SSAT ABSITE Review: Endocrine Adrenal, Thyroid, Parathyroid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Expression Pattern of Delta-Like 1 Homolog in Developing Sympathetic Neurons and Chromaffin Cells
Published in "Gene Expression Patterns 30: 49–54, 2018" which should be cited to refer to this work. Expression pattern of delta-like 1 homolog in developing sympathetic neurons and chromaffin cells ∗ Tehani El Faitwria,b, Katrin Hubera,c, a Institute of Anatomy & Cell Biology, Albert-Ludwigs-University Freiburg, Albert-Str. 17, 79104, Freiburg, Germany b Department of Histology and Anatomy, Faculty of Medicine, Benghazi University, Benghazi, Libya c Department of Medicine, University of Fribourg, Route Albert-Gockel 1, 1700, Fribourg, Switzerland ABSTRACT Keywords: Delta-like 1 homolog (DLK1) is a member of the epidermal growth factor (EGF)-like family and an atypical notch Sympathetic neurons ligand that is widely expressed during early mammalian development with putative functions in the regulation Chromaffin cells of cell differentiation and proliferation. During later stages of development, DLK1 is downregulated and becomes DLK1 increasingly restricted to specific cell types, including several types of endocrine cells. DLK1 has been linked to Adrenal gland various tumors and associated with tumor stem cell features. Sympathoadrenal precursors are neural crest de- Organ of Zuckerkandl rived cells that give rise to either sympathetic neurons of the autonomic nervous system or the endocrine Development ffi Neural crest chroma n cells located in the adrenal medulla or extraadrenal positions. As these cells are the putative cellular Phox2B origin of neuroblastoma, one of the most common malignant tumors in early childhood, their molecular char- acterization is of high clinical importance. In this study we have examined the precise spatiotemporal expression of DLK1 in developing sympathoadrenal cells. We show that DLK1 mRNA is highly expressed in early sympa- thetic neuron progenitors and that its expression depends on the presence of Phox2B. -

HYPOTHALAMUS – PITUITARY-ADRENAL AXIS Learning Objectives OVERVIEW FUNCTIONAL ANATOMY
Introductory Human Physiology ©copyright Emma Jakoi HYPOTHALAMUS – PITUITARY-ADRENAL AXIS Emma R. Jakoi, Ph.D. Learning objectives • Describe the structural and functional organization of the adrenal gland. • Describe the synthesis and secretion of cortical adrenal hormones. • Describe the mechanism of action and physiologic effects of adrenal hormones. • Explain the control of adrenal hormone synthesis and secretion. Describe the major feedback loops that integrate the hypothalamic axis and body homeostasis. • Explain the physiologic roles of the adrenal hormones in normal physiology. OVERVIEW The adrenal glands maintain homeostasis in response to stress. Three major classes of hormones are secreted by these glands: aldosterone (mineralocorticoid), cortisol (glucocorticoid), DHEA (weak androgen), and catecholamines (epinephrine and norepinephrine). FUNCTIONAL ANATOMY The adrenal gland is located on top of the kidney. Like the pituitary, two distinct tissues merge during development to form the adrenal cortex (glandular tissue) and medulla (modified neuronal tissue) (Fig 1). 1 2 cortex 3 medulla Figure 1. Structure of the adrenal gland. The cortex secretes three steroid hormones: 1. aldosterone, 2. cortisol, 3. a weak androgen, DHEA. The medulla secretes epinephrine (Epi) and norepinephrine (NorEpi). 1 Introductory Human Physiology ©copyright Emma Jakoi MINERALOCORTICOIDS The major mineralocorticoid in humans is aldosterone. Aldosterone is NOT under the hypothalamus- pituitary control and does not mediate a negative feedback to this axis. Aldosterone secretion is increased by the vasoconstrictor, angiotensin II, and by elevated plasma K+ concentration. Elevated plasma Na+ inhibits the secretion of aldosterone. Aldosterone, acts in the kidney to promote secretion of K+ into the urine from the blood and the reabsorption of Na+ from the urine into the blood. -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Radiotherapy of Malignant Pheochromocytoma—A Case Report
Case Report Page 1 of 7 Radiotherapy of malignant pheochromocytoma—a case report Chi-Yuan Yeh Department of Radiation Oncology, Tungs’ Taichung Metroharbor Hospital, Taichung, Taiwan Correspondence to: Department of Radiation Oncology, Tungs’ Taichung Metroharbor Hospital, No.699, Sec. 8, Taiwan Blvd., Taichung City 435, Taiwan. Email: [email protected]. Abstract: Pheochromocytomas (PCC) are rare tumors with an estimated incidence of 0.4 to 9.5 cases per 1 million per year. About 5–26% of PCC are malignant and presents with metastasis, for which there is currently no effective therapy. The treatment of choice is for PCC is radical surgery to reduce tumor burden, to provide symptomatic relief of catecholamine excess although complete eradication of the lesions is often not feasible. A number of case reports have been published on the role of radiotherapy for the treatment of PCC. Here we present a 53-year-old male stage III malignant PCC patient who received postoperative adjuvant radiotherapy. A review of current literature is also presented. Keywords: Radiotherapy; pheochromocytoma (PCC); malignant pheochromocytoma; hypertension Received: 12 December 2018; Accepted: 12 August 2019; Published: 27 August 2019. doi: 10.21037/tro.2019.08.02 View this article at: http://dx.doi.org/10.21037/tro.2019.08.02 Introduction reaction confirmed PCC. The term PCC was derived from the Greek words Pheochromocytomas (PCC) and paragangliomas (PGL) phaios (“dusky”), chroma (“color”), and cytoma (“tumor”). are rare catecholamine-secreting tumors that arise from The dark staining reaction of PCC tumor was caused by the chromaffin cells of the adrenal medulla and the sympathetic oxidation of intracellular catecholamines when stained with ganglia respectively. -

Gross Anatomy of the Suprarenal Glands
Edited by: Malak Shalfawi, Noor Adnan Gross Anatomy of the suprarenal glands 5/10/2020 Dr. shatarat. The University of Jordan In the sagittal section below, you can see the retroperitoneal space (encircled by a blue line), which contains structures that lie deep on the posterior abdominal wall and are called retroperitoneal structures, they are the kidneys and suprarenal (adrenal) glands. ➔ The adrenal glands are two small triangular structures located retroperitoneally at the upper poles of the kidneys. [notice the black arrow] 5/10/2020 Dr. shatarat. The University of Jordan You can again notice the kidneys (lying on the posterior abdominal wall and covered by fat), The peritoneum and retroperitoneal space. ➔ The adrenal glands are covered with a thick connective tissue capsule from which the trabeculae extend into the parenchyma carrying blood vessels and nerves. **Extra note: all soft structures in the abdomen, such as the spleen, kidneys and suprarenal glands, have hilum into which all blood vessels and nerve supply getting in or out of them. But each one of these soft structures has its specific modifications on its In this section, you can see the hilum. For example, the ureter getting vertebral column and the muscles of out from the kidneys. the posterior abdominal wall (quadratus lumborum and Psoas 5/10/2020 Dr. shatarat. The University of Jordan major) ➔ Adrenal glands are found on the posterior parietal wall, on each side of the vertebral column, at the level of the 11th thoracic rib and lateral to the first lumber vertebra. They are in the upper part of the abdomen, almost near the diaphragm, NOT in the middle and NOT inferior!!!! ➔ They have flattened triangular shape and are embedded in the perirenal fat at the superior poles of the kidneys. -

Synchronous Primary Hyperparathyroidism and Papillary Thyroid Carcinoma in a 50-Year-Old Female, Who Initially Presented with Uncontrolled Hypertension
Open Access http://www.jparathyroid.com Journal of Journal of Parathyroid Disease 2014,2(2),69–70 Epidemiology and Prevention Synchronous primary hyperparathyroidism and papillary thyroid carcinoma in a 50-year-old female, who initially presented with uncontrolled hypertension Seyed Seifollah Beladi Mousavi1, Hamid Nasri2*, Saeed Behradmanesh3 hough, the association between parathyroid and Implication for health policy/practice/research/ thyroid diseases is not uncommon, however medical education concurrent presence of parathyroid adenoma An association between parathyroid adenoma Tand thyroid cancer is rare (1,2). The association between and thyroid cancer is rare. Awareness of this concurrent thyroid and parathyroid disease was firstly situation will enable clinicians to consider for explained by Kissin et al. in 1947 (2). Awareness of possible thyroid pathology in patients with primary this situation will enable clinicians to consider for hyperparathyroidism. Both of these endocrine diseases possible thyroid pathology in patients with primary could then be managed with a single surgery involving hyperparathyroidism. While thyroid follicular cells and concomitant resection of the thyroid and involved parathyroid cells are embryologically different. It is evident parathyroid glands. that presence of parathyroid adenoma leading to primary hyperparathyroidism and coexistent of thyroid papillary cancer is rare. Both of these endocrine diseases could then coincidence of papillary thyroid carcinoma. After surgery, be managed with a single surgery involving concomitant serum parathormone and calcium returned to their normal resection of the thyroid and involved parathyroid glands. values and patient was referred to an endocrinologist for A 50-year-old female, referred to the nephrology clinic for continuing the treatment of papillary carcinoma. -

Parathyroid Carcinoma Presenting As an Acute Pancreatitis
International Journal of Radiology & Radiation Therapy Case Report Open Access Parathyroid carcinoma presenting as an acute pancreatitis Abstract Volume 3 Issue 3 - 2017 Parathyroid carcinoma is the cause of only 1% of hyperparathyroidism cases. The Enrique Cadena,1,2,3 Alfredo Romero-Rojas1,3 incidence of acute pancreatitis in patients with hyperparathyroidism was reported to 1Department of Head and Neck Surgery and Pathology, be only 1.5%. The occurrence of pancreatitis in patients with parathyroid carcinoma National Cancer Institute, Colombia is unusual, ranging from 0% to 15%. Here, we report a very rare case of parathyroid 2Department of Surgery, National University of Colombia, carcinoma presenting as an acute pancreatitis in a 45years old woman, who was Colombia suspected for hypercalcemia and higher levels of intact parathyroid hormone. The 3Department of Head and Neck Surgery and Pathology, Marly parathyroid carcinoma was verified with ultrasound, CT Scan, and single-photon Clinic, Colombia emission computed tomography. The pathological anatomy report showed a minimally invasive parathyroid carcinoma. Following surgery, the patient was free after almost Correspondence: Enrique Cadena, Department of Head and a 4years follow up. Neck Surgery and Pathology, National Cancer Institute, Bogotá, 1st Street # 9-85, Colombia, Tel 5713341111, 5713341478, Keywords: acute necrotizing pancreatitis, hypercalcemia, primary Email [email protected] hyperparathyroidism, parathyroid carcinoma Received: May 29, 2017 | Published: June 27, 2017 Abbreviations: HPT, hyperparathyroidism; PHPT, primary (2.5mg/dl) levels. Kidney and liver function tests, albumin and hyperparathyroidism; SPECT, single-photon emission computed to- triglyceride levels were all within normal limits. The patient was mography; CT, computed tomography; iPTH, intact parathyroid hor- treated initially with intravenous fluids and H2 blockers, and no oral mone. -

The Adrenal Capsule Is a Signaling Center Controlling Cell Renewal and Zonation Through Rspo3
Downloaded from genesdev.cshlp.org on September 24, 2021 - Published by Cold Spring Harbor Laboratory Press RESEARCH COMMUNICATION The permanent cortex is formed through recruitment of The adrenal capsule is a capsular cells in a process that involves SHH signaling signaling center controlling (King et al. 2009). By E17.5, steroidogenic cells have adopted specific expression profiles, with the outermost cell renewal and zonation cell layers (zona glomerulosa [ZG]) producing enzymes Rspo3 that are required for mineralocorticoid production (e.g., through CYP11B2), and deeper layers (zona fasciculata [ZF]) Valerie Vidal,1,2,3,9 Sonia Sacco,1,2,3,9 expressing genes involved in glucocorticoid synthesis Ana Sofia Rocha,1,2,3,8 Fabio da Silva,1,2,3 (Cyp11b1). In humans, but not rodents, a third layer (zona reticularis) can be distinguished that produces an- Clara Panzolini,1,2,3 Typhanie Dumontet,4,5 1,2,3 6 drogens and is located close to the medulla. Several lines Thi Mai Phuong Doan, Jingdong Shan, of evidence suggest that β-catenin plays an important Aleksandra Rak-Raszewska,6 Tom Bird,7 role in adrenal zonation and maintenance. Activation of Seppo Vainio,6 Antoine Martinez,4,5 the β-catenin pathway is restricted to the ZG (Kim et al. and Andreas Schedl1,2,3 2008; Walczak et al. 2014), and ectopic expression leads to the activation of ZG markers in ZF cells (Berthon 1Institute of Biology Valrose, Université de Nice-Sophia, F-06108 et al. 2010). Moreover, β-catenin seems to bind to and con- Nice, France; 2UMR1091, Institut National de la Santé et de la trol the expression of At1r, a gene specifically expressed Recherche Médicale, F-06108 Nice, France; 3CNRS, UMR7277, within the ZG (Berthon et al. -

Histogenesis of Suprarenal Glands at Different Gestational Age Groups
ORIGINAL ARTICLE ASIAN JOURNAL OF MEDICAL SCIENCES Histogenesis of suprarenal glands at different gestational age groups Ravindra Kumar Boddeti1, Subhadra Devi Velichety2 1Lecturer, 2Professor and Head, Department of Anatomy, Sri Padmavathi Medical College for Women, Sri Venkateswara Institute of Medical Sciences, SVIMS University, Tirupathi, Andhra Pradesh, India Submitted: 22-02-2019 Revised: 10-03-2019 Published: 01-05-2019 ABSTRACT Background: The human foetal suprarenal gland is structurally variant from its adult Access this article online counterpart. The most distinctive features of human foetal suprarenal gland and histologically Website: unique foetal zone, was described first by Elliott and Armour in 1911. After the first trimester, the centrally located foetal zone accounts for most of the foetal adrenal mass. The outer zone http://nepjol.info/index.php/AJMS of the foetal suprarenal gland is called the “definitive zone or neo cortex”; this zone likely DOI: 10.3126/ajms.v10i3.22820 gives rise to the adult adrenal glomerulosa. A third zone called “transitional zone”, lies just E-ISSN: 2091-0576 2467-9100 between the neocortex and foetal zone and is believed to develop into the zona fasciculata. P-ISSN: Aims and Objectives: The current study was designed to study the histogenesis of suprarenal glands at different gestational age groups. Materials and Methods: Twenty-eight formalin preserved dead embryos and foetuses of both sexes, were obtained from the Govt. Maternity Hospital & S.V.Medical College, Tirupati, Andhra Pradesh, India. Specimens were grouped according to their gestational age groups (A,B,C,D) A= 0-12 weeks, B= 13-24 weeks, C= 25-36 weeks and D= more than 36 weeks of gestation. -

Pig Gonads, Adrenal Glands and Brain C
Immunoreactive cytochrome P-45017\g=a\in rat and guinea- pig gonads, adrenal glands and brain C. Le Goascogne1, N. Sanan\l=e'\s1, M. Gou\l=e'\zou1, S. Takemori2, S. Kominami2, E. E. Baulieu1 and P. Robel1 1INSERM U33, Communications Hormonales, and Faculté de Médecine, Université Paris-sud, Lab Hormones F-94275 Bicêtre Cedex France 2 Faculty of Integrated Arts and Sciences, Hiroshima University, Hiroshima 730, Japan Summary. The cytochrome P-45017\g=a\-hydroxylase, 17\ar=r\20lyase (P-45017\g=a\) is the key enzyme responsible for the biosynthesis of androgens in steroidogenic organs. Its cellular localization has been examined with an immunohistochemical technique. In immature rat ovary, P-45017\g=a\was first detected in sparse interstitial cells on postnatal Day 8. The number of immunoreactive interstitial cells increased thereafter and the intensity of P-45017\g=a\staining in these cells was highest at 3 weeks of age. The intensity of staining then started to decline and was very faint at Day 35. From 6 weeks on, the distribution of immunoreactive P-45017\g=a\was of the adult type: it was detected exclusively in the thecal cells of the large antral, preovulatory, follicles. P-45017\g=a\was not detectable during pregnancy except on the day of parturition, when thecal cells were transiently immunoreactive. The staining had vanished 24 h after delivery. Human chorionic gonadotrophin (hCG), injected into immature females on Days 24 to 26, induced P-45017\g=a\prematurely in thecal cells. When injected on Days 12 to 14 of pregnancy, hCG also induced P-45017\g=a\in the thecal cells surrounding the largest follicles, whereas the interstitial and luteal cells were not immunostained. -

Adrenal Gland Hormones
CHAPTER 8 Adrenal Gland Hormones Devra K. Dang, PharmD, BCPS, CDE, FNAP | Trinh Pham, PharmD, BCOP | Jennifer J. Lee, PharmD, BCPS, CDE LEARNING OBJECTIVES KEY TERMS AND DEFINITIONS After completing this chapter, you should be able to ACTH (adrenocorticotropic hormone) — a hormone produced 1. Identify the hormones produced by the adrenal glands by the pituitary gland that stimulates 2. Describe the functions of mineralocorticoids and glucocorticoids in the body the adrenal cortex to produce glucocorticoids, mineralocorticoids, 3. Recognize the signs and symptoms of adrenal insuffi ciency and androgens. PART 4. Describe the pharmacological treatment of patients with acute and chronic adrenal Addison ’ s disease — a disorder insuffi ciency in which the adrenal glands do not produce enough steroid hormones. 3 5. Recognize the signs and symptoms of Cushing ’ s syndrome and the result of too Adenoma — a benign much cortisol (noncancerous) tumor of glandular 6. Describe the pharmacologic and nonpharmacologic management of patients with origin. Cushing ’ s syndrome Adrenal insuffi ciency — a term 7. List management strategies for administration of glucocorticoid and mineralocorti- referring to a defi ciency in the levels of adrenal hormones. coid therapy to avoid development of adrenal disorders Aldosterone — the hormone produced by the adrenal glands that regulates the balance of sodium, he adrenal glands are an integral part of the endocrine system, secreting water, and potassium concentrations in the body. T hormones that act throughout the body to regulate functions and promote Corticotropin-releasing homeostasis. In addition to the neurotransmitters epinephrine and norepineph- hormone (CRH) — a hormone rine, the corticosteroids secreted by the adrenal glands are vital to a wide released by the hypothalamus that variety of physiological processes. -
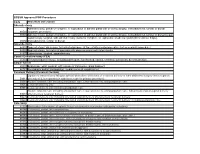
Code Procedure Description Adrenalectomy 60540 Adrenalectomy, Partial Or Complete, Or Exploration of Adrenal Gland with Or Witho
BCBSM Approved POP Procedures Code Procedure Description Adrenalectomy Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal 60540 (separate procedure) 60545 Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal (separate procedure); with excision of adjacent retroperitoneal tumor Laparoscopy, surgical, with adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, 60650 transabdominal, lumbar or dorsal Appendectomy 44955 Appendectomy; when done for indicated purpose at time of other major procedure (not as separate procedure) 44960 Appendectomy; for ruptured appendix with abscess or generalized peritonitis 44970 Laparoscopy, surgical, appendectomy Carotid Endarterectomy (CEA) 35301 Thromboendarterectomy, including patch graft, if performed; carotid, vertebral, subclavian, by neck incision Carpal Tunnel 29848 Endoscopy, wrist, surgical, with release of transverse carpal ligament 64721 Neuroplasty and/or transposition; median nerve at carpal tunnel Cesarean Delivery (Cesarean Section) Ligation or transection of fallopian tube(s) when done at the time of cesarean delivery or intra-abdominal surgery (not a separate 58611 procedure) (List separately in addition to code for primary procedure) 59510 Routine obstetric care including antepartum care, cesarean delivery, and postpartum care 59514 Cesarean delivery only 59515 Cesarean delivery only; including postpartum care