Procedures, Programs and Drugs You Must Precertify
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Spinraza™ (Nusinersen)
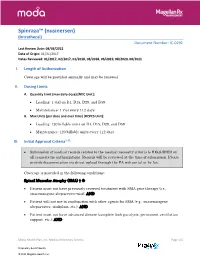
Spinraza™ (nusinersen) (Intrathecal) Document Number: IC-0291 Last Review Date: 08/03/2021 Date of Origin: 01/31/2017 Dates Reviewed: 01/2017, 02/2017, 01/2018, 08/2018, 06/2019, 08/2020, 08/2021 I. Length of Authorization Coverage will be provided annually and may be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: • Loading: 1 vial on D1, D15, D29, and D59 • Maintenance: 1 vial every 112 days B. Max Units (per dose and over time) [HCPCS Unit]: • Loading: 120 billable units on D1, D15, D29, and D59 • Maintenance: 120 billable units every 112 days III. Initial Approval Criteria1-12 • Submission of medical records related to the medical necessity criteria is REQUIRED on all requests for authorizations. Records will be reviewed at the time of submission. Please provide documentation via direct upload through the PA web portal or by fax. Coverage is provided in the following conditions: Spinal Muscular Atrophy (SMA) † Ф • Patient must not have previously received treatment with SMA gene therapy (i.e., onasemnogene abeparvovec-xioi); AND • Patient will not use in combination with other agents for SMA (e.g., onasemnogene abeparvovec, risdiplam, etc.); AND • Patient must not have advanced disease (complete limb paralysis, permanent ventilation support, etc.); AND Moda Health Plan, Inc. Medical Necessity Criteria Page 1/5 Proprietary & Confidential © 2021 Magellan Health, Inc. • Patient must have the following laboratory tests at baseline and prior to each administration*: platelet count, prothrombin time; activated -

2017 ANNUAL REPORT | Translating SCIENCE • Transforming LIVES OUR COMMITMENT Make Every Day Count at PTC, Patients Are at the Center of Everything We Do
20 YEARS OF COMMITMENT 2017 ANNUAL REPORT | Translating SCIENCE • Transforming LIVES OUR COMMITMENT Make every day count At PTC, patients are at the center of everything we do. We have the opportunity to support patients and families living with rare disorders through their journey. We know that every day matters and we are committed to making a difference. OUR SCIENCE Our scientists are finding new ways to regulate biology to control disease We have several scientific research platforms focused on modulating protein expression within the cell that we believe have the potential to address many rare genetic disorders. OUR PEOPLE Care for each other, our community, and for the needs of our patients At PTC, we are looking at drug discovery and development in a whole new light, bringing new technologies and approaches to developing medicines for patients living with rare disorders and cancer. We strive every day to be better than we were the day before. At PTC Therapeutics, it is our mission to provide access to best-in-class treatments for patients who have an unmet need. We are a science-led, global biopharmaceutical company focused on the discovery, development and commercialization of clinically-differentiated medicines that provide benefits to patients with rare disorders. Founded 20 years ago, PTC Therapeutics has successfully launched two rare disorder products and has a global commercial footprint. This success is the foundation that drives investment in a robust pipeline of transformative medicines and our mission to provide access to best-in-class treatments for patients who have an unmet medical need. As we celebrate our 20th year of bringing innovative therapies to patients affected by rare disorders, we reflect on our unwavering commitment to our patients, our science and our employees. -

Spinraza® (Nusinersen)
UnitedHealthcare® Commercial Medical Benefit Drug Policy Spinraza® (Nusinersen) Policy Number: 2021D0059I Effective Date: July 1, 2021 Instructions for Use Table of Contents Page Community Plan Policy Coverage Rationale ....................................................................... 1 • Spinraza® (Nusinersen) Documentation Requirements ...................................................... 3 Applicable Codes .......................................................................... 3 Background.................................................................................... 4 Benefit Considerations .................................................................. 5 Clinical Evidence ........................................................................... 5 U.S. Food and Drug Administration ............................................. 8 References ..................................................................................... 9 Policy History/Revision Information ........................................... 10 Instructions for Use ..................................................................... 11 Coverage Rationale See Benefit Considerations Spinraza® (nusinersen) is proven and medically necessary for the treatment of spinal muscular atrophy (SMA) in patients who meet all of the following criteria: 1-4,22,23 Initial Therapy Diagnosis of spinal muscular atrophy by, or in consultation with, a neurologist with expertise in the diagnosis of SMA; and Submission of medical records (e.g., chart notes, laboratory values) -

DRUGS REQUIRING PRIOR AUTHORIZATION in the MEDICAL BENEFIT Page 1
Effective Date: 08/01/2021 DRUGS REQUIRING PRIOR AUTHORIZATION IN THE MEDICAL BENEFIT Page 1 Therapeutic Category Drug Class Trade Name Generic Name HCPCS Procedure Code HCPCS Procedure Code Description Anti-infectives Antiretrovirals, HIV CABENUVA cabotegravir-rilpivirine C9077 Injection, cabotegravir and rilpivirine, 2mg/3mg Antithrombotic Agents von Willebrand Factor-Directed Antibody CABLIVI caplacizumab-yhdp C9047 Injection, caplacizumab-yhdp, 1 mg Cardiology Antilipemic EVKEEZA evinacumab-dgnb C9079 Injection, evinacumab-dgnb, 5 mg Cardiology Hemostatic Agent BERINERT c1 esterase J0597 Injection, C1 esterase inhibitor (human), Berinert, 10 units Cardiology Hemostatic Agent CINRYZE c1 esterase J0598 Injection, C1 esterase inhibitor (human), Cinryze, 10 units Cardiology Hemostatic Agent FIRAZYR icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent HAEGARDA c1 esterase J0599 Injection, C1 esterase inhibitor (human), (Haegarda), 10 units Cardiology Hemostatic Agent ICATIBANT (generic) icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent KALBITOR ecallantide J1290 Injection, ecallantide, 1 mg Cardiology Hemostatic Agent RUCONEST c1 esterase J0596 Injection, C1 esterase inhibitor (recombinant), Ruconest, 10 units Injection, lanadelumab-flyo, 1 mg (code may be used for Medicare when drug administered under Cardiology Hemostatic Agent TAKHZYRO lanadelumab-flyo J0593 direct supervision of a physician, not for use when drug is self-administered) Cardiology Pulmonary Arterial Hypertension EPOPROSTENOL (generic) -

New Brunswick Drug Plans Formulary
New Brunswick Drug Plans Formulary August 2019 Administered by Medavie Blue Cross on Behalf of the Government of New Brunswick TABLE OF CONTENTS Page Introduction.............................................................................................................................................I New Brunswick Drug Plans....................................................................................................................II Exclusions............................................................................................................................................IV Legend..................................................................................................................................................V Anatomical Therapeutic Chemical (ATC) Classification of Drugs A Alimentary Tract and Metabolism 1 B Blood and Blood Forming Organs 23 C Cardiovascular System 31 D Dermatologicals 81 G Genito Urinary System and Sex Hormones 89 H Systemic Hormonal Preparations excluding Sex Hormones 100 J Antiinfectives for Systemic Use 107 L Antineoplastic and Immunomodulating Agents 129 M Musculo-Skeletal System 147 N Nervous System 156 P Antiparasitic Products, Insecticides and Repellants 223 R Respiratory System 225 S Sensory Organs 234 V Various 240 Appendices I-A Abbreviations of Dosage forms.....................................................................A - 1 I-B Abbreviations of Routes................................................................................A - 4 I-C Abbreviations of Units...................................................................................A -

European Medicines Agency Accepts Marketing Authorization Application for Asfotase Alfa As a Treatment for Patients with Hypophosphatasia
July 24, 2014 European Medicines Agency Accepts Marketing Authorization Application for Asfotase Alfa as a Treatment for Patients with Hypophosphatasia -- Application designated for review under accelerated assessment process -- CHESHIRE, Conn.--(BUSINESS WIRE)-- Alexion Pharmaceuticals, Inc. (NASDAQ:ALXN) today announced that the Marketing Authorization Application (MAA) for asfotase alfa, an investigational, first-in-class targeted enzyme replacement therapy for the treatment of hypophosphatasia (HPP), has been validated and granted accelerated assessment by the European Medicines Agency (EMA). The acceptance of this MAA marks the beginning of the review process in the European Union (EU) for this potential new treatment. "HPP is a devastating disease for patients and their families due to progressive deterioration of bones and muscle weakness, which can result in impaired respiratory function, severe disability and death," said Leonard Bell, M.D., Chief Executive Officer of Alexion. "If approved, asfotase alfa would be the first therapy for patients with this life-threatening disorder." The EU filing includes positive data from 68 patients with pediatric-onset HPP (ranging from newborns to 66 years of age) enrolled in three pivotal prospective studies and their extensions, as well as a retrospective natural history study in infants. In April, Alexion initiated the rolling submission of a Biologics License Application (BLA) for asfotase alfa as a treatment for patients with HPP with the U.S. Food and Drug Administration (FDA). About -

Prescription Drugs Requiring Prior Authorization
PRESCRIPTION DRUGS REQUIRING PRIOR AUTHORIZATION Revised 10/16 As part of our drug utilization management program, members must request and receive prior authorization for certain prescription drugs in order to use their prescription drug benefits. Below is a list of drugs that currently require prior authorization. This list will be updated periodically as new drugs that require prior authorization are introduced. As benefits may vary by group and individual plans, the inclusion of a medication on this list does not imply prescription drug coverage. The Schedule of Benefits contains a list of drug categories that require prior authorization. Prior authorization requests are processed by our pharmacy benefit manager, Express Scripts, Inc. (ESI). Physicians must call ESI to obtain an authorization. (1-800-842-2015). Drug Name Generic Name Drug Classification Abstral fentanyl citrate oral tablet Controlled Dangerous Substance Accu-Chek Test Strips blood glucose test strips Blood Glucose Test Strips Actemra tocilizumab Monoclonal Antibody Acthar corticotropin Hormone Actimmune interferon gamma 1b Interferon Actiq fentanyl citrate OTFC Controlled Dangerous Substance Adcirca tadalafil Pulmonary Vasodilator Adempas riociguat Pulmonary Vasodilator Adlyxin lixisenatide Type 2 Diabetes Advocate Test Strips blood glucose test strips Blood Glucose Test Strips Aerospan** flunisolide Corticosteroids (Inhaled) Afrezza insulin Insulin (inhaled) Ampyra dalfampridine Multiple Sclerosis Agent Altoprev** lovastatin Cholesterol Alvesco** ciclesonide Corticosteroids -

Circulating Biomarkers in Neuromuscular Disorders: What Is Known, What Is New
biomolecules Review Circulating Biomarkers in Neuromuscular Disorders: What Is Known, What Is New Andrea Barp 1,* , Amanda Ferrero 1, Silvia Casagrande 1,2 , Roberta Morini 1 and Riccardo Zuccarino 1 1 NeuroMuscular Omnicentre (NeMO) Trento, Villa Rosa Hospital, Via Spolverine 84, 38057 Pergine Valsugana, Italy; [email protected] (A.F.); [email protected] (S.C.); [email protected] (R.M.); [email protected] (R.Z.) 2 Department of Neurosciences, Drug and Child Health, University of Florence, Largo Brambilla 3, 50134 Florence, Italy * Correspondence: [email protected] Abstract: The urgent need for new therapies for some devastating neuromuscular diseases (NMDs), such as Duchenne muscular dystrophy or amyotrophic lateral sclerosis, has led to an intense search for new potential biomarkers. Biomarkers can be classified based on their clinical value into different categories: diagnostic biomarkers confirm the presence of a specific disease, prognostic biomarkers provide information about disease course, and therapeutic biomarkers are designed to predict or measure treatment response. Circulating biomarkers, as opposed to instrumental/invasive ones (e.g., muscle MRI or nerve ultrasound, muscle or nerve biopsy), are generally easier to access and less “time-consuming”. In addition to well-known creatine kinase, other promising molecules seem to be candidate biomarkers to improve the diagnosis, prognosis and prediction of therapeutic response, such as antibodies, neurofilaments, and microRNAs. However, there are some criticalities that can complicate their application: variability during the day, stability, and reliable performance metrics Citation: Barp, A.; Ferrero, A.; (e.g., accuracy, precision and reproducibility) across laboratories. In the present review, we discuss Casagrande, S.; Morini, R.; Zuccarino, the application of biochemical biomarkers (both validated and emerging) in the most common NMDs R. -

The Use of Ataluren in the Effective Management of Duchenne Muscular Dystrophy
Review Neuromuscular Diseases Early Diagnosis and Treatment – The Use of Ataluren in the Effective Management of Duchenne Muscular Dystrophy Eugenio Mercuri,1 Ros Quinlivan2 and Sylvie Tuffery-Giraud3 1. Catholic University, Rome, Italy; 2. Great Ormond Street Hospital and National Hospital for Neurology and Neurosurgery, London, UK; 3. Laboratory of Genetics of Rare Diseases (LGMR), University of Montpellier, Montpellier, France DOI: https://doi.org/10.17925/ENR.2018.13.1.31 he understanding of the natural history of Duchenne muscular dystrophy (DMD) is increasing rapidly and new treatments are emerging that have the potential to substantially improve the prognosis for patients with this disabling and life-shortening disease. For many, Thowever, there is a long delay between the appearance of symptoms and DMD diagnosis, which reduces the possibility of successful treatment. DMD results from mutations in the large dystrophin gene of which one-third are de novo mutations and two-thirds are inherited from a female carrier. Roughly 75% of mutations are large rearrangements and 25% are point mutations. Certain deletions and nonsense mutations can be treated whereas many other mutations cannot currently be treated. This emphasises the need for early genetic testing to identify the mutation, guide treatment and inform genetic counselling. Treatments for DMD include corticosteroids and more recently, ataluren has been approved in Europe, the first disease-modifying therapy for treating DMD caused by nonsense mutations. The use of ataluren in DMD is supported by positive results from phase IIb and phase III studies in which the treatment produced marked improvements in the 6-minute walk test, timed function tests such as the 10 m walk/run test and the 4-stair ascent/descent test compared with placebo. -

Asfotase Alfa for Infants and Young Children with Hypophosphatasia: 7 Year Outcomes of a Single-Arm, Open-Label, Phase 2 Extension Trial
Articles Asfotase alfa for infants and young children with hypophosphatasia: 7 year outcomes of a single-arm, open-label, phase 2 extension trial Michael P Whyte, Jill H Simmons, Scott Moseley, Kenji P Fujita, Nicholas Bishop, Nada J Salman, John Taylor, Dawn Phillips, Mairead McGinn, William H McAlister Summary Background Our previous phase 2, open-label study of 11 infants and young children with life-threatening perinatal or Lancet Diabetes Endocrinol infantile hypophosphatasia showed 1 year safety and efficacy of asfotase alfa, an enzyme replacement therapy. We 2019; 7: 93–105 aimed to report the long-term outcomes over approximately 7 years of treatment. Published Online December 14, 2018 http://dx.doi.org/10.1016/ Methods We did a prespecified, end of study, 7 year follow-up of our single-arm, open-label, phase 2 trial in which S2213-8587(18)30307-3 children aged 3 years or younger with life-threatening perinatal or infantile hypophosphatasia were recruited from This online publication has been ten hospitals (six in the USA, two in the UK, one in Canada, and one in the United Arab Emirates). Patients received corrected. The corrected version asfotase alfa (1 mg/kg three times per week subcutaneously, adjusted to 3 mg/kg three times per week if required) for first appeared at thelancet. up to 7 years (primary treatment period plus extension phase) or until the product became commercially available; com/diabetes-endocrinology on January 22, 2019 dosage adjustments were made at each visit according to changes in the patient’s weight. The primary objectives of See Comment page 76 this extension study were to assess the long-term tolerability of asfotase alfa, defined as the number of patients with Center for Metabolic Bone one or more treatment-emergent adverse events, and skeletal manifestations associated with hypophosphatasia, Disease and Molecular evaluated using the Radiographic Global Impression of Change (RGI-C) scale (−3 indicating severe worsening, and Research, Shriners Hospital for +3 complete or near-complete healing). -

Asfotase Alfa (Strensiq) for Treatment of Hypophosphatasia in Infants and Children
AHRQ Healthcare Horizon Scanning System – Potential High-Impact Interventions Report Priority Area 08: Functional Limitations and Disability Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov Contract No. HHSA290-2010-00006-C Prepared by: ECRI Institute 5200 Butler Pike Plymouth Meeting, PA 19462 December 2015 Statement of Funding and Purpose This report incorporates data collected during implementation of the Agency for Healthcare Research and Quality (AHRQ) Healthcare Horizon Scanning System by ECRI Institute under contract to AHRQ, Rockville, MD (Contract No. HHSA290-2010-00006-C). The findings and conclusions in this document are those of the authors, who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. This report’s content should not be construed as either endorsements or rejections of specific interventions. As topics are entered into the System, individual topic profiles are developed for technologies and programs that appear to be close to diffusion into practice in the United States. Those reports are sent to various experts with clinical, health systems, health administration, and/or research backgrounds for comment and opinions about potential for impact. The comments and opinions received are then considered and synthesized by ECRI Institute to identify interventions that experts deemed, through the comment process, to have potential for high impact. Please see the methods section for more details about this process. -

Transaction Drug 1St (DIN) 2Nd (PIN) 3Rd (PIN) 4Th (PIN) 5Th (PIN) 6Th
Transaction Drug 1st (DIN) 2nd (PIN) 3rd (PIN) 4th (PIN) 5th (PIN) 6th (PIN) 7th (PIN) 8th (PIN) 9th (PIN) 10th (PIN) 11th (PIN) 12th (PIN) 13th (PIN) Alectinib (Alecensaro®) 02458136 00904400 − − − − − − − − − − − 150 mg capsule Alemtuzumab (LemtradaTM) 02418320 00904161 00904162 00904163 00904164 00904165 00904166 00904167 − − − − − 12 mg / 1.2 mL single-use vial Asfotase alfa (Strensiq®) 02444615 00904483 00904484 00904485 − − − − − − − − − 18 mg / 0.45 mL single-use vial Asfotase alfa (Strensiq®) 02444623 00904486 00904487 00904488 00904489 00904490 − − − − − − − 28 mg / 0.7 mL single-use vial Asfotase alfa (Strensiq®) 02444631 00904491 00904492 00904493 − − − − − − − − − 40 mg / 1 mL single-use vial Asfotase alfa (Strensiq®) 02444658 00904494 00904495 00904496 00904497 00904498 00904499 00904500 00904501 00904502 00904504 00904505 − 80 mg / 0.8 mL single-use vial Canakinumab (Ilaris®) 150 mg/mL powder for solution 02344939 00904404 00903809 00904410 − − − − − − − − − for injection Canakinumab (Ilaris®) 02460351 00904405 00904411 00904412 − − − − − − − − − 150 mg/mL solution for injection Ceftolozane / Tazobactam 02446901 00904433 − − − − − − − − − − − (Zerbaxa®) 1 g / 0.5 g vial Cerliponase Alfa (Brineura®) 150 mg / 5 mL solution for 02484013 00904634 00904635 00904636 − − − − − − − − − intracerebroventricular infusion Cladribine (MavencladTM) 02470179 00904524 00904525 00904526 00904642 − − − − − − − − 10 mg tablet Cysteamine (ProcysbiTM) 02464713 00904354 00904355 − − − − − − − − − − 75 mg delayed-release capsule Daclastavir (DaklinzaTM)