2008 December;38(4)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Management of Empysema
Surgical Management of Empysema John A Odell MB ChB, FRCS(Ed), FACS Emeritus Professor of Surgery Mayo Clinic College of Medicine Previously Surgical Director Lung Transplantation ©2013 MFMER | slide-1 Problem case. How would you manage? • 64yr male • Previous RLL bullectomy. • Recent left pneumothorax managed elsewhere with chest tube placement. • Because of continued air-leak talc pleurodesis. • Air-leak continues. ©2013 MFMER | slide-2 • On nasal oxygen. Dyspneic on walking • Significant air-leak. More dyspneic when suction applied to chest drain. • FEV1 40% predicted. DLCO 12% predicted. Options? • Thoracotomy and close air leak surgically • Videothoracoscopy and closure of air-leak • Thoracotomy and decortication • Remove chest drain • List for transplantation Historical Treatment of Emphysema • Abdominal compression belts. The stimulus was the observation that emphysematous patients lean forward when breathing. • Pneumoperitoneum. In an attempt to restore diaphragmatic curvature. • Lungs too large for the chest – costochondrectomy or transverse sternotomy to provide more room. Multiple wedge excisions. • Chest grown too large – thoracoplasty • Pleurodesis. Emphysema results from alveolar wall ischemia. • Phrenectomy. Overvigerous inspiration was ripping alveolar walls. • Hilar denervation. To decrease bronchoconstriction and mucous production mediated by the parasympathetic nervous system. • Whole lung irradiation. To increase elastic recoil by inducing fibrosis. ©2013 MFMER | slide-7 Variants of Emphysema that may be Surgically -

Effect of an Indwelling Pleural Catheter Vs Talc Pleurodesis On
This supplement contains the following items: 1. Original protocol, final protocol, summary of changes. 2. Original statistical analysis plan. There were no further changes to the original statistical analysis plan. Downloaded From: https://jamanetwork.com/ on 10/02/2021 The Australasian Malignant Pleural Effusion Trial (AMPLE) A Multicentre Randomized Study Comparing Indwelling Pleural Catheter vs Talc Pleurodesis in Patients with Malignant Pleural Effusions Ethics Registration number 2012-005 Protocol version number 1.0 Protocol date 10/01/2012 Authorised by: Name: Prof YC Gary Lee Role: Chief Investigator Signature: Date: 10/01/2012 Downloaded From: https://jamanetwork.com/ on 10/02/2021 General Information This document describes the Western Australian Randomised Malignant Effusion trial for the purpose of submission for review by the relevant human research and ethics committees. It provides information about procedures for entering patients into the trial and this protocol should not be used as a guide for the treatment of other patients; every care was taken in its drafting, but corrections or amendments may be necessary. Questions or problems relating to this study should be referred to the Chief Investigator or Trial Coordinator. Compliance The trial will be conducted in compliance with this protocol, the National Statement on Ethical Conduct in Human Research, data protection laws and other guidelines as appropriate. It will be registered with the Australia and New Zealand Clinical Trials Registry, once ethical approval is secured. -

ANZHMG) & the Hyperbaric Technicians and Nurses Association (HTNA)
The Australian and New Zealand Hyperbaric Medicine Group (ANZHMG) & The Hyperbaric Technicians and Nurses Association (HTNA) COVID-19 Guidelines 1 | ANZHMG/HTNA COVID - 19 v1.1 2020 - 03- 27 Published by the South Pacific Underwater Medicine Society (SPUMS), c/- Australian and New Zealand College of Anaesthetists (ANZCA), 630 St Kilda Road, Melbourne VIC 3004, Australia. E-mail: [email protected] Website: spums.org.au This document is based upon the Australian and New Zealand Intensive Care Society (2020) ANZICS COVID-19 Guidelines. Melbourne: ANZICS, with permission. THE ANZHMG/HTNA COVID-19 Working Group gratefully acknowledge the kindness of the Australian & New Zealand Intensive Care Society in permitting the use of their guidelines as a template for our own. © Australian and New Zealand Hyperbaric Medicine Group 2020. Not for sale. This work may be reproduced, free of charge, in whole or in part for clinical, study, training, research or any other fair purpose, subject to the inclusion of an acknowledgment of the source. SPUMS requests that you attribute this publication (and any material sourced from it) using the following citation: Australian and New Zealand Hyperbaric Medicine Group and the Hyperbaric Technicians and Nurses Association (2020), ANZHMG/HTNA COVID-19 Guidelines. Melbourne: SPUMS. Disclaimer The Australian and New Zealand Hyperbaric Medicine Group (ANZHMG) and Hyperbaric Technicians and Nurses Association (HTNA) COVID-19 Guidelines have been developed to assist hyperbaric clinicians prepare and plan for the maintenance of hyperbaric services during a pandemic, and provide a safe working environment for staff and patients. Considerable effort has been made to ensure the information contained within the recommendations is correct at the time of publication. -

Nursing in a Critical Care Hyperbaric Unit at Merida, Yucatan, Mexico: Report of a Case of an Acute Pediatric Burn Patient
Case Report Page 1 of 6 Nursing in a critical care hyperbaric unit at Merida, Yucatan, Mexico: report of a case of an acute pediatric burn patient Judith Ruiz-Aguilar, Rodrigo Diaz-Ibañez, E. Cuauhtemoc Sanchez-Rodriguez Hyperbaric Medicine Service, Hospital Centro de Especialidades Médicas del Sureste (CEM) and Hospital Agustín O’Horan, Merida, Yucatan, Mexico Correspondence to: Judith Ruiz-Aguilar, RN, MEd. Chief of Nursing, Hyperbaric Medicine Service, Hospital Centro de Especialidades Médicas del Sureste (CEM) and Hospital Agustín O’Horan, Merida, Yucatan, Mexico. Email: [email protected]. Abstract: Hyperbaric oxygen therapy (HBOT) for intensive care unit (ICU) patients places special technical and knowledge-based skills demands on nurses inside hyperbaric chambers. Probably the best clinical contributions of HBOT are in the acute cases, in the ischemia reperfusion injury. Nevertheless in the last years, hyperbaric units have focused more in chronic wounds. The first golden rule to treat an ICU patient in a hyperbaric chamber is that you can maintain the same quality of care inside the chamber as in the ICU. This means that the hyperbaric unit has to have the technology means as well as the proficiency and competency of its personnel to provide intensive care inside the chamber. These require competent nursing personnel. We present a case of a 5-year-old pediatric patient who suffered a deep second-degree thermal burn that compromised 32% of the total body surface; including the face, neck, thorax and both arms. The patient received medical support, HBOT and daily wound care. He received a total of 14 treatments and underwent complete healing of the burned areas. -

2019 Coding and Payment Information Pleural Effusions and Ascites Management
2019 coding and payment information Pleural effusions and ascites management The information contained in this document, including Reimbursement rates shown are Medicare national the codes supplied, is provided for informational payments for 2019 and do not reflect actual payments purposes only. BD makes no statement, promise or made to individual providers, as payments are adjusted guarantee concerning the appropriateness of any codes specific to particular geographic regions. for a particular procedure, actual levels of All information is subject to change without notice. In reimbursement, payment or charge or that addition, payers or local carriers may have their own reimbursement will be made. coding and billing requirements. Consult your payer This is not intended to be a comprehensive guide to all organization with regard to local reimbursement policies. coding and payment information. 2019 Medicare outpatient facility rates CPT® 2019 APC OPPS 2019 ASC Description APC Status code base rate* base rate Pleural catheter procedures 32550 Insertion of indwelling tunneled pleural catheter 5341 J1 $2,947 $1,790 32552 Removal of indwelling tunneled pleural catheter with cuff 5181 Q2 $620 $319 32560 Instillation via chest tube/catheter, agent for pleurodesis 5181 T $620 N/A 32650 Thoracoscopy, surgical, with pleurodesis (e.g., mechanical or chemical) N/A; inpatient procedure Peritoneal catheter procedures Insertion of tunneled intraperitoneal catheter (e.g., dialysis, intraperitoneal chemotherapy instillation, management of ascites), 49418 -
FAQ Document
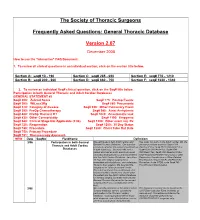
The Society of Thoracic Surgeons Frequently Asked Questions: General Thoracic Database Version 2.07 December 2008 How to use the “interactive” FAQ Document: 1. To review all clinical questions in an individual section, click on the section title below. Section A: seq# 10 - 190 Section C: seq# 285 - 650 Section E: seq# 770 - 1210 Section B: seq# 200 - 260 Section D: seq# 660 - 750 Section F: seq# 1220 - 1340 2. To review an individual Seq# clinical question, click on the Seq# title below. Participation in both General Thoracic and Adult Cardiac Databases GENERAL STATEMENT #2 Seq# 200: Zubrod Score Seq# 775: Postop Events Seq# 300: WtLoss3Kg Seq# 860: Pneumonia Seq# 310: Category of disease Seq# 930: Other Pulmonary Event Seq# 390: PreOp Chemotherapy Seq# 940: Atrial Arrhythmia Seq# 400: PreOp Thoracic RT Seq# 1020: Anastomotic leak Seq# 430: Other Cormorbidity Seq# 1190: Empyema Seq# 540: Clinical Stage Not Applicable (2.06) Seq# 1200: Other event req. Rx Seq# 725: Reoperation Seq# 1250: 30 Day Status Seq# 740: Procedure Seq# 1280: Chest Tube Out Date Seq# 750: Primary Procedure Seq# 751: Thoracoscopy Approach NEW Date SeqNo FieldName Definition 3/06 Participation in both General We participate in both Adult Cardiac and Yes, enter into both. In the Adult Cardiac DB, the Thoracic and Adult Cardiac General Thoracic Database. Our question primary procedure would be Seq# 1310 pertains to whether the patient should end up OpOCard=Yes; Seq# 2510 ONCAoAn=Yes; Databases in both databases. Scenario--We had a Seq# 2530 ONCArch=Yes; Seq# 2540 patient who had an aortic aneurysm repair ONCDesc=Yes; Seq# 3220 Readm30=Yes; (arch/descending thoracic) and was entered Seq# ReadmRsn=either Pneumonia or other into the Adult Cardiac Database. -

Safety Manual Program/Monthly Safety Awearness
2014 Safety Manual/Monthly Safety Awareness Program Serena Group Hyperbaric Medicine Centers Page 1 Confidential and Proprietary Information SerenaGroup Hyperbaric Medical Center Do not copy or distribute 2014 Fire Safety Plan 1. Purpose To provide hyperbaric personnel a predetermined plan in the event of a fire in the hyperbaric area in order to reduce injury and/or catastrophic outcomes. 2. Policy 2.1. In the event of an emergency, the Hyperbaric Medicine Center personnel will be prepared to respond. 2.2. The Safety Director shall be designated by the Program Director / Manager or designee. NOTE: NFPA 99 Health Care Facilities, 1999 edition, (page 131) “19-3.1.3.2 A safety director shall be designated in charge of all hyperbaric equipment. The safety director shall work closely with facility management personnel and the hyperbaric physician(s) to establish procedures for safe operation and maintenance of the hyperbaric facility. He or she shall make necessary recommendations for departmental safety policies and procedures. The safety director shall have the authority to restrict or remove any potentially hazardous supply or equipment items from the chamber.” 2.3. Each plan shall be collaboratively developed with the hospital fire safety policy in conjunction with NFPA standards. 2.4. There will be no smoking or open flames in the hyperbaric area. 2.5. The area will be kept exceptionally clean and free of fire hazards according to the NGPA for Hyperbaric health care facilities. 2.6. The chamber itself will be kept exceptionally clean of lint and dust particles as these are hazardous when inside the chamber. -

(ANZHMG) & the Hyperbaric Technicians and Nurses Association
The Australian and New Zealand Hyperbaric Medicine Group (ANZHMG) & The Hyperbaric Technicians and Nurses Association (HTNA) COVID-19 Guidelines 1 | ANZHMG/HTNA COVID - 19 v1.1 2020 - 03- 27 Published by the South Pacific Underwater Medicine Society (SPUMS), c/- Australian and New Zealand College of Anaesthetists (ANZCA), 630 St Kilda Road, Melbourne VIC 3004, Australia. E-mail: [email protected] Website: spums.org.au This document is based upon the Australian and New Zealand Intensive Care Society (2020) ANZICS COVID-19 Guidelines. Melbourne: ANZICS, with permission. THE ANZHMG/HTNA COVID-19 Working Group gratefully acknowledge the kindness of the Australian & New Zealand Intensive Care Society in permitting the use of their guidelines as a template for our own. © Australian and New Zealand Hyperbaric Medicine Group 2020. Not for sale. This work may be reproduced, free of charge, in whole or in part for clinical, study, training, research or any other fair purpose, subject to the inclusion of an acknowledgment of the source. SPUMS requests that you attribute this publication (and any material sourced from it) using the following citation: Australian and New Zealand Hyperbaric Medicine Group and the Hyperbaric Technicians and Nurses Association (2020), ANZHMG/HTNA COVID-19 Guidelines. Melbourne: SPUMS. Disclaimer The Australian and New Zealand Hyperbaric Medicine Group (ANZHMG) and Hyperbaric Technicians and Nurses Association (HTNA) COVID-19 Guidelines have been developed to assist hyperbaric clinicians prepare and plan for the maintenance of hyperbaric services during a pandemic, and provide a safe working environment for staff and patients. Considerable effort has been made to ensure the information contained within the recommendations is correct at the time of publication. -

Agenda Item 5
List A (O) Respiratory system treatments and procedures. (1) Biopsy and/or excision (removal) of lesion of larynx, vocal cords, trachea (A) Loss or change of voice. (B) Swallowing or breathing difficulties. (C) Perforation (hole) or fistula (connection) in esophagus (tube from throat to stomach). (2) Rhinoplasty (surgery to change the shape of the nose) or nasal reconstruction with or without septoplasty A) Deformity of skin, bone or cartilage. (B) Creation of new problems, such as perforation of the nasal septum (hole in wall between the right and left halves of the nose) or breathing difficulty. (3) Submucous resection of nasal septum or nasal septoplasty (surgery to remove blockage in or straighten the nose) (A) Persistence, recurrence or worsening of the obstruction. (B) Perforation of nasal septum (hole in wall between the right and left halves of the nose) with dryness and crusting. (C) External deformity of the nose. (4) Sinus surgery/endoscopic sinus surgery (A) Spinal fluid leak (B) Visual loss or other eye injury (C) Numbness in front teeth and palate (D) Loss or reduction in sense of taste or smell (E) Recurrence of disease (F) Empty Nose Syndrome (sensation of nasal congestion, sensation of not being able to take in adequate air through nose) (G) Injury to tear duct causing drainage of tears down the cheek (H) Brain injury and/or infection (I) Injury to nasal septum (J) Nasal obstruction (5) Lung biopsy (A) Air leak with pneumothorax (leak of air from lung to inside of chest causing the lung to collapse) with need for insertion of chest drainage tube into space between lung and chest wall or repeat surgery. -

June 18-20, 2015 Annual Scientific Meeting
UNDERSEA & HYPERBARIC MEDICAL SOCIETY ANNUAL SCIENTIFIC MEETING HOTEL BONAVENTURE MONTREAL, CANADA JUNE 18-20, 2015 2015 UHMS Scientific Meeting June 18-20 Montreal, Canada TABLE OF CONTENTS Subject Page No. Disclosures ................................................................................................................................................................ 6-7 Schedule .................................................................................................................................................................. 8-13 Continuing Education ................................................................................................................................................ 13 Associates’ Breakout Schedule .................................................................................................................................. 14 Evaluation / MOC Credit Information ....................................................................................................................... 15 Committee Meetings .................................................................................................................................................. 16 Exhibitors .............................................................................................................................................................. 17-20 SESSIONS/ABSTRACTS THURSDAY GENERAL SESSION .............................................................................................................. 22-63 PRESIDENT’S -

Hyperbaric Medicine Center During the Actual Questions About the Treatment Process Are Treatment Process, for All Patients’ Confidentiality, No Always Welcomed
Patient Label / Name HBO - HYPERBARIC OXYGEN PATIENT EDUCATION - Page | 1 FAQs HBO is a medical treatment which enhances the body’s natural healing process by inhalation of 100% oxygen in a total body chamber, where atmospheric pressure is WHAT IS HBO? increased and controlled. It is used for a wide variety of treatments usually as an adjunctive part of an overall HBO or HBOT stands for: Hyperbaric Oxygen Therapy medical care plan that can be done on an inpatient or WHAT DOES IT DO? outpatient basis. HBO or HBOT, simply, HBOT is a means of providing WAIT! CAN YOU TELL ME MORE ABOUT THE additional oxygen to your body tissues. “ENTIRELY CLOSED PRESSURE CHAMBER”? HOW DOES IT WORK? Your entire body will go in a closely monitored, TRANSPARENT, 100% ACRYLIC topped, sealed chamber. By exposing the Most patients have plenty of room to get comfortable entire body to and can enjoy their 1.5-2 hour treatments while watching oxygen under TV (installed on each chamber with internal speakers) or increased napping. atmospheric A highly qualified Hyperbaric Tech will be in the room pressure. with you at all times during your treatment, and you will be closely monitored before, during and after all HBO The patient is entirely enclosed in a pressure chamber Treatments. breathing 100% oxygen (O2) at greater than one atmosphere HBO Chambers have microphones that allow your HBO (atm) pressure. Tech to hear you without need to push any buttons. SO, HOW DOES THAT HELP? Simply call out and you will be heard. If you should need to cut your treatment short or want to get out at any HBO therapy serves 4 PRIMARY FUNCTIONS: time, your HBO Tech is always right there to safely decompress the chamber and help you out and call for 1. -

The Kent Hospital Wound Recovery and Hyperbaric Medicine Center: a Brief Overview, 1998–2013
CONTRIBUTION The Kent Hospital Wound Recovery and Hyperbaric Medicine Center: A Brief Overview, 1998–2013 LISA J. GOULD, MD, PhD; CATHERINE DECIANTIS, RN, CHRN; RONALD P. ZINNO, MD; GEORGE A. PERDRIZET, MD, PhD 13 17 EN ABSTRACT cannot devote the necessary time and effort required in the A brief description of the Wound Recovery and Hyperbaric management of these patients. Wound centers add value to Medicine Center, now in its second decade of service, the institutions and communities in which they serve. will inform the general medical community of this As the field has expanded, the science of chronic wound valuable asset. care has also grown. The increased utilization of hyperbaric Demand for wound care services is predicted to grow oxygen therapy (HBOT) is one example of this new growth. steadily over the next several decades. Kent Hospital’s vi- Approximately 10-15% of patients presenting to wound care sion for wound care is embodied in its thriving Wound centers will qualify for HBOT. Oxygen deficiency is a criti- Recovery and Hyperbaric Medicine Center. New cost- cal component of many wound types for which HBOT may effective wound healing therapies must be developed provide the cure or substantially boost other healing inter- and evidence-based practices established. New physi- ventions. Under the direction of Dr. Stephen Cummings, cians and support staff must be trained. Only through a Kent Hospital acquired three hyperbaric chambers in March blending of high quality clinical care with research and 2002, prompting a name change to the Kent Wound Recov- education will these objectives be achieved and future ery and Hyperbaric Medicine Center (KWRHMC) (Figure 1).