Effect of an Indwelling Pleural Catheter Vs Talc Pleurodesis On
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Management of Empysema
Surgical Management of Empysema John A Odell MB ChB, FRCS(Ed), FACS Emeritus Professor of Surgery Mayo Clinic College of Medicine Previously Surgical Director Lung Transplantation ©2013 MFMER | slide-1 Problem case. How would you manage? • 64yr male • Previous RLL bullectomy. • Recent left pneumothorax managed elsewhere with chest tube placement. • Because of continued air-leak talc pleurodesis. • Air-leak continues. ©2013 MFMER | slide-2 • On nasal oxygen. Dyspneic on walking • Significant air-leak. More dyspneic when suction applied to chest drain. • FEV1 40% predicted. DLCO 12% predicted. Options? • Thoracotomy and close air leak surgically • Videothoracoscopy and closure of air-leak • Thoracotomy and decortication • Remove chest drain • List for transplantation Historical Treatment of Emphysema • Abdominal compression belts. The stimulus was the observation that emphysematous patients lean forward when breathing. • Pneumoperitoneum. In an attempt to restore diaphragmatic curvature. • Lungs too large for the chest – costochondrectomy or transverse sternotomy to provide more room. Multiple wedge excisions. • Chest grown too large – thoracoplasty • Pleurodesis. Emphysema results from alveolar wall ischemia. • Phrenectomy. Overvigerous inspiration was ripping alveolar walls. • Hilar denervation. To decrease bronchoconstriction and mucous production mediated by the parasympathetic nervous system. • Whole lung irradiation. To increase elastic recoil by inducing fibrosis. ©2013 MFMER | slide-7 Variants of Emphysema that may be Surgically -

2019 Coding and Payment Information Pleural Effusions and Ascites Management
2019 coding and payment information Pleural effusions and ascites management The information contained in this document, including Reimbursement rates shown are Medicare national the codes supplied, is provided for informational payments for 2019 and do not reflect actual payments purposes only. BD makes no statement, promise or made to individual providers, as payments are adjusted guarantee concerning the appropriateness of any codes specific to particular geographic regions. for a particular procedure, actual levels of All information is subject to change without notice. In reimbursement, payment or charge or that addition, payers or local carriers may have their own reimbursement will be made. coding and billing requirements. Consult your payer This is not intended to be a comprehensive guide to all organization with regard to local reimbursement policies. coding and payment information. 2019 Medicare outpatient facility rates CPT® 2019 APC OPPS 2019 ASC Description APC Status code base rate* base rate Pleural catheter procedures 32550 Insertion of indwelling tunneled pleural catheter 5341 J1 $2,947 $1,790 32552 Removal of indwelling tunneled pleural catheter with cuff 5181 Q2 $620 $319 32560 Instillation via chest tube/catheter, agent for pleurodesis 5181 T $620 N/A 32650 Thoracoscopy, surgical, with pleurodesis (e.g., mechanical or chemical) N/A; inpatient procedure Peritoneal catheter procedures Insertion of tunneled intraperitoneal catheter (e.g., dialysis, intraperitoneal chemotherapy instillation, management of ascites), 49418 -

Effect of Heliox Breathing on Flow Limitation in Chronic Heart Failure Patients
Eur Respir J 2009; 33: 1367–1373 DOI: 10.1183/09031936.00117508 CopyrightßERS Journals Ltd 2009 Effect of heliox breathing on flow limitation in chronic heart failure patients M. Pecchiari*, T. Anagnostakos#, E. D’Angelo*, C. Roussos#, S. Nanas# and A. Koutsoukou# ABSTRACT: Patients with chronic heart failure (CHF) exhibit orthopnoea and tidal expiratory flow AFFILIATIONS limitation in the supine position. It is not known whether the flow-limiting segment occurs in the *Istituto di Fisiologia Umana I, Universita` degli Studi di Milano, peripheral or central part of the tracheobronchial tree. The location of the flow-limiting segment Milan, Italy, and can be inferred from the effects of heliox (80% helium/20% oxygen) administration. If maximal #Dept of Critical Care and Pulmonary expiratory flow increases with this low-density mixture, the choke point should be located in the Services, Evangelismos General central airways, where the wave-speed mechanism dominates. If the choke point were located in Hospital, Medical School, University of Athens, Athens, Greece. the peripheral airways, where maximal flow is limited by a viscous mechanism, heliox should have no effect on flow limitation and dynamic hyperinflation. CORRESPONDENCE Tidal expiratory flow limitation, dynamic hyperinflation and breathing pattern were assessed in M. Pecchiari 14 stable CHF patients during air and heliox breathing at rest in the sitting and supine position. Istituto di Fisiologia Umana I via L. Mangiagalli 32 No patient was flow-limited in the sitting position. In the supine posture, eight patients exhibited 20133 Milan tidal expiratory flow limitation on air. Heliox had no effect on flow limitation and dynamic Italy hyperinflation and only minor effects on the breathing pattern. -
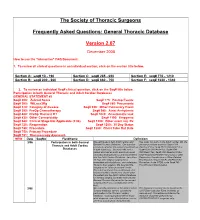
FAQ Document
The Society of Thoracic Surgeons Frequently Asked Questions: General Thoracic Database Version 2.07 December 2008 How to use the “interactive” FAQ Document: 1. To review all clinical questions in an individual section, click on the section title below. Section A: seq# 10 - 190 Section C: seq# 285 - 650 Section E: seq# 770 - 1210 Section B: seq# 200 - 260 Section D: seq# 660 - 750 Section F: seq# 1220 - 1340 2. To review an individual Seq# clinical question, click on the Seq# title below. Participation in both General Thoracic and Adult Cardiac Databases GENERAL STATEMENT #2 Seq# 200: Zubrod Score Seq# 775: Postop Events Seq# 300: WtLoss3Kg Seq# 860: Pneumonia Seq# 310: Category of disease Seq# 930: Other Pulmonary Event Seq# 390: PreOp Chemotherapy Seq# 940: Atrial Arrhythmia Seq# 400: PreOp Thoracic RT Seq# 1020: Anastomotic leak Seq# 430: Other Cormorbidity Seq# 1190: Empyema Seq# 540: Clinical Stage Not Applicable (2.06) Seq# 1200: Other event req. Rx Seq# 725: Reoperation Seq# 1250: 30 Day Status Seq# 740: Procedure Seq# 1280: Chest Tube Out Date Seq# 750: Primary Procedure Seq# 751: Thoracoscopy Approach NEW Date SeqNo FieldName Definition 3/06 Participation in both General We participate in both Adult Cardiac and Yes, enter into both. In the Adult Cardiac DB, the Thoracic and Adult Cardiac General Thoracic Database. Our question primary procedure would be Seq# 1310 pertains to whether the patient should end up OpOCard=Yes; Seq# 2510 ONCAoAn=Yes; Databases in both databases. Scenario--We had a Seq# 2530 ONCArch=Yes; Seq# 2540 patient who had an aortic aneurysm repair ONCDesc=Yes; Seq# 3220 Readm30=Yes; (arch/descending thoracic) and was entered Seq# ReadmRsn=either Pneumonia or other into the Adult Cardiac Database. -

Agenda Item 5
List A (O) Respiratory system treatments and procedures. (1) Biopsy and/or excision (removal) of lesion of larynx, vocal cords, trachea (A) Loss or change of voice. (B) Swallowing or breathing difficulties. (C) Perforation (hole) or fistula (connection) in esophagus (tube from throat to stomach). (2) Rhinoplasty (surgery to change the shape of the nose) or nasal reconstruction with or without septoplasty A) Deformity of skin, bone or cartilage. (B) Creation of new problems, such as perforation of the nasal septum (hole in wall between the right and left halves of the nose) or breathing difficulty. (3) Submucous resection of nasal septum or nasal septoplasty (surgery to remove blockage in or straighten the nose) (A) Persistence, recurrence or worsening of the obstruction. (B) Perforation of nasal septum (hole in wall between the right and left halves of the nose) with dryness and crusting. (C) External deformity of the nose. (4) Sinus surgery/endoscopic sinus surgery (A) Spinal fluid leak (B) Visual loss or other eye injury (C) Numbness in front teeth and palate (D) Loss or reduction in sense of taste or smell (E) Recurrence of disease (F) Empty Nose Syndrome (sensation of nasal congestion, sensation of not being able to take in adequate air through nose) (G) Injury to tear duct causing drainage of tears down the cheek (H) Brain injury and/or infection (I) Injury to nasal septum (J) Nasal obstruction (5) Lung biopsy (A) Air leak with pneumothorax (leak of air from lung to inside of chest causing the lung to collapse) with need for insertion of chest drainage tube into space between lung and chest wall or repeat surgery. -

Hyperbaric Medicine Center During the Actual Questions About the Treatment Process Are Treatment Process, for All Patients’ Confidentiality, No Always Welcomed
Patient Label / Name HBO - HYPERBARIC OXYGEN PATIENT EDUCATION - Page | 1 FAQs HBO is a medical treatment which enhances the body’s natural healing process by inhalation of 100% oxygen in a total body chamber, where atmospheric pressure is WHAT IS HBO? increased and controlled. It is used for a wide variety of treatments usually as an adjunctive part of an overall HBO or HBOT stands for: Hyperbaric Oxygen Therapy medical care plan that can be done on an inpatient or WHAT DOES IT DO? outpatient basis. HBO or HBOT, simply, HBOT is a means of providing WAIT! CAN YOU TELL ME MORE ABOUT THE additional oxygen to your body tissues. “ENTIRELY CLOSED PRESSURE CHAMBER”? HOW DOES IT WORK? Your entire body will go in a closely monitored, TRANSPARENT, 100% ACRYLIC topped, sealed chamber. By exposing the Most patients have plenty of room to get comfortable entire body to and can enjoy their 1.5-2 hour treatments while watching oxygen under TV (installed on each chamber with internal speakers) or increased napping. atmospheric A highly qualified Hyperbaric Tech will be in the room pressure. with you at all times during your treatment, and you will be closely monitored before, during and after all HBO The patient is entirely enclosed in a pressure chamber Treatments. breathing 100% oxygen (O2) at greater than one atmosphere HBO Chambers have microphones that allow your HBO (atm) pressure. Tech to hear you without need to push any buttons. SO, HOW DOES THAT HELP? Simply call out and you will be heard. If you should need to cut your treatment short or want to get out at any HBO therapy serves 4 PRIMARY FUNCTIONS: time, your HBO Tech is always right there to safely decompress the chamber and help you out and call for 1. -
Methacholine Challenge Test 1 2
Methacholine Challenge Test 1 2 What is Methacholine Challenge Test (MCT)? Also, • Do not consume a heavy meal within 2 hours of the test. You can have a light It is a test that measures if your airways narrow after inhaling specific provoking meal e.g. sandwich, soup or salad within 2 hours before the test. agent. The provoking agent used in this test is inhaled methacholine. The degree • Do not wear any tight clothes. of resultant airway narrowing is dependent on each individual’s susceptibility and this airway narrowing will be assessed objectively by measuring the lung function You may also need to stop certain medications before taking the test depending on what clinical questions your physician would like answered based on your MCT changes before and after inhalation of the methacholine in progressively larger results. Different medications have to be stopped at different times before the test doses. Increased airway hyperresponsiveness is usually a hallmark feature of asthma. depending on how long they stay in your body. It is important for you to check with your doctor regarding the safety of stopping Why do I need this operation/procedure? these medications before discontinuing them for the test. Commonly, if you had presented with respiratory symptoms such as shortness of How long before the test? Avoid the following: breath, wheezing, chest tightness or cough, 6weeks Omalizumab your physician may consider doing a MCT to 1week Tiotropium (Spiriva) establish the diagnosis of asthma, especially if 48hours Combination inhalers such as Seretide (fluticasone/ initial lung function tests have not confirmed salmeterol) or Symbicort (budesonide/formoterol) or the diagnosis. -

Lymphangioleiomyomatosis (LAM)
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES Lymphangioleiomyomatosis (LAM) What is LAM? Lymphangioleiomyomatosis (lim-FAN-jee-oh-ly-oh-my-oh-ma- Pneumothroax TOE-sis), also known as LAM, is a rare lung disease that mainly Lung Cysts affects women, usually during their childbearing years. LAM occurs in 3-8 women per million in the general population. LAM is caused by mutations in the tuberous sclerosis complex (TSC) genes. These mutations lead to growth of abnormal cells that spread by the blood stream and make their way into the lungs. Once in the lungs, these cells create holes in the lung tissue (called cysts) that can weaken breathing and the ability to take up oxygen. What are the symptoms of LAM? blood protein called vascular endothelial growth factor-D Symptoms of LAM are similar to other lung diseases. Some (VEGF-D). Elevated VEGF-D levels can help confirm the times patients can be misdiagnosed with asthma, bronchitis, diagnosis of LAM without needing a lung biopsy. Blood or emphysema. These symptoms include: levels of VEGF-D should be checked before doing invasive procedures, such as lung biopsy. ■■ Shortness of breath Lung Biopsy ■■ Fatigue In most (>70%) patients, the diagnosis of LAM can be ■■ Lung collapse, also known as a pneumothorax confirmed based on clinical and/or laboratory findings and ■■ Chest pain does not require a biopsy. However, a lung biopsy may be CLIP AND COPY AND CLIP ■■ Cough needed to confirm the diagnosis of LAM in some cases. ■■ Coughing up small amounts blood There are two ways to do a lung biopsy to diagnose LAM: How is LAM diagnosed and monitored? 1. -

Tracheotomy in COVID-19 Patients: Optimizing Patient Selection and Identifying Prognostic Indicators
Tracheotomy in COVID-19 patients: Optimizing Patient selection and identifying prognostic indicators Stubington T.J.1, Mallick A.S., Garas G.3, Stubington E.4 ,Reddy C.5 , Mansuri M.S.6 1. MBBS BMedSci MRCS(ENT) PGCert (MedEd), Department of Otorhinolaryngology - Head and Neck Surgery, Royal Derby Hospital, Uttoxeter Road, Derby, DE22 3NE, United Kingdom 2. MBBS MRCS (DOHNS) PhD, Department of Otorhinolaryngology - Head and Neck Surgery, Royal Derby Hospital, Uttoxeter Road, Derby, DE22 3NE, United Kingdom 3. PhD FRCS FEBORL-HNS, Department of Otorhinolaryngology - Head and Neck Surgery, Nottingham University Hospitals NHS Trust, Queens Medical Center Campus, Nottingham, NG7 2UH, United Kingdom 4. BSc, Mres, PhD STOR-I Centre for Doctoral Training, Lancaster university, UK 5. MBBS FANZCA, Department of Anaesthesia, Royal Derby Hospital, Uttoxeter Road, Derby, DE22 3NE 6. MBChB, Msc, Dip (RMES), FRCS (ORL), Department of Otorhinolaryngology - Head and Neck Surgery, Royal Derby Hospital, Uttoxeter Road, Derby, DE22 3NE, United Kingdom Corresponding Author: Thomas James Stubington, Dept. Head and Neck Surgery, Royal Derby Hospital, Uttoxeter Road, Derby, DE223NE [email protected] Keywords SARS-CoV-2, Coronavirus, COVID-19, Pandemic, Tracheotomy Word Count: 1787 Abstract Background Tracheotomy, through its ability to wean patients off ventilation, can shorten ICU length of stay and in doing so increase ICU bed capacity, crucial for saving lives during the COVID-19 pandemic. To date, there is a paucity of patient selection criteria and prognosticators to facilitate decision-making and enhance precious ICU capacity. Methods Prospective study of COVID-19 patients undergoing tracheotomy (n=12) over a 4-week period (March-April 2020). -

A Proof-Of-Principle Study of Hyperbaric Oxygen As a Radiosensitizer Prior to Stereotactic Radiosurgery for Brain Metastases
CLINICAL RESEARCH ROTOCOL A proof-of-principle study of hyperbaric oxygen as a radiosensitizer prior to stereotactic radiosurgery for brain metastases Principal Investigator: Alan Hartford, M.D., Ph.D., FACR Section of Radiation Oncology Dartmouth-Hitchcock Medical Center One Medical Center Drive Lebanon, NH 03756 603-650-6600 Co-investigators Jay Buckey, M.D. (hyperbaric medicine) David Gladstone, Sc.D. (radiation physics) Gregory Russo, M.D. (radiation oncology) Clifford Eskey, M.D., Ph.D. (neuroradiology) Arti Gaur, Ph.D. (neurobiology and translational science) Ben Williams, Ph.D. (radiation physics and radiobiology) Biostatistical Support Tor Tosteson, Ph.D. (biostatistics) Zhongze Li, M.S. (biostatistics) Radiology Clifford Eskey, M.D., Ph.D. (neuroradiology) Pathology Research staff Divya Ravi, M.S. Suzanne Vaughn, R.N., O.C.N. Funding Sponsor: NCCC-Clinical Translational Research Program Dartmouth-Hitchcock Medical Center Study Product: Hyperbaric oxygen as radiosensitizer for SRS treatment Protocol Number: D12129 IND Number: Not applicable Initial Version: [7 June 2012] V1 Amended: [07 November 2014] V6 Amended: [17 August 2012] V2 Amended: [20 January 2015] V7 Amended: [25 July 2013] V3 Amended: [18 April 2018] V8 Amended: [28 February 2014] V4 Amended: [11 April 2019] V9 Amended: [17 October 2014] V5 Amended: [17 March 2020] V10 CONFIDENTIAL [HBO – SRS for brain mets] Page ii Version: 10 – 17 March 2020 Table of Contents STUDY SUMMARY..........................................................................................................1 -

Standardisation of Spirometry
Eur Respir J 2005; 26: 319–338 DOI: 10.1183/09031936.05.00034805 CopyrightßERS Journals Ltd 2005 SERIES ‘‘ATS/ERS TASK FORCE: STANDARDISATION OF LUNG FUNCTION TESTING’’ Edited by V. Brusasco, R. Crapo and G. Viegi Number 2 in this Series Standardisation of spirometry M.R. Miller, J. Hankinson, V. Brusasco, F. Burgos, R. Casaburi, A. Coates, R. Crapo, P. Enright, C.P.M. van der Grinten, P. Gustafsson, R. Jensen, D.C. Johnson, N. MacIntyre, R. McKay, D. Navajas, O.F. Pedersen, R. Pellegrino, G. Viegi and J. Wanger CONTENTS AFFILIATIONS Background ............................................................... 320 For affiliations, please see Acknowledgements section FEV1 and FVC manoeuvre .................................................... 321 Definitions . 321 CORRESPONDENCE Equipment . 321 V. Brusasco Requirements . 321 Internal Medicine University of Genoa Display . 321 V.le Benedetto XV, 6 Validation . 322 I-16132 Genova Quality control . 322 Italy Quality control for volume-measuring devices . 322 Fax: 39 103537690 E-mail: [email protected] Quality control for flow-measuring devices . 323 Test procedure . 323 Received: Within-manoeuvre evaluation . 324 March 23 2005 Start of test criteria. 324 Accepted after revision: April 05 2005 End of test criteria . 324 Additional criteria . 324 Summary of acceptable blow criteria . 325 Between-manoeuvre evaluation . 325 Manoeuvre repeatability . 325 Maximum number of manoeuvres . 326 Test result selection . 326 Other derived indices . 326 FEVt .................................................................. 326 Standardisation of FEV1 for expired volume, FEV1/FVC and FEV1/VC.................... 326 FEF25–75% .............................................................. 326 PEF.................................................................. 326 Maximal expiratory flow–volume loops . 326 Definitions. 326 Equipment . 327 Test procedure . 327 Within- and between-manoeuvre evaluation . 327 Flow–volume loop examples. 327 Reversibility testing . 327 Method . -

Expiratory Capnography in Asthma
Eur Respir J, 1994, 7, 318–323 Copyright ERS Journals Ltd 1994 DOI: 10.1183/09031936.94.07020318 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 Expiratory capnography in asthma: B. You*, R. Peslin**, C. Duvivier**, V. Dang Vu*, J.P. Grilliat* Expiratory capnography in asthma: evaluation of various shape indices. B. You, R. *U.M.G., Service de Médecine H, Hôpital Peslin, C. Duvivier, V. Dang Vu, J.P. Grilliat. ERS Journals Ltd 1994. Central, Nancy, France. **INSERM, Unité ABSTRACT: The shape of the capnogram is modified by airway obstruction, and 14, Physiopathologie Respiratoire, Vandœuvre- the evaluation of this deformation, using measurable indices, could allow an indi- les- Nancy, France. rect measurement of bronchial patency. A previous study undertaken in asthmat- Correspondence: B. You ic subjects showed a good correlation between a capnographic index (end-tidal slope) 19 Avenue du Vieux Château and a spirometric parameter (forced expiratory volume in one second as a per- Vandœuvre-les-Nancy centage of predicted (FEV1 %pred)) and suggested the study of other indices. 54500 The correlations between capnographic and spirometric indices were measured France in 10 healthy subjects and 30 asthmatic patients. The usefulness of eight descriptive indices, analysing the successive phases of the capnogram, was assessed by measur- Keywords: Asthma ing their reproducibility and their sensitivity to airway obstruction. The intra- capnography individual and interindividual variabilities (Vi and VI) and the noise/signal ratio carbon dioxide lung function tests (Vi/VI) were measured by comparing the results of two successive capnographic monitoring measurements in 14 asthmatic subjects.