SARS-Cov-2, COVID-19 & Mountain Sports
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Accidentology of Mountain Sports Situation Review & Diagnosis
Accidentology of mountain sports Situation review & diagnosis Bastien Soulé Brice Lefèvre Eric Boutroy Véronique Reynier Frédérique Roux Jean Corneloup December 2014 A study produced by a research group Scientific supervisor: Bastien Soulé, sociologist Université Lyon 1, Sporting research and innovation centre Brice Lefèvre, sociologist Université Lyon 1, Sporting research and innovation centre Eric Boutroy, anthropologist Université Lyon 1, Sporting research and innovation centre Véronique Reynier, psychologist Université Grenoble Alpes, Sport & social environment laboratory Frédérique Roux, jurist Université Lyon 1, Sporting research and innovation centre Jean Corneloup, sociologist Université de Clermont-Ferrand, UMR PACTE CNRS With scientific support from PARN, Alpine centre for study and research in the field of natural risk prevention Acknowledgements We would like to thank all those contacted for interviews (sometimes several times) for their kind collaboration. We were authorised by most of the parties involved to access their accident/rescue intervention data. Being conscious of the sensitive nature of such information, and the large number of requests to access it, we hereby express our deepest gratitude. We would also like to thank the Petzl Foundation for having initiated and supported this project, and particularly Philippe Descamps for his openness and patience, Olivier Moret and Stéphane Lozac’hmeur for their assistance with this project. Cover photo: © O. Moret Back cover: © O. Moret Layout: Blandine Reynard Translation: -

What the New NPS Wilderness Climbing Policy Means for Climbers and Bolting Page 8
VERTICAL TIMES The National Publication of the Access Fund Summer 13/Volume 97 www.accessfund.org What the New NPS Wilderness Climbing Policy Means for Climbers and Bolting page 8 HOW TO PARK LIKE A CHAMP AND PRESERVE ACCESS 6 A NEW GEM IN THE RED 11 WISH FOR CLIMBING ACCESS THIS YEAR 13 AF Perspective “ The NPS recognizes that climbing is a legitimate and appropriate use of Wilderness.” — National Park Service Director Jonathan Jarvis his past May, National Park Service (NPS) Director Jonathan Jarvis issued an order explicitly stating that occasional fixed anchor use is T compatible with federally managed Wilderness. The order (Director’s Order #41) ensures that climbers will not face a nationwide ban on fixed anchors in NPS managed Wilderness, though such anchors should be rare and may require local authorization for placement or replacement. This is great news for anyone who climbs in Yosemite, Zion, Joshua Tree, Canyonlands, or Old Rag in the Shenandoah, to name a few. We have always said that without some provision for At the time, it seemed that fixed anchors, technical roped climbing can’t occur — and the NPS agrees. the tides were against us, The Access Fund has been working on this issue for decades, since even before we officially incorporated in 1991. In 1998, the U.S. Forest Service (USFS) that a complete ban on fixed issued a ban on fixed anchors in Wilderness (see photo inset) — at the time, it anchors in all Wilderness seemed that the tides were against us, that a complete ban on fixed anchors in all Wilderness areas was imminent. -

SKI TOURING in NORWAY Ski Touring in USA, France, Spain, Germany, Austria, Switzerland and Sweden and Their Perceptions of Norway As a Ski Touring Destination
Knowledge transfer project: SKI TOURING IN NORWAY Ski touring in USA, France, Spain, Germany, Austria, Switzerland and Sweden and their perceptions of Norway as a ski touring destination 2017‐2018 Contents Summary and key findings Ski touring France pages 1 – 30 Ski touring Germany, Austria, Switzerland pages 31 – 62 Ski touring Spain pages 63 – 76 Ski touring US pages 77 – 92 Ski touring Sweden pages 93 – 114 Photo: Håvard Myklebust – visitnorway.com Summary and key findings This project is a cooperation between Innovation Norway and NCE Tourism Fjord Norway. The project was conducted by Innovation Norway’s offices in France, Germany, USA, Spain and Sweden in 2017‐18. The project has been done in two phases. First we did a desktop survey scanning the markets’ ski touring tour operators, web sites, organizations, magazines and festivals. Secondly we conducted interviews with the most relevant tour operators in each market. The results are shown in this report. We hope that this report can contribute in the production of high quality ski touring adventures in Norway. Key results and take‐home messages are mentioned in this summary, but we recommend you to read the whole report. Opportunities ‐ There is an increased interest for ski touring in France, Germany, Spain and Sweden. In USA, the demand seems to remain stable. ‐ Sales of ski touring equipment has increased largely in France, ‐ Ski touring will most likely not become a volume activity, due to high demand of physical abilities, good mountain and snow knowledge and a certain income (France) ‐ In USA, Norway enjoys a strong association with skiing. -
CLARUS CORPORATION (Exact Name of Registrant As Specified in Its Charter)
UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 FORM 10-Q x Quarterly Report Pursuant to Section 13 or 15(d) of the Securities Exchange Act of 1934 For the quarterly period ended: June 30, 2019 or ¨ Transition Report Pursuant to Section 13 or 15(d) of the Securities Exchange Act of 1934 For the transition period from _________ to _________ Commission File Number: 001-34767 CLARUS CORPORATION (Exact name of registrant as specified in its charter) Delaware 58-1972600 (State or other jurisdiction of (I.R.S. Employer incorporation or organization) Identification Number) 2084 East 3900 South Salt Lake City, Utah 84124 (Address of principal executive offices) (Zip code) (801) 278-5552 (Registrant’s telephone number, including area code) Indicate by check mark whether the registrant: (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes x No ¨ Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes x No ¨ Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company, or an emerging growth company. -

Outdoor Recreation Activities in Nature Protection Areas – Situation in Germany
Working Papers of the Finnish Forest Research Institute 2 http://www.metla.fi/julkaisut/workingpapers/2004/mwp002.htm Outdoor recreation activities in nature protection areas – situation in Germany Stefan Türk, Edwin Jakob, Alexander Krämer & Ralf Roth Institut für Natursport und Ökologie, Deutsche Sporthochschule Köln, Germany [email protected] [email protected] [email protected] [email protected] Abstract: Within a research project of the Federal Nature Conservation Agency, the Institute of Outdoor Sports and Environment points out new developments in outdoor activities in several German landscapes significantly used for sports activities. Therefore two different types of landscape analysis were chosen: First the monitoring of selected sports activities in landscapes with special equipment respectively high frequented by sportsmen (top-spot method) and second the recording of the real utilisation of near-natural landscapes (area method). The results of the scientific analytics were combined with sociological knowl- edge to describe the development of outdoor recreation in different sport activities (e.g.: canoeing, climbing, paragliding or canyoning). Considering these results the possibilities and the limits of modern concepts of guidance are discussed. Convenience offers, the use of police law or the establishment of a new outdoor culture (depending on Scandinavian standards) will attach great importance to minimize stress and interference in natural landscapes. It is shown that the changes in outdoor activities offer the possibility for a sustainable use of the German countryside for recreation as well as for environment. The Significance of Outdoor Sporting even booming. Other sports, like skiing for example, Activities continue to be popular. Apart from the sportsmen and women, who are traditionally organised in clubs, Fun, self-realisation, independence, spontaneity, and there is a significant number of people who pursue individuality combined with nature experience are the new outdoor trend sports. -

SNOW SHOW 2019 STORE LIST January 30-February 1, 2019 | Colorado Convention Center | Denver, CO
SNOW SHOW 2019 STORE LIST January 30-February 1, 2019 | Colorado Convention Center | Denver, CO This retail store location list details only one unique storefront per city/state and/or city/country that attended Outdoor Retailer Snow Show 2019. ALABAMA THE WOODSMAN CO ......................................................FORT SMITH EV RIDEABLES ..................................................HUNTINGTON BEACH WERNERS TRADING CO ..................................................... CULLMAN WAL-MART .................................................................... BENTONVILLE FABFITFUN ................................................................... LOS ANGELES FAMBRANDS LLC........................................................................ BELL ALASKA CALIFORNIA FAST SKI SPORTS .................................................MAMMOTH LAKES 212TH RESCUE SQUADRON ...................................................... JBER 707 STREET ................................................................. LOS ANGELES FIGS .............................................................................. LOS ANGELES 6TH AVENUE OUTFITTERS ............................................ ANCHORAGE ABRAXAS ...............................................................................EUREKA FIRST CLOTHING ......................................................SAN FRANCISCO ALASKA HELISKIING ..............................................................HAINES ACTION SPORTS ..........................................................BAKERSFIELD FLIP -

Corporate Responsibility in the Outdoor
UNIVERSIDADE DE LISBOA FACULDADE DE MOTRICIDADE HUMANA Communication of corporate social responsibility: An analysis of different brands in the outdoor industry Dissertação elaborada com vista à obtenção do Grau de Mestre em Gestão do Desporto Orientador: Professor Doutor Abel Hermínio Lourenço Correia Júri: Presidente Professor Doutor Carlos Jorge Pinheiro Colaço, professor associado com agregação da Faculdade de Motricidade Humana da Universidade de Lisboa. Vogais Professor Doutor Abel Hermínio Lourenço Correia, professor associado com agregação da Faculdade de Motricidade Humana da Universidade de Lisboa; Professora Doutora Ana Maria Peixoto Naia, professora auxiliar da Faculdade de Motricidade Humana da Universidade de Lisboa. Isabella Maria Limmer 2017 Acknowledgment First of all I want to thank my supervisors Professor Doutor Abel Hermínio Lourenço Correia and Professor Doutor Rui Daniel Gaspar Neto Biscaia for their constant support and providing of professional knowledge. Furthermore I would like to express my gratitude to all participated outdoor brands for providing the relevant information for this thesis. Another thank you goes to my family. Especially to my parents, Edith and Ludwig, who made it possible for me, being the person who I am and always supporting me, and to my brother, Matthias, for his constant help and advices. I also want to give thanks to my closest friends and my boyfriend, Pierre, who were next to me and supported me through the entire writing process. I Resumo O estudo teve como objetivo analisar o papel da responsabilidade social empresarial (RSE) na indústria de atividades ao ar livre e verificar a implementação da comunicação da RSE nos sites das marcas deste sector. -

Mountain Bikers' Attitudes Towards Mountain Biking Tourism Destinations
MOUNTAIN BIKERS’ ATTITUDES TOWARDS MOUNTAIN BIKING TOURISM DESTINATIONS BY JULIE MOULARDE A thesis submitted to the Victoria University of Wellington as partial fulfilment of the requirements for the degree of Master of Tourism Management Victoria University of Wellington 2015 Abstract This thesis, grounded in consumer culture theory, delves into the sociocultural dynamics involved in tourist attitude content and formation. It addresses gaps in special interest tourism, sports tourism and tourist attitudes towards destinations literatures and further knowledge of mountain biking tourism, a niche, but growing, market. Qualitative methods grounded in interpretivism were used to understand how mountain bikers purposefully traveling to mountain bike tourism destinations form attitudes towards these destinations. Twenty-five mountain bikers from Wellington who qualified as serious leisure participants and had previously travelled for the primary purpose of mountain biking were interviewed. Social influence – through social ties, interactions and subcultural involvement – plays a central role in the respondents’ travel motivations and information search process, and thus influences attitude formation, strength and content. Therefore, the respondents are grouped based on centrality of mountain biking identity and subsequent desire to align with the subculture, and differences in attitude formation processes are highlighted. The respondents hold positive attitudes towards most destinations, emphasizing the need to investigate attitude strength and degree of positivity. Four main evaluative dimensions of attitudes are detailed (adventurous, natural, social and utilitarian). It is established that attitudes towards tourism destinations are (1) a qualitative evaluation of the experience anticipated or enabled rather that a quantitative appraisal of attributes, (2) continuously adjusted from the point of naïve awareness onwards, and (3) most relevant and revealing when operationalised as holistic summary evaluations rather than interrelated components. -

Managing Uncertainty Cover Art by Jim Harris
® 6"1 ÊΣ]Ê "°Ê{ÊUÊ*,Ê2013 Managing Uncertainty Cover art by Jim Harris In This Issue From the President...............................................................2 From the Editor ........................................................................2 AAA News......................................................................................3 What’s New . 4 Snow Science Time for a New Friction Term ...............................................8 Story by Doug Krause Beacon Interference Issues ..................................................10 Stream Flow & Wet Avalanche Cycles ..........................11 Trigger Locations in Complex Terrain............................26 Near twelve thousand feet in Silverton, there is a ridge that defines the southern boundary of Prospect Gulch. From this ridge, numerous north-facing avalanche paths descend through the sub-alpine forest. Just above treeline there is Managing Uncertainty a lightly wooded rib that separates a path’s shady side from the sunny side. We agreed that the light on the sunny side Improving Decision-Making Speak Your Mind .................................................cover, 14 made it a little more appealing. Steve dropped in and encountered semi-supportive temperature crust and invisible Group Communication in the Backcountry ...........15 wind funk. I changed my mind regarding the importance of pretty light and cautiously skied fall line to the top of the rib Radio Protocols.......................................................................17 between the adjacent start zones. A few scrubby trees provided a nice vantage from which to inspect the area. On either The Wisdom of Crowds .....................................................17 side of me the slopes steepened and fell to the valley floor about 1400' below. I hollered “I’m gonna check this side.” Continuing Pro Development: CAA Level 2 ..........18 I decided to throw a cut on the start zone before committing to the fall line, sussed my move and slowly approached Perspectives on Risk Risk: Focusing on the Wrong Action . -

Ski Meister Summer 2020
Alf Engen Ski Museum Foundation Ski MEISTER Utah Olympic Park, Park City, Utah PAGE 3 PAGE New Wasatch Mountain Exhibit! PAGE 4 PAGE Memories of Bear Hollow PAGE 7 PAGE Hall of Fame Oddity PAGE 10 PAGE A Museum Success Story SUMMER 2020 Preserving the rich history of snow sports in the Intermountain West engenmuseum.org CHAIRMAN’S LETTER Recently, I joined Alf Engen Ski Museum Executive Director Connie Nelson to welcome guests back to our museum for the first time since March 14. As I walked around the museum, I felt very comfortable and safe. I was also re- energized by our exhibits and the chance I had to engage again with the history I love. Board of Trustees We all learned many things from our quarantine this spring. One of those Tom Kelly personal revelations was how important culture and the arts are in my life, and Chairman the lives of our community. For 72 days this spring, our museum held only mem- David L. Vandehei ories. Now visitors are once again absorbing the remarkable history and stories inside the museum’s walls. Chairman Emeritus When the shutdown was implemented in mid-March, our board and staff acted quickly to handle the Alan K. Engen unprecedented circumstances. First and foremost, we assured our employees they would have a paycheck. Chairman Emeritus Then we turned our focus to support programs and dove into budgets. We plotted a course to protect our historical assets to ensure that when the time came, we could open our doors once again. Scott C. -

Banff Mountain Film Festival World Tour Film Menu
Banff Mountain Film Festival World Tour Films 2007/2008 20 Seconds of Joy Best Film on Mountain Sport and People’s Choice Award Germany, 2007, 60 minutes Directed by Jens Hoffman Produced by Cleonice Comino Website: www.f24film.com "I don't want to die, I want to live. I'm pretty good at running away, and this is my escape." This is how Karina Hollekim describes her dedication to BASE jumping. Documentary filmmaker Jens Hoffman first met the now 30-year-old Norwegian in 2002. He immediately started to film, planning to follow Karina over a long period, trying to understand why a young woman would challenge herself mentally and physically in such an extreme sport. Jens accompanies her through many stages of her BASE-jumping career, until it comes to a sudden stop and changes all aspects of her life. 24 Solo USA, 2007, 55 minutes Directed by Jason Berry Produced by Ken Bell Website: www.grippedfilms.com "24 Solo" follows the gut-wrenching story of Chris Eatough on his quest for a seventh world title in the unforgiving discipline of 24-hour solo mountain-bike racing. In the face of increased pressure from sponsors, new competitors to the sport, and a pregnant wife, Chris focuses his entire season on one race. Dark horse Craig Gordon, who is the Australian national champion, challenges Chris to a level of intensity and exhaustion which leaves one rider with severe blood poisoning. Aerialist USA, 2007, 27 minutes Directed by Brad Lynch, Jim Hurst Produced By Brad Lynch Website: www.aerialistmovie.com Dean Potter is obsessed with being attached to the world by as little as possible. -
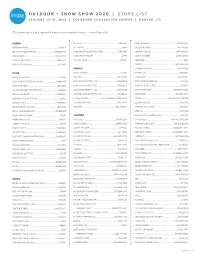
Snow Show 2020 Store List
OUTDOOR + SNOW SHOW 2020 | STORE LIST JANUARY 29-31, 2020 | COLORADO CONVENTION CENTER | DENVER, CO The below list includes registered buyers that attended Outdoor + Snow Show 2020. ALABAMA SKI HAUS ..........................................................................FLAGSTAFF CLEAN AESTHETIC .....................................................PLAYA DEL REY MOBTOWN MERCH................................................................ MOBILE SKI PRO INC ...............................................................................MESA COLLEGE OUTSIDE ....................................................... CARPINTERIA MOUNTAIN HIGH OUTFITTERS .....................................BIRMINGHAM SNOW MOUNTAIN RIVER INC (SMR) ...............................FLAGSTAFF COMFORT KICKS LA ..................................................SANTA MONICA PANTS STORE ............................................................... LEEDSLEEDS SUNRISE PARK RESORT .........................................................GREER COOZIE OUTDOORS ...................................................SANTA MONICA TRUCK GEAR BY LINE-X .................................................HUNTSVILLE THE HIKE HOUSE .................................................................. SEDONA COSMOTOG .................................................................................BREA WERNERS TRADING CO ..................................................... CULLMAN CURATED ..................................................................SAN FRANCISCO ARKANSAS CUSTOM SKI ESCAPE