PADI Medical Statement
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Management of Empysema
Surgical Management of Empysema John A Odell MB ChB, FRCS(Ed), FACS Emeritus Professor of Surgery Mayo Clinic College of Medicine Previously Surgical Director Lung Transplantation ©2013 MFMER | slide-1 Problem case. How would you manage? • 64yr male • Previous RLL bullectomy. • Recent left pneumothorax managed elsewhere with chest tube placement. • Because of continued air-leak talc pleurodesis. • Air-leak continues. ©2013 MFMER | slide-2 • On nasal oxygen. Dyspneic on walking • Significant air-leak. More dyspneic when suction applied to chest drain. • FEV1 40% predicted. DLCO 12% predicted. Options? • Thoracotomy and close air leak surgically • Videothoracoscopy and closure of air-leak • Thoracotomy and decortication • Remove chest drain • List for transplantation Historical Treatment of Emphysema • Abdominal compression belts. The stimulus was the observation that emphysematous patients lean forward when breathing. • Pneumoperitoneum. In an attempt to restore diaphragmatic curvature. • Lungs too large for the chest – costochondrectomy or transverse sternotomy to provide more room. Multiple wedge excisions. • Chest grown too large – thoracoplasty • Pleurodesis. Emphysema results from alveolar wall ischemia. • Phrenectomy. Overvigerous inspiration was ripping alveolar walls. • Hilar denervation. To decrease bronchoconstriction and mucous production mediated by the parasympathetic nervous system. • Whole lung irradiation. To increase elastic recoil by inducing fibrosis. ©2013 MFMER | slide-7 Variants of Emphysema that may be Surgically -

Effect of an Indwelling Pleural Catheter Vs Talc Pleurodesis On
This supplement contains the following items: 1. Original protocol, final protocol, summary of changes. 2. Original statistical analysis plan. There were no further changes to the original statistical analysis plan. Downloaded From: https://jamanetwork.com/ on 10/02/2021 The Australasian Malignant Pleural Effusion Trial (AMPLE) A Multicentre Randomized Study Comparing Indwelling Pleural Catheter vs Talc Pleurodesis in Patients with Malignant Pleural Effusions Ethics Registration number 2012-005 Protocol version number 1.0 Protocol date 10/01/2012 Authorised by: Name: Prof YC Gary Lee Role: Chief Investigator Signature: Date: 10/01/2012 Downloaded From: https://jamanetwork.com/ on 10/02/2021 General Information This document describes the Western Australian Randomised Malignant Effusion trial for the purpose of submission for review by the relevant human research and ethics committees. It provides information about procedures for entering patients into the trial and this protocol should not be used as a guide for the treatment of other patients; every care was taken in its drafting, but corrections or amendments may be necessary. Questions or problems relating to this study should be referred to the Chief Investigator or Trial Coordinator. Compliance The trial will be conducted in compliance with this protocol, the National Statement on Ethical Conduct in Human Research, data protection laws and other guidelines as appropriate. It will be registered with the Australia and New Zealand Clinical Trials Registry, once ethical approval is secured. -
2008 June;38(2)
9^k^c\VcY=neZgWVg^XBZY^X^cZKdajbZ(-Cd#'?jcZ'%%- EJGEDH:HD;I=:HD8>:I>:H IdegdbdiZVcY[VX^a^iViZi]ZhijYnd[VaaVheZXihd[jcYZglViZgVcY]neZgWVg^XbZY^X^cZ Idegdk^YZ^c[dgbVi^dcdcjcYZglViZgVcY]neZgWVg^XbZY^X^cZ IdejWa^h]V_djgcVaVcYidXdckZcZbZbWZghd[ZVX]HdX^ZinVccjVaanViVhX^Zci^ÄXXdc[ZgZcXZ HDJI=E68>;>8JC9:GL6I:G :JGDE:6CJC9:GL6I:G6C9 B:9>8>C:HD8>:IN 76GDB:9>86AHD8>:IN D;;>8:=DA9:GH D;;>8:=DA9:GH EgZh^YZci EgZh^YZci 9gB^`Z7ZccZii 1B#7ZccZii5jchl#ZYj#Vj3 Egd[#6a[7gjWV`` 1Va[#d#WgjWV``5cicj#cd3 EVhiçEgZh^YZci K^XZEgZh^YZci 9g8]g^h6Xdii 1XVXdii5deijhcZi#Xdb#Vj3 9gEZiZg<Zgbdceg 1eZiZg#\ZgbdcegZ5b^a#WZ3 HZXgZiVgn >bbZY^ViZEVhiEgZh^YZci 9gHVgV]AdX`aZn 1hejbhhZXgZiVgn5\bV^a#Xdb3 9gCdZb^7^iiZgbVc 1cdZb^W5im#iZX]c^dc#VX#^a3 IgZVhjgZg EVhiEgZh^YZci 9g<jnL^aa^Vbh 1hejbh5[VhibV^a#cZi3 9gGVb^gd8Va^"8dgaZd 1^gdXVa^5YVcZjgdeZ#dg\3 :YjXVi^dcD[ÄXZg =dcdgVgnHZXgZiVgn 9g9Vk^YHbVgi 1YVk^Y#hbVgi5Y]]h#iVh#\dk#Vj3 9g?dZg\HX]bjio 1_dZg\#hX]bjio5]^c#X]3 EjWa^XD[ÄXZg BZbWZgViAVg\Z'%%, 9gKVcZhhV=VaaZg 1kVcZhhV#]VaaZg5XYbX#Xdb#Vj3 9gE]^a7gnhdc 1e]^a#Wgnhdc5YYgX#dg\3 8]V^gbVc6CO=B< BZbWZgViAVg\Z'%%+ 9g9Vk^YHbVgi 1YVk^Y#hbVgi5Y]]h#iVh#\dk#Vj3 Egd[#BV^YZ8^bh^i 1bX^bh^i5^hiVcWja#ZYj#ig3 8dbb^iiZZBZbWZgh BZbWZgViAVg\Z'%%* 9g<aZc=Vl`^ch 1]Vl`ZnZ5hl^[iYha#Xdb#Vj3 9g6gb^c@ZbbZg 1Vgb^c5`ZbbZgh#YZ3 9gHVgV]H]Vg`Zn 1hVgV]#h]Vg`Zn5YZ[ZcXZ#\dk#Vj3 9gHXdiiHfj^gZh 1hXdii#hfj^gZh5YZ[ZcXZ#\dk#Vj3 69B>C>HIG6I>DC 69B>C>HIG6I>DC BZbWZgh]^e =dcdgVgnIgZVhjgZgBZbWZgh]^eHZXgZiVgn HiZkZ<dWaZ 1hejbhVYb5W^\edcY#cZi#Vj3 EVig^X^VLddY^c\ &+7jghZab6kZcjZ!=V^cVjai!>a[dgY B:B7:GH=>E :hhZm!><+(:=!Jc^iZY@^c\Ydb -

Title: Drowning and Therapeutic Hypothermia: Dead Man Walking
Title: Drowning and Therapeutic Hypothermia: Dead Man Walking Author(s): Angela Kavenaugh, D.O., Jamie Cohen, D.O., Jennifer Davis MD FAAP, Department of PICU Affiliation(s): Chris Evert Children’s Hospital, Broward Health Medical Center ABSTRACT BODY: Background: Drowning is the second leading cause of death in children and is associated with severe morbidity and mortality, most often due to hypoxic-ischemic encephalopathy. Those that survive are often left with debilitating neurological deficits. Therapeutic Hypothermia after resuscitation from ventricular fibrillation or pulseless ventricular tachycardia induced cardiac arrest is the standard of care in adults and has also been proven to have beneficial effects that persist into early childhood when utilized in neonatal birth asphyxia, but has yet to be accepted into practice for pediatrics. Objective: To present supportive evidence that Therapeutic Hypothermia improves mortality and morbidity specifically for pediatric post drowning patients. Case Report: A five year old male presented to the Emergency Department after pool submersion of unknown duration. He was found to have asphyxial cardiac arrest and received bystander CPR, which was continued by EMS for a total of 10 minutes, including 2 doses of epinephrine. CPR continued into the emergency department. Upon presentation to the ED, he was found to have fixed and dilated pupils, unresponsiveness, with a GCS of 3. Upon initial pulse check was found to have return of spontaneous circulation, with sinus tachycardia. His blood gas revealed 6.86/45/477/8/-25. He was intubated, given 2 normal saline boluses and 2 mEq/kg of Sodium Bicarbonate. The initial head CT was normal. -

2019 Coding and Payment Information Pleural Effusions and Ascites Management
2019 coding and payment information Pleural effusions and ascites management The information contained in this document, including Reimbursement rates shown are Medicare national the codes supplied, is provided for informational payments for 2019 and do not reflect actual payments purposes only. BD makes no statement, promise or made to individual providers, as payments are adjusted guarantee concerning the appropriateness of any codes specific to particular geographic regions. for a particular procedure, actual levels of All information is subject to change without notice. In reimbursement, payment or charge or that addition, payers or local carriers may have their own reimbursement will be made. coding and billing requirements. Consult your payer This is not intended to be a comprehensive guide to all organization with regard to local reimbursement policies. coding and payment information. 2019 Medicare outpatient facility rates CPT® 2019 APC OPPS 2019 ASC Description APC Status code base rate* base rate Pleural catheter procedures 32550 Insertion of indwelling tunneled pleural catheter 5341 J1 $2,947 $1,790 32552 Removal of indwelling tunneled pleural catheter with cuff 5181 Q2 $620 $319 32560 Instillation via chest tube/catheter, agent for pleurodesis 5181 T $620 N/A 32650 Thoracoscopy, surgical, with pleurodesis (e.g., mechanical or chemical) N/A; inpatient procedure Peritoneal catheter procedures Insertion of tunneled intraperitoneal catheter (e.g., dialysis, intraperitoneal chemotherapy instillation, management of ascites), 49418 -
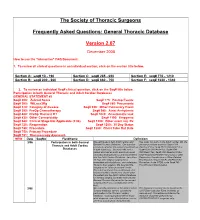
FAQ Document
The Society of Thoracic Surgeons Frequently Asked Questions: General Thoracic Database Version 2.07 December 2008 How to use the “interactive” FAQ Document: 1. To review all clinical questions in an individual section, click on the section title below. Section A: seq# 10 - 190 Section C: seq# 285 - 650 Section E: seq# 770 - 1210 Section B: seq# 200 - 260 Section D: seq# 660 - 750 Section F: seq# 1220 - 1340 2. To review an individual Seq# clinical question, click on the Seq# title below. Participation in both General Thoracic and Adult Cardiac Databases GENERAL STATEMENT #2 Seq# 200: Zubrod Score Seq# 775: Postop Events Seq# 300: WtLoss3Kg Seq# 860: Pneumonia Seq# 310: Category of disease Seq# 930: Other Pulmonary Event Seq# 390: PreOp Chemotherapy Seq# 940: Atrial Arrhythmia Seq# 400: PreOp Thoracic RT Seq# 1020: Anastomotic leak Seq# 430: Other Cormorbidity Seq# 1190: Empyema Seq# 540: Clinical Stage Not Applicable (2.06) Seq# 1200: Other event req. Rx Seq# 725: Reoperation Seq# 1250: 30 Day Status Seq# 740: Procedure Seq# 1280: Chest Tube Out Date Seq# 750: Primary Procedure Seq# 751: Thoracoscopy Approach NEW Date SeqNo FieldName Definition 3/06 Participation in both General We participate in both Adult Cardiac and Yes, enter into both. In the Adult Cardiac DB, the Thoracic and Adult Cardiac General Thoracic Database. Our question primary procedure would be Seq# 1310 pertains to whether the patient should end up OpOCard=Yes; Seq# 2510 ONCAoAn=Yes; Databases in both databases. Scenario--We had a Seq# 2530 ONCArch=Yes; Seq# 2540 patient who had an aortic aneurysm repair ONCDesc=Yes; Seq# 3220 Readm30=Yes; (arch/descending thoracic) and was entered Seq# ReadmRsn=either Pneumonia or other into the Adult Cardiac Database. -

Agenda Item 5
List A (O) Respiratory system treatments and procedures. (1) Biopsy and/or excision (removal) of lesion of larynx, vocal cords, trachea (A) Loss or change of voice. (B) Swallowing or breathing difficulties. (C) Perforation (hole) or fistula (connection) in esophagus (tube from throat to stomach). (2) Rhinoplasty (surgery to change the shape of the nose) or nasal reconstruction with or without septoplasty A) Deformity of skin, bone or cartilage. (B) Creation of new problems, such as perforation of the nasal septum (hole in wall between the right and left halves of the nose) or breathing difficulty. (3) Submucous resection of nasal septum or nasal septoplasty (surgery to remove blockage in or straighten the nose) (A) Persistence, recurrence or worsening of the obstruction. (B) Perforation of nasal septum (hole in wall between the right and left halves of the nose) with dryness and crusting. (C) External deformity of the nose. (4) Sinus surgery/endoscopic sinus surgery (A) Spinal fluid leak (B) Visual loss or other eye injury (C) Numbness in front teeth and palate (D) Loss or reduction in sense of taste or smell (E) Recurrence of disease (F) Empty Nose Syndrome (sensation of nasal congestion, sensation of not being able to take in adequate air through nose) (G) Injury to tear duct causing drainage of tears down the cheek (H) Brain injury and/or infection (I) Injury to nasal septum (J) Nasal obstruction (5) Lung biopsy (A) Air leak with pneumothorax (leak of air from lung to inside of chest causing the lung to collapse) with need for insertion of chest drainage tube into space between lung and chest wall or repeat surgery. -
The Post-Mortem Appearances in Cases of Asphyxia Caused By
a U?UST 1902.1 ASPHYXIA CAUSED BY DROWNING 297 Table I. Shows the occurrence of fluid and mud in the 55 fresh bodies. ?ritfinal Jlrttclcs. Fluid. Mud. Air-passage ... .... 20 2 ? ? and stomach ... ig 6 ? ? stomach and intestine ... 7 1 ? ? and intestine X ??? Stomach ... ??? THE POST-MORTEM APPEARANCES IN Intestine ... ... 1 Stomach and intestine ... ... i CASES OF ASPHYXIA CAUSED BY DROWNING. Total 46 9 = 55 By J. B. GIBBONS, From the above table it will be seen that fluid was in the alone in 20 LIEUT.-COL., I.M.S., present air-passage cases, in the air-passage and stomach in sixteen, Lute Police-Surgeon, Calcutta, Civil Surgeon, Ilowrah. in the air-passage, stomach and intestine in seven, in the air-passage and intestine in one. As used in this table the term includes frothy and non- frothy fluid. Frothy fluid is only to be expected In the period from June 1893 to November when the has been quickly recovered from months which I body 1900, excluding three during the water in which drowning took place and cases on leave, 15/ of was privilege asphyxia examined without delay. In some of my cases were examined me in the due to drowning by it was present in a most typical form; there was For the of this Calcutta Morgue. purpose a bunch of fine lathery froth about the nostrils, all cases of death inhibition paper I exclude by and the respiratory tract down to the bronchi due to submersion and all cases of or syncope was filled with it. received after into death from injuries falling The quantity of fluid in the air-passage varies the water. -

Respiratory Physiology for the Anesthesiologist
REVIEW ARTICLE Deborah J. Culley, M.D., Editor ABSTRACT Respiratory function is fundamental in the practice of anesthesia. Knowledge of basic physiologic principles of respiration assists in the proper implemen- tation of daily actions of induction and maintenance of general anesthesia, Respiratory Physiology delivery of mechanical ventilation, discontinuation of mechanical and pharma- cologic support, and return to the preoperative state. The current work pro- Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/130/6/1064/455191/20190600_0-00035.pdf by guest on 24 September 2021 for the Anesthesiologist vides a review of classic physiology and emphasizes features important to the anesthesiologist. The material is divided in two main sections, gas exchange Luca Bigatello, M.D., Antonio Pesenti, M.D. and respiratory mechanics; each section presents the physiology as the basis ANESTHESIOLOGY 2019; 130:1064–77 of abnormal states. We review the path of oxygen from air to the artery and of carbon dioxide the opposite way, and we have the causes of hypoxemia and of hypercarbia based on these very footpaths. We present the actions nesthesiologists take control of the respiratory func- of pressure, flow, and volume as the normal determinants of ventilation, and Ation of millions of patients throughout the world each we review the resulting abnormalities in terms of changes of resistance and day. We learn to maintain gas exchange and use respiration compliance. to administer anesthetic gases through the completion of (ANESTHESIOLOGY 2019; 130:1064–77) surgery, when we return this vital function to its legitimate owners, ideally with a seamless transition to a healthy post- operative course. -

MECAP News April 2021
U.S. Consumer Product Safety Commission MECAPnews MEDICAL EXAMINERS AND CORONERS ALERT PROJECT April 2021 MECAP Reports | Page 2 Asphyxia/Suffocation Carbon Monoxide Poisoning Submersion MECAP Reports | Page 3 Fire All-Terrain Vehicles (ATVs) Electrocution Fatalities Involving Other Hazards MECAP Contact | Page 4 The following pages summarize MECAP reports Yolanda Nash received by CPSC selected for follow-up Program Analyst investigation. The entries include a brief Division of Hazard and Injury Data description of the incident to illustrate the type and Systems Directorate for Epidemiology nature of the reported fatalities. This important information helps CPSC carry out its mission to U.S. Consumer Product Safety protect the public from product-related injuries and Commission deaths. 4330 East-West Highway Bethesda, MD We appreciate your support; please continue to 20814 report your product-related cases to us. [email protected] 1-800-638-8095 x7502 or 301-504-7502 *Cases selected for CPSC follow-up investigation Asphyxiation/ down to sleep in a toddler basement stairs. The Suffocation bed with multiple heavy electric power had been blankets. The next morning, shut off, and the generator *A 7-year-old female was the mother found the was used to provide power. discovered by her mother decedent positioned face EMS measured the carbon unresponsive in bed with a down in the soft bedding monoxide level at 500 ppm. balloon pulled over her face. and blankets. Despite The cause of death was The decedent became emergency efforts, the carbon monoxide poisoning. entangled with a helium infant was pronounced dead balloon tied to her bed and at the hospital. -

SCUBA Medical Statement
MEDICAL STATEMENT Participant Record (Confidential Information) Please read carefully before signing. This is a statement in which you are informed of some potential risks established safety procedures are not followed, however, there are involved in scuba diving and of the conduct required of you during the increased risks. scuba training program. Your signature on this statement is required for To scuba dive safely, you should not be extremely overweight or you to participate in the scuba training program offered out of condition. Diving can be strenuous under certain conditions. Your respiratory and circulatory systems must be in good health. All body air by STAFF and spaces must be normal and healthy. A person with coronary disease, a Instructor current cold or congestion, epilepsy, a severe medical problem or who is under the influence of alcohol or drugs should not dive. If you have GEORGIA TECH CAMPUS RECREATION CENTER located in the asthma, heart disease, other chronic medical conditions or you are tak- Facility ing medications on a regular basis, you should consult your doctor and the instructor before participating in this program, and on a regular basis city of ATLANTA , state/province of GEORGIA . thereafter upon completion. You will also learn from the instructor the important safety rules regarding breathing and equalization while scuba Read this statement prior to signing it. You must complete this diving. Improper use of scuba equipment can result in serious injury. You Medical Statement, which includes the medical questionnaire section, to must be thoroughly instructed in its use under direct supervision of a enroll in the scuba training program. -

Brownie's THIRD LUNG
BrMARINEownie GROUP’s Owner’s Manual Variable Speed Hand Carry Hookah Diving System ADVENTURE IS ALWAYS ON THE LINE! VSHCDC Systems This manual is also available online 3001 NW 25th Avenue, Pompano Beach, FL 33069 USA Ph +1.954.462.5570 Fx +1.954.462.6115 www.BrowniesMarineGroup.com CONGRATULATIONS ON YOUR PURCHASE OF A BROWNIE’S SYSTEM You now have in your possession the finest, most reliable, surface supplied breathing air system available. The operation is designed with your safety and convenience in mind, and by carefully reading this brief manual you can be assured of many hours of trouble-free enjoyment. READ ALL SAFETY RULES AND OPERATING INSTRUCTIONS CONTAINED IN THIS MANUAL AND FOLLOW THEM WITH EACH USE OF THIS PRODUCT. MANUAL SAFETY NOTICES Important instructions concerning the endangerment of personnel, technical safety or operator safety will be specially emphasized in this manual by placing the information in the following types of safety notices. DANGER DANGER INDICATES AN IMMINENTLY HAZARDOUS SITUATION WHICH, IF NOT AVOIDED, WILL RESULT IN DEATH OR SERIOUS INJURY. THIS IS LIMITED TO THE MOST EXTREME SITUATIONS. WARNING WARNING INDICATES A POTENTIALLY HAZARDOUS SITUATION WHICH, IF NOT AVOIDED, COULD RESULT IN DEATH OR INJURY. CAUTION CAUTION INDICATES A POTENTIALLY HAZARDOUS SITUATION WHICH, IF NOT AVOIDED, MAY RESULT IN MINOR OR MODERATE INJURY. IT MAY ALSO BE USED TO ALERT AGAINST UNSAFE PRACTICES. NOTE NOTE ADVISE OF TECHNICAL REQUIREMENTS THAT REQUIRE PARTICULAR ATTENTION BY THE OPERATOR OR THE MAINTENANCE TECHNICIAN FOR PROPER MAINTENANCE AND UTILIZATION OF THE EQUIPMENT. REGISTER YOUR PRODUCT ONLINE Go to www.BrowniesMarineGroup.com to register your product.