cardiac arrest, severe cognitive impairment, or cervical spinal cord injury. I. STATEMENT OF THE PROBLEM Aspiration is likely to occur with cardiac arrest, severe cog- ypoxia and obstruction of the airway are linked to nitive impairment, or severe maxillofacial injury. A major preventable and potentially preventable acute trauma clinical concern with thoracic injury is the development of Hdeaths.1–4 There is substantial documentation that hyp- nonhypercarbic hypoxemia. Lung injury and nonhypercarbic oxia is common in severe brain injury and worsens neuro- hypoxemia are also potential sequelae of aspiration. -

2019 Coding and Payment Information Pleural Effusions and Ascites Management
2019 coding and payment information Pleural effusions and ascites management The information contained in this document, including Reimbursement rates shown are Medicare national the codes supplied, is provided for informational payments for 2019 and do not reflect actual payments purposes only. BD makes no statement, promise or made to individual providers, as payments are adjusted guarantee concerning the appropriateness of any codes specific to particular geographic regions. for a particular procedure, actual levels of All information is subject to change without notice. In reimbursement, payment or charge or that addition, payers or local carriers may have their own reimbursement will be made. coding and billing requirements. Consult your payer This is not intended to be a comprehensive guide to all organization with regard to local reimbursement policies. coding and payment information. 2019 Medicare outpatient facility rates CPT® 2019 APC OPPS 2019 ASC Description APC Status code base rate* base rate Pleural catheter procedures 32550 Insertion of indwelling tunneled pleural catheter 5341 J1 $2,947 $1,790 32552 Removal of indwelling tunneled pleural catheter with cuff 5181 Q2 $620 $319 32560 Instillation via chest tube/catheter, agent for pleurodesis 5181 T $620 N/A 32650 Thoracoscopy, surgical, with pleurodesis (e.g., mechanical or chemical) N/A; inpatient procedure Peritoneal catheter procedures Insertion of tunneled intraperitoneal catheter (e.g., dialysis, intraperitoneal chemotherapy instillation, management of ascites), 49418 -

Unusual Case of Non-Resolving Necrotizing Pneumonia: a Last Resort Measure for Cure
eCommons@AKU Department of Surgery Department of Surgery June 2016 Unusual case of non-resolving necrotizing pneumonia: a last resort measure for cure. Naseem Salahuddin Aga Khan University, [email protected] Naila Baig Ansari Aga Khan University Saulat H. Fatimi Aga Khan University, [email protected] Follow this and additional works at: http://ecommons.aku.edu/pakistan_fhs_mc_surg_surg Part of the Surgery Commons Recommended Citation Salahuddin, N., Ansari, N., Fatimi, S. (2016). Unusual case of non-resolving necrotizing pneumonia: a last resort measure for cure.. JPMA: Journal of the Pakistan Medical Association, 66(6), 754-756. Available at: http://ecommons.aku.edu/pakistan_fhs_mc_surg_surg/566 754 CASE REPORT Unusual case of non-resolving necrotizing pneumonia: A last resort measure for cure Naseem Salahuddin, 1 Naila Baig-Ansari, 2 Saulat Hasnain Fatimi 3 Abstract pathogen of acute CAP, 2,3 and accounts for most cases of To our knowledge, this is an unusual case of a community- slowly resolving pneumonia.The majority of previously acquired pneumonia (CAP) with sepsis secondary to healthy hospitalized patients with severe CAP responded Streptococcus pneumoniae that required lung resection satisfactorily to prompt initiation of appropriate antibiotic for a non-resolving consolidation. A 74 year old previously therapy; however, it is estimated that 10% of hospitalized healthy woman, presented with acute fever, chills and CAP patients have slowly resolving or nonresolving pleuritic chest pain in Emergency Department (ED). A disease. 4 diagnosis of CAP was established with a Pneumonia Severity Index CURB-65 score of 5/5. In the ER, she was Case Report promptly and appropriately managed with antibiotics History: A 74 year old woman who was previously and aggressive supportive therapy. -
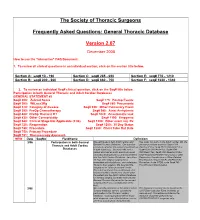
FAQ Document
The Society of Thoracic Surgeons Frequently Asked Questions: General Thoracic Database Version 2.07 December 2008 How to use the “interactive” FAQ Document: 1. To review all clinical questions in an individual section, click on the section title below. Section A: seq# 10 - 190 Section C: seq# 285 - 650 Section E: seq# 770 - 1210 Section B: seq# 200 - 260 Section D: seq# 660 - 750 Section F: seq# 1220 - 1340 2. To review an individual Seq# clinical question, click on the Seq# title below. Participation in both General Thoracic and Adult Cardiac Databases GENERAL STATEMENT #2 Seq# 200: Zubrod Score Seq# 775: Postop Events Seq# 300: WtLoss3Kg Seq# 860: Pneumonia Seq# 310: Category of disease Seq# 930: Other Pulmonary Event Seq# 390: PreOp Chemotherapy Seq# 940: Atrial Arrhythmia Seq# 400: PreOp Thoracic RT Seq# 1020: Anastomotic leak Seq# 430: Other Cormorbidity Seq# 1190: Empyema Seq# 540: Clinical Stage Not Applicable (2.06) Seq# 1200: Other event req. Rx Seq# 725: Reoperation Seq# 1250: 30 Day Status Seq# 740: Procedure Seq# 1280: Chest Tube Out Date Seq# 750: Primary Procedure Seq# 751: Thoracoscopy Approach NEW Date SeqNo FieldName Definition 3/06 Participation in both General We participate in both Adult Cardiac and Yes, enter into both. In the Adult Cardiac DB, the Thoracic and Adult Cardiac General Thoracic Database. Our question primary procedure would be Seq# 1310 pertains to whether the patient should end up OpOCard=Yes; Seq# 2510 ONCAoAn=Yes; Databases in both databases. Scenario--We had a Seq# 2530 ONCArch=Yes; Seq# 2540 patient who had an aortic aneurysm repair ONCDesc=Yes; Seq# 3220 Readm30=Yes; (arch/descending thoracic) and was entered Seq# ReadmRsn=either Pneumonia or other into the Adult Cardiac Database. -
Toman's Tuberculosis Case Detection, Treatment, and Monitoring
TOMAN’S TUBERCULOSIS TOMAN’S TUBERCULOSIS CASE DETECTION, TREATMENT, AND MONITORING The second edition of this practical, authoritative reference book provides a rational basis for the diagnosis and management of tuberculosis. Written by a number of experts in the field, it remains faithful to Kurt Toman’s original question-and-answer format, with subject matter grouped under the three headings Case detection, Treatment, and Monitoring. It is a testament to the enduring nature of the first edition that so much CASE DETECTION, TREA material has been retained unchanged. At the same time, the new edition has had not only to address the huge resurgence of tuber- culosis, the emergence of multidrug-resistant bacilli, and the special needs of HIV-infected individuals with tuberculosis, but also to encompass significant scientific advances. These changes in the profile of the disease and in approaches to management have inevitably prompted many new questions and answers and given a different complexion to others. Toman’s Tuberculosis remains essential reading for all who need to AND MONITORING TMENT, QUESTIONS learn more about every aspect of tuberculosis – case-finding, manage- ment, and effective control strategies. It provides invaluable support AND to anyone in the front line of the battle against this disease, from ANSWERS programme managers to policy-makers and from medical personnel to volunteer health workers. SECOND EDITION ISBN 92 4 154603 4 WORLD HEALTH ORGANIZATION WHO GENEVA Toman’s Tuberculosis Case detection, treatment, and monitoring – questions and answers SECOND EDITION Edited by T. Frieden WORLD HEALTH ORGANIZATION GENEVA 2004 WHO Library Cataloguing-in-Publication Data Toman’s tuberculosis case detection, treatment, and monitoring : questions and answers / edited by T. -

Agenda Item 5
List A (O) Respiratory system treatments and procedures. (1) Biopsy and/or excision (removal) of lesion of larynx, vocal cords, trachea (A) Loss or change of voice. (B) Swallowing or breathing difficulties. (C) Perforation (hole) or fistula (connection) in esophagus (tube from throat to stomach). (2) Rhinoplasty (surgery to change the shape of the nose) or nasal reconstruction with or without septoplasty A) Deformity of skin, bone or cartilage. (B) Creation of new problems, such as perforation of the nasal septum (hole in wall between the right and left halves of the nose) or breathing difficulty. (3) Submucous resection of nasal septum or nasal septoplasty (surgery to remove blockage in or straighten the nose) (A) Persistence, recurrence or worsening of the obstruction. (B) Perforation of nasal septum (hole in wall between the right and left halves of the nose) with dryness and crusting. (C) External deformity of the nose. (4) Sinus surgery/endoscopic sinus surgery (A) Spinal fluid leak (B) Visual loss or other eye injury (C) Numbness in front teeth and palate (D) Loss or reduction in sense of taste or smell (E) Recurrence of disease (F) Empty Nose Syndrome (sensation of nasal congestion, sensation of not being able to take in adequate air through nose) (G) Injury to tear duct causing drainage of tears down the cheek (H) Brain injury and/or infection (I) Injury to nasal septum (J) Nasal obstruction (5) Lung biopsy (A) Air leak with pneumothorax (leak of air from lung to inside of chest causing the lung to collapse) with need for insertion of chest drainage tube into space between lung and chest wall or repeat surgery. -

Translational Deep Phenotyping of Deaths Related to the COVID-19 Pandemic: Protocol for a Prospective Observational Autopsy Study
Open access Protocol BMJ Open: first published as 10.1136/bmjopen-2021-049083 on 27 August 2021. Downloaded from Translational deep phenotyping of deaths related to the COVID-19 pandemic: protocol for a prospective observational autopsy study Mikkel Jon Henningsen ,1 Apameh Khatam- Lashgari,1 Kristine Boisen Olsen,1 Christina Jacobsen,1 Christian Beltoft Brøchner ,2 Jytte Banner1 To cite: Henningsen MJ, ABSTRACT Strengths and limitations of this study Khatam- Lashgari A, Olsen KB, Introduction The COVID-19 pandemic is an international et al. Translational deep emergency with an extreme socioeconomic impact and a ► A standardised, prospective autopsy study on COVID- phenotyping of deaths high mortality and disease burden. The COVID-19 outbreak related to the COVID-19 19- related deaths with systematic data collection. is neither fully understood nor fully pictured. Autopsy studies pandemic: protocol for a ► A multidisciplinary, translational approach elucidat- can help understand the pathogenesis of COVID-19 and has prospective observational ing changes from protein level to whole human. already resulted in better treatment of patients. Structured autopsy study. BMJ Open ► A comprehensive biobank and extensive registry and systematic autopsy of COVID-19- related deaths will 2021;11:e049083. doi:10.1136/ data as an umbrella for planned and future research. bmjopen-2021-049083 enhance the mapping of pathophysiological pathways, not ► The internal control group partly compensates for possible in the living. Furthermore, it provides an opportunity Prepublication history and the observational design. ► to envision factors translationally for the purpose of disease additional supplemental material ► Limited by a selected sample of COVID-19 diseased prevention in this and future pandemics. -

Treatment and Outcomes of Community-Acquired Pneumonia at Canadian Hospitals Research Brian G
Treatment and outcomes of community-acquired pneumonia at Canadian hospitals Research Brian G. Feagan,* Thomas J. Marrie,† Catherine Y. Lau,‡ Recherche Susan L. Wheeler,‡ Cindy J. Wong,* Margaret K. Vandervoort* From *the London Clinical Abstract Trials Research Group, London, Ont.; †the Background: Community-acquired pneumonia is a common disease with a large Department of Medicine, economic burden. We assessed clinical practices and outcomes among patients University of Alberta, with community-acquired pneumonia admitted to Canadian hospitals. Edmonton, Alta.; Methods: A total of 20 hospitals (11 teaching and 9 community) participated. Data and ‡Janssen–Ortho from the charts of adults admitted during November 1996, January 1997 and Incorporated, Toronto, Ont. March 1997 were reviewed to determine length of stay (LOS), admission to an intensive care unit and 30-day in-hospital mortality. Multivariate analyses exam- This article has been peer reviewed. ined sources of variability in LOS. The type and duration of antibiotic therapy and the proportion of patients who were treated according to clinical practice CMAJ 2000;162(10):1415-20 guidelines were determined. Results: A total of 858 eligible patients were identified; their mean age was 69.4 (standard deviation 17.7) years. The overall median LOS was 7.0 days (in- terquartile range [IQR] 4.0–11.0 days); the median LOS ranged from 5.0 to 9.0 days across hospitals (IQR 6.0–7.8 days). Only 22% of the variability in LOS could be explained by known factors (disease severity 12%; presence of chronic obstructive lung disease or bacterial cause for the pneumonia 2%; hospital site 7%). -

Upper Vs. Lower in ICD-10
Acute Respiratory Tract Infection Acute respiratory infection [ARI] โรคิดเ้อเียบพันของระบบหายใจ้งแ่่องจูกึงุงลมในปอด ีอาการไ่เิน 4 ัปดา์ Upper respiratory infection [URI] โรคิดเ้อเียบพันของระบบหายใจ่วน้น เ่ม้งแ่่องจูกึงก่องเียง Chapter X Lower respiratory infection [LRI] J00-J99 Respiratory System โรคิดเ้อเียบพันของระบบหายใจ่วน่าง . พญ ้งใจ เจิญิล์ เ่ม้งแ่่วนบนของหลอดลมไปจนึงุงลมในปอด ก่มงานโสต ศอ นาิก รพ.สวรร์ประชาัก์ นครสวรร์ 1 2 Respiratory Tract Acute Respiratory Tract Infection Upper! vs. Lower Upper Respiratory Infection Lower Respiratory Infection ! Acute nasopharyngitis [Common cold] Acute bronchitis ! in ICD-10 Acute pharyngitis Acute bronchiolitis Acute tonsillitis Pneumonia ! Acute sinusitis Upper respiratory tract Acute laryngotracheitis Acute otitis media เ่ม้งแ่่องจูกึงหลอดลมให่ (trachea) Acute epiglottitis Lower respiratory tract Acute tracheitis Acute laryngotracheobronchitis เ่ม้งแ่หลอดลมของปอด (bronchus) ไปจนึงุงลมในปอด 3 4 Respiratory Tract Infection Upper Respiratory Tract Infection Summary Diagnosis ICD-10 Summary Diagnosis ICD-10 Acute nasopharyngitis J00 Tonsillitis J03.- Common cold J00 Acute laryngitis J04.0 Acute pharyngitis J02.9 Acute obstructive laryngitis J05.0 Acute suppurative pharyngitis J20.9 Acute laryngopharyngitis J06.0 Streptococcal pharyngitis J02.0 Acute epiglottitis J05.1 Specific organism pharyngitis J02.8 Acute tracheitis J04.1 Pharyngitis J02.9 Acute laryngotracheitis J04.2 Upper respiratory infection [URI] J06.9 Acute upper respiratory tract infection of multiple sites J06.8 Lower respiratory