Pdf&Tabid=77&Mid=860&Language=En-US for Supporting This Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Provincial Business Environment Scorecard in Cambodia
The Provincial Business Environment Scorecard in Cambodia A Measure of Economic Governance and Regulatory Policy November 2009 PBES 2009 | 1 The Provincial Business Environment Scorecard1 in Cambodia A Measure of Economic Governance and Regulatory Policy November 2009 1 The Provincial Business Environment Scorecard (PBES) is a partnership between the International Finance Corporation and the donors of the MPDF Trust Fund (the European Union, Finland, Ireland, the Netherlands, New Zealand, and Switzerland), and The Asia Foundation, with funding support from Danida, DFID and NZAID, the Multi-Donor Livelihoods Facility. PBES 2009 | 3 PBES 2009 | 4 Table of Contents List of Tables ..........................................................................................................................................................iii List of Figures .........................................................................................................................................................iv Abbreviations ............................................................................................................................................................v Acknowledgments .....................................................................................................................................................vi 1. Introduction ............................................................................................................................ 1 1. PBES Scorecard and Sub-indices .......................................................................................... -

Cambodia Msme 2/Bee Project Quarterly Report No. 15 (April 1 – June 30, 2012)
s page left intentionally blank for double-sided printing. CAMBODIA MSME 2/BEE PROJECT QUARTERLY REPORT NO. 15 (APRIL 1 – JUNE 30, 2012) TASK ORDER NO. 04 JULY 31, 2012 JANUARY 31, 2011 This publication was produced for review by the United States Agency for International ThisDevelopment. publication It was was produced prepared for by reviewDAI. by the United States Agency for International Development. It was prepared by DAI. This page left intentionally blank for double-sided printing. USAID Cambodia MSME2/BEE Project Quarterly Report No. 15 Task Order No. 4 Program Title: Strengthening Micro, Small and Medium Enterprises in Cambodia Sponsoring USAID Office: USAID/Cambodia Contract Number: EEM-I-00-07-00009-00/04 Contractor: DAI Date of Publication: July 31, 2012 Author: Cambodia MSME 2/BEE Project The authors’ views expressed in this publication do not necessarily reflect the views of the United States Agency for International Development or the United States Government. Contents Introduction ..................................................................................................................... 8 Background ..................................................................................................................... 8 Project Objectives and Approach .................................................................................... 9 Summary of Project Highlights This Quarter ................................................................. 10 Component 1 - Strengthening Value Chains ........................................ -
Information to Users
INFORMATION TO USERS The most advanced technology has been used to photograph and reproduce this manuscript from the microfilm master. UMI films the text directly from the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter face, while others may be from any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleedthrough, substandard margins, and improper alignment can adversely affect reproduction. In the unlikely event that the author did not send UMI a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. Oversize materials (e.g., maps, drawings, charts) are reproduced by sectioning the original, beginning at the upper left-hand corner and continuing from left to right in equal sections with small overlaps. Each original is also photographed in one exposure and is included in reduced form at the back of the book. Photographs included in the original manuscript have been reproduced xerographically in this copy. Higher quality 6" x 9" black and white photographic prints are available for any photographs or illustrations appearing in this copy for an additional charge. Contact UMI directly to order. University Microfilms International A Bell & Howell Information Company 300 North Zeeb Road. Ann Arbor, Ml 48106-1346 USA 313/761-4700 800/521-0600 Order Number 9111799 Evolutionary morphology of the locomotor apparatus in Arachnida Shultz, Jeffrey Walden, Ph.D. -
Inclusive and Sustainable Value Chains and Food Fortification
Credit: DCA\LWD Rapid Assessment Report May 2016. Photo from Prey Veng village, Prambei Mom commune, Thpong district, Kampong Speu Synthesis Report of NGO Drought Assessments in Cambodia: by Participant Organisations of the Humanitarian Response Forum (HRF) May 2016 Table of Contents Table of Contents 2 Acronyms 3 1. Executive Summary 4 2. Objective of the Report 6 3. Methodology and Report Limitations 6 4. Situation Overview 8 5. Findings and Observations 10 5.1 Affected areas and Priority Needs 10 5.2 Snapshot of Sectoral Findings 12 5.3 Coping Strategies 19 6. Response to Date 20 6.1 Government Response 20 6.2 HRF Participant Organisations’ Response 21 7. Conclusion and Recommendations 24 8. Annexes 26 Report compiled by Sharon Moynihan Hill ([email protected]) 2 Acronyms CARE CARE International in Cambodia CHF Cambodia Humanitarian Forum CWS Church World Service DCA Danish Church Aid DCDM District Committee for Disaster Management FGM Focused Group Discussions HEKS Hilfswerk der Evangelischenkirchen HRF Humanitarian Response Forum KII Key Informant Interviews LWD Life with Dignity MoEYS Ministry of Education Youth and Sport MRD Ministry of Rural Development NCDM National Committee for Disaster Management PCDM Provincial Committee for Disaster Management PDoA Provincial Department of Agriculture PDoWRAM Provincial Department of Water Resources and Meteorology PIN People in Need PoE Provincial Department of Education PWD People with Disabilities RGA Rapid Gender Assessment WFP World Food Programme WWH Welthungerhilfe 3 1. Executive Summary The 2015-16 El Niño weather phenomenon has resulted in significantly less rainfall patterns, warmer weather and delayed or shorter monsoon rains in Cambodia. -

How Do Rural Communities Sustain Sanitation Gains? Qualitative Comparative Analyses of Community-Led Approaches in Cambodia and Ghana
sustainability Article How Do Rural Communities Sustain Sanitation Gains? Qualitative Comparative Analyses of Community-Led Approaches in Cambodia and Ghana Jessica Tribbe 1,* , Valentina Zuin 2, Caroline Delaire 1, Ranjiv Khush 1 and Rachel Peletz 1 1 The Aquaya Institute, San Anselmo, CA 94960, USA; [email protected] (C.D.); [email protected] (R.K.); [email protected] (R.P.) 2 Division of Social Science, Yale-NUS College, Singapore 138527, Singapore; [email protected] * Correspondence: [email protected]; Tel.: +1-(513)314-9254 Abstract: Community-led Total Sanitation (CLTS) is a popular intervention for eliminating open defecation in rural communities. Previous research has explored the contextual and programmatic factors that influence CLTS performance. Less is known about the community-level conditions that sustain latrine coverage and use. We hypothesized three categories of community conditions underlying CLTS sustainability: (i) engagement of community leaders, (ii) follow-up intensity, and (iii) support to poor households. We evaluated these among communities in Cambodia and Ghana, and applied fuzzy-set Qualitative Comparative Analysis (fsQCA) to identify combinations of conditions that influenced current latrine coverage and consistent latrine use. In Cambodia, latrine coverage was highest in communities with active commune-level leaders rather than traditional Citation: Tribbe, J.; Zuin, V.; Delaire, leaders, and with leaders who used casual approaches for promoting latrine construction. Latrine C.; Khush, R.; Peletz, R. How Do use in Cambodia was less consistent among communities with intense commune engagement, higher Rural Communities Sustain pressure from traditional leaders, high follow-up and high financial support. In Ghana, by contrast, Sanitation Gains? Qualitative active leaders, high follow-up, high pro-poor support, and continued activities post-implementation Comparative Analyses of Community-Led Approaches in promoted latrine coverage and consistent use. -

KHM 0801 Cbdrrgoodpractic
Building Disaster Resilient Communities – DipECHO Consortium (Dan Church Aid/ActionAid/People in Need) Documentation of CBDRR Models for the DipECHO VIII Action in Cambodia PCDM provincial trainers conducting training on DRR for CSOs in Kompong Channang October 2013 Mrs. Bernie O‟Neill Abbreviations Used AAC Action Aid Cambodia ADIFE Association for the increase in Development of Family Economy (local partner of AAC) BBC British Broadcasting Corporation BDRC Building Disaster Resilient Communities (title of consortium proposal to DipECHO) BMC Banteay Meanchey (province) BTB Battambang (province) CBDRR Community Based Disaster Risk Reduction CCDM Commune Committee for Disaster Management CEDAC Centre d‟Etude et de Development Agricole Cambodgien CHRD Cambodian Human Resource Development (local partner of AAC) CIP Commune Investment Plan CRC Cambodian Red Cross CSO Civil Society Organization DCA Dan Church Aid DCDM District Committee for Disaster Management DM Disaster Management DRAT Drought Resistant Agriculture Technology DRM Disaster Risk Management DRR Disaster Risk Reduction ECHO European Commission Humanitarian (office) Aid EWS Early Warning System GPG Good Practice Guide HVCA Hazard, Vulnerability, Capacity Assessment IEC Information, Education & Communication (materials) KAFDOC Khmer Association for the Development of the Countryside LWD Life With Dignity (implementing partner of DCA) MOEYS Ministry of Education, Youth & Sport MoI Ministry of Information NCDM National Committee for Disaster Management NDEWS Natural Disaster Early -

Detection of Influenza a Viruses from Environmental Lake and Pond Ice
TITLE “DETECTION OF INFLUENZA A VIRUSES FROM ENVIRONMENTAL LAKE AND POND ICE” Zeynep A. Koçer A Dissertation Submitted to the Graduate College of Bowling Green State University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY August 2010 Committee: Scott O. Rogers, Advisor W. Robert Midden Graduate Faculty Representative John Castello George Bullerjahn Paul Morris ii ABSTRACT Scott O. Rogers, Advisor Environmental ice is an ideal matrix for the long-term protection of organisms due to the limitation of degradative processes. As a result of global climate change, some glaciers and polar ice fields are melting at rapid rates. This process releases viable microorganisms that have been embedded in the ice, sometimes for millions of years. We propose that viral pathogens have adapted to being entrapped in ice, such that they are capable of infecting naïve hosts after melting from the ice. Temporal gene flow, which has been termed genome recycling (Rogers et al., 2004), may allow pathogens to infect large host populations rapidly. Accordingly, we hypothesize that viable influenza A virions are preserved in lake and pond ice. Our main objective was to identify influenza A (H1-H16) from the ice of a few lakes and ponds in Ohio that have high numbers of migratory and local waterfowl visiting the sites. We developed a set of hemagglutinin subtype-specific primers for use in four multiplex RT-PCR reactions. Model studies were developed by seeding environmental lake water samples in vitro with influenza A viruses and subjecting the seeded water to five freeze-thaw cycles at -20oC and -80oC. -
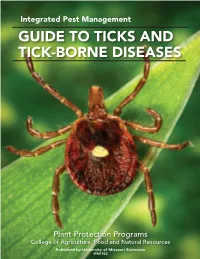
Guide to Ticks and Tick-Borne Diseases
Integrated Pest Management GUIDE TO TICKS AND TICK-BORNE DISEASES Plant Protection Programs College of Agriculture, Food and Natural Resources Published by University of Missouri Extension IPM1032 This publication is part of a series of integrated pest CONTENTS management (IPM) manuals prepared by the Plant Protection Programs of the University of Missouri. Topics INTRODUCTION TO TICKS . 3 covered in the series include an introduction to scouting, Morphology . 4 weed identification and management, plant diseases, and Identification . .6 insects of field and horticultural crops. These IPM manuals Life cycle . .7 are available from MU Extension at the following address: Behavior . 8 Distribution and ecology . 10 Extension Publications MEDICALLY IMPORTANT TICKS . .12 2800 Maguire Blvd. Lone star tick (Amblyomma americanum) . 12 Columbia, MO 65211 American dog tick (Dermacentor variabilis) .13 800-292-0969 Blacklegged tick (Ixodes scapularis) . 13 Brown dog tick (Rhipicephalus sanguineus) . 14 Relapsing fever tick (Ornithodoros turicata) 14 Bat tick (Ornithodoros kelleyi) . .15 Author Richard M. Houseman TICK-BORNE DISEASES . .16 Associate Professor of Entomology Human ehrlichiosis . 16 University of Missouri Extension Rocky Mountain spotted fever . 17 Southern tick-associated rash illness . .17 Lyme disease . 18. On the cover Anaplasmosis . 18 Dorsal view of a female lone star tick, Tick-borne relapsing fever . 19 Amblyomma americanum. Photo credit: James Tularemia . 19. Gathany, CDC INDIVIDUAL PERSONAL PROTECTION . 20 Photo credits Tick bite prevention . .20 Tick checks . 22 All photos were provided by the author, unless Tick removal . 22 otherwise indicated. Self-monitoring and medical treatment . 23 Follow-up . 24 Credits Centers for Disease Control and Prevention INTEGRATED PEST MANAGEMENT (IPM) (CDC) OF TICK POPULATIONS . -

Research Article Isolation of a Reassortant H1N2 Swine Flu Strain of Type (Swine-Human-Avian) and Its Genetic Variability Analysis
Hindawi BioMed Research International Volume 2018, Article ID 1096079, 10 pages https://doi.org/10.1155/2018/1096079 Research Article Isolation of a Reassortant H1N2 Swine Flu Strain of Type (Swine-Human-Avian) and Its Genetic Variability Analysis Long-Bai Wang , Qiu-Yong Chen, Xue-Min Wu , Yong-Liang Che, Cheng-Yan Wang, Ru-Jing Chen, and Lun-Jiang Zhou Institute of Animal Husbandry and Veterinary Medicine, Fujian Academy of Agriculture Sciences, Fujian Animal Disease Control Technology Development Center, Fuzhou, Fujian 350013, China Correspondence should be addressed to Lun-Jiang Zhou; [email protected] Received 3 January 2018; Accepted 26 February 2018; Published 29 May 2018 Academic Editor: Jialiang Yang Copyright © 2018 Long-Bai Wang et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Weisolated an infuenza strain named A/Swine/Fujian/F1/2010 (H1N2) from a pig suspected to be infected with swine fu. Te results of electron microscopy, hemagglutination (HA) assay, hemagglutination inhibition (HI) assay, and whole genome sequencing analysis suggest that it was a reassortant virus of swine (H1N1 subtype), human (H3N2 subtype), and avian infuenza viruses. To further study the genetic evolution of A/Swine/Fujian/F1/2010 (H1N2), we cloned its whole genome fragments using RT-PCR and performed phylogenetic analysis on the eight genes. As a result, the nucleotide sequences of HA, NA, PB1, PA, PB2, NP, M, and NS gene are similar to those of A/Swine/Shanghai/1/2007(H1N2) with identity of 98.9%, 98.9%, 99.0%, 98.6%, 99.0%, 98.9%, 99.3%, and 99.3%, respectively. -

Land Transactions in Rural Cambodia a Synthesis of Findings from Research on Appropriation and Derived Rights to Land
Études et Travaux en ligne no 18 Pel Sokha, Pierre-Yves Le Meur, Sam Vitou, Laing Lan, Pel Setha, Hay Leakhena & Im Sothy Land Transactions in Rural Cambodia A Synthesis of Findings from Research on Appropriation and Derived Rights to Land LES ÉDITIONS DU GRET Land Transactions in Rural Cambodia Document Reference Pel Sokha, Pierre-Yves Le Meur, Sam Vitou, Laing Lan, Pel Setha, Hay Leakhen & Im Sothy, 2008, Land Transactions in Rural Cambodia : A synthesis of Findings from Research on Appropriation and Derived Rights to Land, Coll. Études et Travaux, série en ligne n°18, Éditions du Gret, www.gret.org, May 2008, 249 p. Authors: Pel Sokha, Pierre-Yves Le Meur, Sam Vitou, Laing Lan, Pel Setha, Hay Leakhen & Im Sothy Subject Area(s): Land Transactions Geographic Zone(s): Cambodia Keywords: Rights to Land, Rural Development, Land Transaction, Land Policy Online Publication: May 2008 Cover Layout: Hélène Gay Études et Travaux Online collection This collection brings together papers that present the work of GRET staff (research programme results, project analysis documents, thematic studies, discussion papers, etc.). These documents are placed online and can be downloaded for free from GRET’s website (“online resources” section): www.gret.org They are also sold in printed format by GRET’s bookstore (“publications” section). Contact: Éditions du Gret, [email protected] Gret - Collection Études et Travaux - Série en ligne n° 18 1 Land Transactions in Rural Cambodia Contents Acknowledgements.................................................................................................................................. -
Serological Methods in the Identification and Characterization of Viruses
CHAPTER 4 Serological Methods in the Identification and Characterization of Viruses M. H. V. Van Regenmortel Laboratoire de Virologie Institut de Biologie Mo!eculaire et Cellulaire 67000 Strasbourg, France 1. INTRODUCTION The purpose of this chapter is to present an integrated view of the various serological techniques that have been used in virology. The accent will be placed on the principles that govern each type of test and on the general applicability of the different serological techniques in all fields of virus research. In recent years, advances in serological tech niques have sometimes been applied in only one area of virology, although they could have been equally useful to workers studying other groups of viruses. No doubt this stems from the host-oriented approach that has guided the compartmentation of virology into separate fields of specialization. When it comes to serological properties, however, the similarities between animal, insect, bacterial, and plant viruses are paramount. The same immunochemical principles govern the in vitro serological reactions of all viral antigens, and much of general interest can be learned from the findings obtained with each particular group of viruses. An attempt will be made here to emphasize the general validity of specific experimental procedures. A number of recent reviews restricted to the serology of particular groups of viruses are available 183 H. Fraenkel-Conrat et al. (eds.), Comprehensive Virology © Plenum Press, New York 1981 184 Chapter 4 (Cowan, 1973; Schmidt and Lennette, 1973; Ball, 1974; Kurstak and Morisset, 1974; Burns and Allison, 1975; Mazzone and Tignor, 1976; Mayr et al., 1977; Tyrrell, 1978; Van Regenmortel, 1978; Cooper, 1979). -

MORFOLOGIA E DESENVOLVIMENTO DO SISTEMA REPRODUTOR MASCULINO DE CARRAPATOS DO GÊNERO Amblyomma (ACARI, IXODIDAE): UMA ANÁLISE COMPARATIVA
UNIVERSIDADE ESTADUAL PAULISTA “JÚLIO DE MESQUITA FILHO” INSTITUTO DE BIOCIÊNCIAS – RIO unesp CLARO PROGRAMA DE PÓS-GRADUAÇÃO EM CIÊNCIAS BIOLÓGICAS (BIOLOGIA CELULAR E MOLECULAR) MORFOLOGIA E DESENVOLVIMENTO DO SISTEMA REPRODUTOR MASCULINO DE CARRAPATOS DO GÊNERO Amblyomma (ACARI, IXODIDAE): UMA ANÁLISE COMPARATIVA BRUNO RODRIGUES SAMPIERI Tese apresentada ao Instituto de Biociências do Campus de Rio Claro, Universidade Estadual Paulista, como parte dos requisitos para obtenção do título de Doutor em Ciências Biológicas (Biologia Celular e Molecular). Maio - 2016 UNIVERSIDADE ESTADUAL PAULISTA “JÚLIO DE MESQUITA FILHO” INSTITUTO DE BIOCIÊNCIAS – RIO unesp CLARO PROGRAMA DE PÓS-GRADUAÇÃO EM CIÊNCIAS BIOLÓGICAS (BIOLOGIA CELULAR E MOLECULAR) MORFOLOGIA E DESENVOLVIMENTO DO SISTEMA REPRODUTOR MASCULINO DE CARRAPATOS DO GÊNERO Amblyomma (ACARI, IXODIDAE): UMA ANÁLISE COMPARATIVA BRUNO RODRIGUES SAMPIERI ORIENTADORA: PROFA. DRA. MARIA IZABEL CAMARGO-MATHIAS CO-ORIENTADOR: PROF. DR. ODAIR CORREA BUENO Tese apresentada ao Instituto de Biociências do Campus de Rio Claro, Universidade Estadual Paulista, como parte dos requisitos para obtenção do título de Doutor em Ciências Biológicas (Biologia Celular e Molecular). Maio - 2016 591.4 Sampieri, Bruno Rodrigues S192m Morfologia e desenvolvimento do sistema reprodutor masculino de carrapatos do gênero Amblyomma (Acari, Ixodidae) : uma análise comparativa / Bruno Rodrigues Sampieri. - Rio Claro, 2016 113 f. : il., figs., tabs. Tese (doutorado) - Universidade Estadual Paulista, Instituto de Biociências de Rio Claro Orientadora: Maria Izabel Souza Camargo Coorientador: Odair Correa Bueno 1. Anatomia comparada. 2. Espermiotaxonomia. 3. Espermiocladística. 4. Filogenia. 5. Controle. I. Título. Ficha Catalográfica elaborada pela STATI - Biblioteca da UNESP Campus de Rio Claro/SP Dedicatória Dedico esta tese aos meus pais, à minha esposa, à minha filha e ao meu irmão, pelo apoio, companheirismo e paciência; por compartilharem comigo angústias e conquistas.