Tracheotomy in COVID-19 Patients: Optimizing Patient Selection and Identifying Prognostic Indicators
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Management of Empysema
Surgical Management of Empysema John A Odell MB ChB, FRCS(Ed), FACS Emeritus Professor of Surgery Mayo Clinic College of Medicine Previously Surgical Director Lung Transplantation ©2013 MFMER | slide-1 Problem case. How would you manage? • 64yr male • Previous RLL bullectomy. • Recent left pneumothorax managed elsewhere with chest tube placement. • Because of continued air-leak talc pleurodesis. • Air-leak continues. ©2013 MFMER | slide-2 • On nasal oxygen. Dyspneic on walking • Significant air-leak. More dyspneic when suction applied to chest drain. • FEV1 40% predicted. DLCO 12% predicted. Options? • Thoracotomy and close air leak surgically • Videothoracoscopy and closure of air-leak • Thoracotomy and decortication • Remove chest drain • List for transplantation Historical Treatment of Emphysema • Abdominal compression belts. The stimulus was the observation that emphysematous patients lean forward when breathing. • Pneumoperitoneum. In an attempt to restore diaphragmatic curvature. • Lungs too large for the chest – costochondrectomy or transverse sternotomy to provide more room. Multiple wedge excisions. • Chest grown too large – thoracoplasty • Pleurodesis. Emphysema results from alveolar wall ischemia. • Phrenectomy. Overvigerous inspiration was ripping alveolar walls. • Hilar denervation. To decrease bronchoconstriction and mucous production mediated by the parasympathetic nervous system. • Whole lung irradiation. To increase elastic recoil by inducing fibrosis. ©2013 MFMER | slide-7 Variants of Emphysema that may be Surgically -

Effect of an Indwelling Pleural Catheter Vs Talc Pleurodesis On
This supplement contains the following items: 1. Original protocol, final protocol, summary of changes. 2. Original statistical analysis plan. There were no further changes to the original statistical analysis plan. Downloaded From: https://jamanetwork.com/ on 10/02/2021 The Australasian Malignant Pleural Effusion Trial (AMPLE) A Multicentre Randomized Study Comparing Indwelling Pleural Catheter vs Talc Pleurodesis in Patients with Malignant Pleural Effusions Ethics Registration number 2012-005 Protocol version number 1.0 Protocol date 10/01/2012 Authorised by: Name: Prof YC Gary Lee Role: Chief Investigator Signature: Date: 10/01/2012 Downloaded From: https://jamanetwork.com/ on 10/02/2021 General Information This document describes the Western Australian Randomised Malignant Effusion trial for the purpose of submission for review by the relevant human research and ethics committees. It provides information about procedures for entering patients into the trial and this protocol should not be used as a guide for the treatment of other patients; every care was taken in its drafting, but corrections or amendments may be necessary. Questions or problems relating to this study should be referred to the Chief Investigator or Trial Coordinator. Compliance The trial will be conducted in compliance with this protocol, the National Statement on Ethical Conduct in Human Research, data protection laws and other guidelines as appropriate. It will be registered with the Australia and New Zealand Clinical Trials Registry, once ethical approval is secured. -

2019 Coding and Payment Information Pleural Effusions and Ascites Management
2019 coding and payment information Pleural effusions and ascites management The information contained in this document, including Reimbursement rates shown are Medicare national the codes supplied, is provided for informational payments for 2019 and do not reflect actual payments purposes only. BD makes no statement, promise or made to individual providers, as payments are adjusted guarantee concerning the appropriateness of any codes specific to particular geographic regions. for a particular procedure, actual levels of All information is subject to change without notice. In reimbursement, payment or charge or that addition, payers or local carriers may have their own reimbursement will be made. coding and billing requirements. Consult your payer This is not intended to be a comprehensive guide to all organization with regard to local reimbursement policies. coding and payment information. 2019 Medicare outpatient facility rates CPT® 2019 APC OPPS 2019 ASC Description APC Status code base rate* base rate Pleural catheter procedures 32550 Insertion of indwelling tunneled pleural catheter 5341 J1 $2,947 $1,790 32552 Removal of indwelling tunneled pleural catheter with cuff 5181 Q2 $620 $319 32560 Instillation via chest tube/catheter, agent for pleurodesis 5181 T $620 N/A 32650 Thoracoscopy, surgical, with pleurodesis (e.g., mechanical or chemical) N/A; inpatient procedure Peritoneal catheter procedures Insertion of tunneled intraperitoneal catheter (e.g., dialysis, intraperitoneal chemotherapy instillation, management of ascites), 49418 -
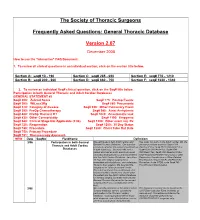
FAQ Document
The Society of Thoracic Surgeons Frequently Asked Questions: General Thoracic Database Version 2.07 December 2008 How to use the “interactive” FAQ Document: 1. To review all clinical questions in an individual section, click on the section title below. Section A: seq# 10 - 190 Section C: seq# 285 - 650 Section E: seq# 770 - 1210 Section B: seq# 200 - 260 Section D: seq# 660 - 750 Section F: seq# 1220 - 1340 2. To review an individual Seq# clinical question, click on the Seq# title below. Participation in both General Thoracic and Adult Cardiac Databases GENERAL STATEMENT #2 Seq# 200: Zubrod Score Seq# 775: Postop Events Seq# 300: WtLoss3Kg Seq# 860: Pneumonia Seq# 310: Category of disease Seq# 930: Other Pulmonary Event Seq# 390: PreOp Chemotherapy Seq# 940: Atrial Arrhythmia Seq# 400: PreOp Thoracic RT Seq# 1020: Anastomotic leak Seq# 430: Other Cormorbidity Seq# 1190: Empyema Seq# 540: Clinical Stage Not Applicable (2.06) Seq# 1200: Other event req. Rx Seq# 725: Reoperation Seq# 1250: 30 Day Status Seq# 740: Procedure Seq# 1280: Chest Tube Out Date Seq# 750: Primary Procedure Seq# 751: Thoracoscopy Approach NEW Date SeqNo FieldName Definition 3/06 Participation in both General We participate in both Adult Cardiac and Yes, enter into both. In the Adult Cardiac DB, the Thoracic and Adult Cardiac General Thoracic Database. Our question primary procedure would be Seq# 1310 pertains to whether the patient should end up OpOCard=Yes; Seq# 2510 ONCAoAn=Yes; Databases in both databases. Scenario--We had a Seq# 2530 ONCArch=Yes; Seq# 2540 patient who had an aortic aneurysm repair ONCDesc=Yes; Seq# 3220 Readm30=Yes; (arch/descending thoracic) and was entered Seq# ReadmRsn=either Pneumonia or other into the Adult Cardiac Database. -

Agenda Item 5
List A (O) Respiratory system treatments and procedures. (1) Biopsy and/or excision (removal) of lesion of larynx, vocal cords, trachea (A) Loss or change of voice. (B) Swallowing or breathing difficulties. (C) Perforation (hole) or fistula (connection) in esophagus (tube from throat to stomach). (2) Rhinoplasty (surgery to change the shape of the nose) or nasal reconstruction with or without septoplasty A) Deformity of skin, bone or cartilage. (B) Creation of new problems, such as perforation of the nasal septum (hole in wall between the right and left halves of the nose) or breathing difficulty. (3) Submucous resection of nasal septum or nasal septoplasty (surgery to remove blockage in or straighten the nose) (A) Persistence, recurrence or worsening of the obstruction. (B) Perforation of nasal septum (hole in wall between the right and left halves of the nose) with dryness and crusting. (C) External deformity of the nose. (4) Sinus surgery/endoscopic sinus surgery (A) Spinal fluid leak (B) Visual loss or other eye injury (C) Numbness in front teeth and palate (D) Loss or reduction in sense of taste or smell (E) Recurrence of disease (F) Empty Nose Syndrome (sensation of nasal congestion, sensation of not being able to take in adequate air through nose) (G) Injury to tear duct causing drainage of tears down the cheek (H) Brain injury and/or infection (I) Injury to nasal septum (J) Nasal obstruction (5) Lung biopsy (A) Air leak with pneumothorax (leak of air from lung to inside of chest causing the lung to collapse) with need for insertion of chest drainage tube into space between lung and chest wall or repeat surgery. -

Hyperbaric Medicine Center During the Actual Questions About the Treatment Process Are Treatment Process, for All Patients’ Confidentiality, No Always Welcomed
Patient Label / Name HBO - HYPERBARIC OXYGEN PATIENT EDUCATION - Page | 1 FAQs HBO is a medical treatment which enhances the body’s natural healing process by inhalation of 100% oxygen in a total body chamber, where atmospheric pressure is WHAT IS HBO? increased and controlled. It is used for a wide variety of treatments usually as an adjunctive part of an overall HBO or HBOT stands for: Hyperbaric Oxygen Therapy medical care plan that can be done on an inpatient or WHAT DOES IT DO? outpatient basis. HBO or HBOT, simply, HBOT is a means of providing WAIT! CAN YOU TELL ME MORE ABOUT THE additional oxygen to your body tissues. “ENTIRELY CLOSED PRESSURE CHAMBER”? HOW DOES IT WORK? Your entire body will go in a closely monitored, TRANSPARENT, 100% ACRYLIC topped, sealed chamber. By exposing the Most patients have plenty of room to get comfortable entire body to and can enjoy their 1.5-2 hour treatments while watching oxygen under TV (installed on each chamber with internal speakers) or increased napping. atmospheric A highly qualified Hyperbaric Tech will be in the room pressure. with you at all times during your treatment, and you will be closely monitored before, during and after all HBO The patient is entirely enclosed in a pressure chamber Treatments. breathing 100% oxygen (O2) at greater than one atmosphere HBO Chambers have microphones that allow your HBO (atm) pressure. Tech to hear you without need to push any buttons. SO, HOW DOES THAT HELP? Simply call out and you will be heard. If you should need to cut your treatment short or want to get out at any HBO therapy serves 4 PRIMARY FUNCTIONS: time, your HBO Tech is always right there to safely decompress the chamber and help you out and call for 1. -

Lymphangioleiomyomatosis (LAM)
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES Lymphangioleiomyomatosis (LAM) What is LAM? Lymphangioleiomyomatosis (lim-FAN-jee-oh-ly-oh-my-oh-ma- Pneumothroax TOE-sis), also known as LAM, is a rare lung disease that mainly Lung Cysts affects women, usually during their childbearing years. LAM occurs in 3-8 women per million in the general population. LAM is caused by mutations in the tuberous sclerosis complex (TSC) genes. These mutations lead to growth of abnormal cells that spread by the blood stream and make their way into the lungs. Once in the lungs, these cells create holes in the lung tissue (called cysts) that can weaken breathing and the ability to take up oxygen. What are the symptoms of LAM? blood protein called vascular endothelial growth factor-D Symptoms of LAM are similar to other lung diseases. Some (VEGF-D). Elevated VEGF-D levels can help confirm the times patients can be misdiagnosed with asthma, bronchitis, diagnosis of LAM without needing a lung biopsy. Blood or emphysema. These symptoms include: levels of VEGF-D should be checked before doing invasive procedures, such as lung biopsy. ■■ Shortness of breath Lung Biopsy ■■ Fatigue In most (>70%) patients, the diagnosis of LAM can be ■■ Lung collapse, also known as a pneumothorax confirmed based on clinical and/or laboratory findings and ■■ Chest pain does not require a biopsy. However, a lung biopsy may be CLIP AND COPY AND CLIP ■■ Cough needed to confirm the diagnosis of LAM in some cases. ■■ Coughing up small amounts blood There are two ways to do a lung biopsy to diagnose LAM: How is LAM diagnosed and monitored? 1. -

A Proof-Of-Principle Study of Hyperbaric Oxygen As a Radiosensitizer Prior to Stereotactic Radiosurgery for Brain Metastases
CLINICAL RESEARCH ROTOCOL A proof-of-principle study of hyperbaric oxygen as a radiosensitizer prior to stereotactic radiosurgery for brain metastases Principal Investigator: Alan Hartford, M.D., Ph.D., FACR Section of Radiation Oncology Dartmouth-Hitchcock Medical Center One Medical Center Drive Lebanon, NH 03756 603-650-6600 Co-investigators Jay Buckey, M.D. (hyperbaric medicine) David Gladstone, Sc.D. (radiation physics) Gregory Russo, M.D. (radiation oncology) Clifford Eskey, M.D., Ph.D. (neuroradiology) Arti Gaur, Ph.D. (neurobiology and translational science) Ben Williams, Ph.D. (radiation physics and radiobiology) Biostatistical Support Tor Tosteson, Ph.D. (biostatistics) Zhongze Li, M.S. (biostatistics) Radiology Clifford Eskey, M.D., Ph.D. (neuroradiology) Pathology Research staff Divya Ravi, M.S. Suzanne Vaughn, R.N., O.C.N. Funding Sponsor: NCCC-Clinical Translational Research Program Dartmouth-Hitchcock Medical Center Study Product: Hyperbaric oxygen as radiosensitizer for SRS treatment Protocol Number: D12129 IND Number: Not applicable Initial Version: [7 June 2012] V1 Amended: [07 November 2014] V6 Amended: [17 August 2012] V2 Amended: [20 January 2015] V7 Amended: [25 July 2013] V3 Amended: [18 April 2018] V8 Amended: [28 February 2014] V4 Amended: [11 April 2019] V9 Amended: [17 October 2014] V5 Amended: [17 March 2020] V10 CONFIDENTIAL [HBO – SRS for brain mets] Page ii Version: 10 – 17 March 2020 Table of Contents STUDY SUMMARY..........................................................................................................1 -

Effectiveness of Chemical Pleurodesis in Spontaneous Pneumothorax
Thorax Online First, published on November 1, 2016 as 10.1136/thoraxjnl-2015-207967 Respiratory research Thorax: first published as 10.1136/thoraxjnl-2015-207967 on 1 November 2016. Downloaded from ORIGINAL ARTICLE Effectiveness of chemical pleurodesis in spontaneous pneumothorax recurrence prevention: a systematic review R J Hallifax,1 A Yousuf,1 H E Jones,2 J P Corcoran,1 I Psallidas,1 N M Rahman1 1Oxford Centre for Respiratory ABSTRACT Medicine, Oxford University Objectives Spontaneous pneumothorax is a common Key messages Hospitals NHS Trust, Oxford, UK pathology. International guidelines suggest pleurodesis 2Faculty of Health Sciences, for non-resolving air leak or recurrence prevention at School of Social and second occurrence. This study comprehensively reviews What is the key question? Community Medicine, the existing literature regarding chemical pleurodesis ▸ How effective are chemical pleurodesis agents University of Bristol, Bristol, UK efficacy. at recurrence prevention in spontaneous Correspondence to Design We systematically reviewed the literature to pneumothorax? Dr Rob J Hallifax, Oxford identify relevant randomised controlled trials (RCTs), Respiratory Trials Unit, case–control studies and case series. We described the What is the bottom line? University of Oxford, Churchill findings of these studies and tabulated relative ▸ Talc poudrage at thoracoscopy and talc or Hospital, Oxford OX3 7LJ, UK; minocycline pleurodesis as an adjunct to [email protected] recurrence rates or ORs (in studies with control groups). Meta-analysis was not performed due to substantial surgery provide low recurrence rates. Less Received 21 October 2015 clinical heterogeneity. invasive options include pleurodesis using Revised 2 August 2016 Results Of 560 abstracts identified by our search tetracycline or ‘blood patch’ via chest drain. -

Lam-Guideline-Pt2.Pdf
AMERICAN THORACIC SOCIETY DOCUMENTS Lymphangioleiomyomatosis Diagnosis and Management: High-Resolution Chest Computed Tomography, Transbronchial Lung Biopsy, and Pleural Disease Management An Official American Thoracic Society/Japanese Respiratory Society Clinical Practice Guideline Nishant Gupta, Geraldine A. Finlay, Robert M. Kotloff, Charlie Strange, Kevin C. Wilson, Lisa R. Young, Angelo M. Taveira-DaSilva, Simon R. Johnson, Vincent Cottin, Steven A. Sahn, Jay H. Ryu, Kuniaki Seyama, Yoshikazu Inoue, Gregory P. Downey, MeiLan K. Han, Thomas V. Colby, Kathryn A. Wikenheiser-Brokamp, Cristopher A. Meyer, Karen Smith, Joel Moss*, and Francis X. McCormack*; on behalf of the ATS Assembly on Clinical Problems THIS OFFICIAL CLINICAL PRACTICE GUIDELINE WAS APPROVED BY THE AMERICAN THORACIC SOCIETY OCTOBER 2017 AND BY THE JAPANESE RESPIRATORY SOCIETY AUGUST 2017 Background: Recommendations regarding key aspects Results: For women who have cystic changes on high-resolution related to the diagnosis and pharmacological treatment of computed tomography of the chest characteristic of LAM, but who have lymphangioleiomyomatosis (LAM) were recently published. We no additional confirmatory features of LAM (i.e., clinical, radiologic, or now provide additional recommendations regarding four specific serologic), the guideline panel made conditional recommendations questions related to the diagnosis of LAM and management of against making a clinical diagnosis of LAM on the basis of the high- pneumothoraces in patients with LAM. resolution computed tomography -

Signs in Chest Imaging
Diagn Interv Radiol 2011; 17:18–29 CHEST IMAGING © Turkish Society of Radiology 2011 PICTORIAL ESSAY Signs in chest imaging Oktay Algın, Gökhan Gökalp, Uğur Topal ABSTRACT adiological practice includes classification of illnesses with similar A radiological sign can sometimes resemble a particular object characteristics through recognizable signs. Knowledge of and abil- or pattern and is often highly suggestive of a group of similar pathologies. Awareness of such similarities can shorten the dif- R ity to recognize these signs can aid the physician in shortening ferential diagnosis list. Many such signs have been described the differential diagnosis list and deciding on the ultimate diagnosis for for X-ray and computed tomography (CT) images. In this ar- ticle, we present the most frequently encountered plain film a patient. In this report, 23 important and frequently seen radiological and CT signs in chest imaging. These signs include for plain signs are presented and described using chest X-rays, computed tomog- films the air bronchogram sign, silhouette sign, deep sulcus raphy (CT) images, illustrations and photographs. sign, Continuous diaphragm sign, air crescent (“meniscus”) sign, Golden S sign, cervicothoracic sign, Luftsichel sign, scim- itar sign, doughnut sign, Hampton hump sign, Westermark Plain films sign, and juxtaphrenic peak sign, and for CT the gloved finger Air bronchogram sign sign, CT halo sign, signet ring sign, comet tail sign, CT an- giogram sign, crazy paving pattern, tree-in-bud sign, feeding Bronchi, which are not normally seen, become visible as a result of vessel sign, split pleura sign, and reversed halo sign. opacification of the lung parenchyma. -

Physicians As Assistants at Surgery: 2016 Update
Physicians as Assistants at Surgery: 2016 Update Participating Organizations: American College of Surgeons American Academy of Ophthalmology American Academy of Orthopaedic Surgeons American Academy of Otolaryngology – Head and Neck Surgery American Association of Neurological Surgeons American Pediatric Surgical Association American Society of Colon and Rectal Surgeons American Society of Plastic Surgeons American Society of Transplant Surgeons American Urological Association Congress of Neurological Surgeons Society for Surgical Oncology Society for Vascular Surgery Society of American Gastrointestinal Endoscopic Surgeons The American College of Obstetricians and Gynecologists The Society of Thoracic Surgeons Physicians as Assistants at Surgery: 2016 Update INTRODUCTION This is the seventh edition of Physicians as Assistants at Surgery, a study first undertaken in 1994 by the American College of Surgeons and other surgical specialty organizations. The study reviews all procedures listed in the “Surgery” section of the 2016 American Medical Association’s Current Procedural Terminology (CPT TM). Each organization was asked to review new codes since 2013 that are applicable to their specialty and determine whether the operation requires the use of a physician as an assistant at surgery: (1) almost always; (2) almost never; or (3) some of the time. The results of this study are presented in the accompanying report, which is in a table format. This table presents information about the need for a physician as an assistant at surgery. Also, please note that an indication that a physician would “almost never” be needed to assist at surgery for some procedures does NOT imply that a physician is never needed. The decision to request that a physician assist at surgery remains the responsibility of the primary surgeon and, when necessary, should be a payable service.