Diagnostic Approach to Soft Tissue Tumors
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Who, How and What of Pathology of Soft Tissue Sarcoma
Editorial Page 1 of 11 Who, how and what of pathology of soft tissue sarcoma Salvatore Lorenzo Renne Anatomic Pathology Unit, Humanitas Research Hospital, Humanitas University, Rozzano, MI 20089, Italy Correspondence to: Salvatore Lorenzo Renne. Adjunct Teaching Professor, Anatomic Pathology Unit, Humanitas Research Hospital, Humanitas University, Via Manzoni 56, Rozzano, MI 20089, Italy. Email: [email protected]. Submitted Aug 06, 2018. Accepted for publication Aug 23, 2018. doi: 10.21037/cco.2018.10.09 View this article at: http://dx.doi.org/10.21037/cco.2018.10.09 Introduction to soft tissue sarcoma (STS) adipocytes (lipoma, spindle cells lipoma, hibernoma, well- pathology differentiated liposarcoma (LPS), myxoid LPS, etc.). One chapter is dedicated to specific entities “of uncertain STS is a generic term that refers to a heterogeneous group differentiation” that are well-characterized entities that do of rare neoplastic diseases. The aim of this review is to not readily resemble any normal mesenchymal cells (as the discuss the role of pathology in the multidisciplinary Ewing sarcoma or the synovial sarcoma—a clear misnomer). management of STS patients. This will be done: (I) The last chapter is dedicated to those sarcomas that do illustrating the framework for the current classification; (II) not follow in any of the previously listed diagnosis and are examining the characteristics that allows an expert diagnosis; therefore called “undifferentiated/unclassified sarcomas” (III) describing the role of the sarcoma pathologist -

Complete Case of a Rare but Benign Soft Tissue Tumor
Hindawi Case Reports in Orthopedics Volume 2019, Article ID 6840693, 5 pages https://doi.org/10.1155/2019/6840693 Case Report Hibernoma of the Upper Extremity: Complete Case of a Rare but Benign Soft Tissue Tumor Thomas Reichel ,1 Kilian Rueckl,1 Annabel Fenwick,1,2 Niklas Vogt,3 Maximilian Rudert,1 and Piet Plumhoff1 1Department of Orthopedic Surgery, Koenig-Ludwig-Haus, University of Wuerzburg, Brettreichstraße 11, 97074 Wuerzburg, Germany 2Department of Trauma Surgery, Klinikum Augsburg, 86156 Augsburg, Germany 3Department of Pathology, University of Wuerzburg, 97080 Wuerzburg, Germany Correspondence should be addressed to Thomas Reichel; [email protected] Received 26 February 2019; Accepted 14 April 2019; Published 21 May 2019 Academic Editor: Elke R. Ahlmann Copyright © 2019 Thomas Reichel et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Hibernoma is a rare benign lipomatous tumor showing differentiation of brown fatty tissue. To the author’s best knowledge, there is no known case of malignant transformation or metastasis. Due to their slow, noninfiltrating growth hibernomas are often an incidental finding in the third or fourth decade of life. The vast majority are located in the thigh, neck, and periscapular region. A diagnostic workup includes ultrasound and contrast-enhanced MRI. Differential diagnosis is benign lipoma, well- differentiated liposarcoma, and rhabdomyoma. An incisional biopsy followed by marginal resection of the tumor is the standard of care, and recurrence after complete resection is not reported. The current paper presents diagnostic and intraoperative findings of a hibernoma of the upper arm and reviews similar reports in the current literature. -

Pleomorphic Adenoma of Buccal Mucosa: a Rare Case Report
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 16, Issue 3 Ver. XI (March. 2017), PP 75-78 www.iosrjournals.org Pleomorphic Adenoma of Buccal Mucosa: A Rare Case Report Ashwini Jangamashetti, BDS1, Siddesh Shenoy, MDS2, R.Krishna Kumar MDS3, Amol Jeur, MS4 1Post Graduate Student, Department Of Oral Medicine And Radiology, MARDC,Pune 2Reader, Department of oral Medicine and radiology, M.A Rangoonwala Dental College and Research Center, Pune (MARDC), 3Professor and HOD, Department of oral Medicine and Radiology, MARDC, Pune 4Assistant Professor in Department of General surgery, Krishna Medical College of KIMS Deemed University , Abstract: Pleomorphic adenoma is a benign tumor of the salivary gland that consists of a combination of epithelial and mesenchymal elements1. About 90% of these tumors occur in the parotid gland and 10% in the minor salivary glands2. Among intra oral pleomorphic adenomas buccal vestibule is among the rarest sites3. A case of pleomorphic adenoma of minor salivary glands in the buccal vestibule in a 36 year-old female is discussed4. It includes review of literature, clinical features, histopathology, radiological findings and treatment of the tumor, with emphasis on diagnosis4. The mass was removed by wide local excision with adequate margins5. Keywords: minor salivary gland, pleomorphic adenoma, tumor, parotid gland, vestibule, mesenchymal elements. I. Introduction Pleomorphic adenoma (PA) is defined by World Health Organization in 1972 as a circumscribed tumor characterized by its pleomorphic or mixed appearance clearly recognizable epithelial tissue being intermingled with tissue of mucoid, myxoid and chondroid appearance2. Among all salivary gland tumors, pleomorphic adenoma is the most frequently encountered lesion accounting for approximately 60% of all salivary gland neoplasms3. -

A Case Report1 양측 흉막에 발생한 결합조직형성 소원형세포종양의 증례 보고1
Case Report pISSN 1738-2637 / eISSN 2288-2928 J Korean Soc Radiol 2015;72(4):295-299 http://dx.doi.org/10.3348/jksr.2015.72.4.295 Bilateral Presentation of Pleural Desmoplastic Small Round Cell Tumors: A Case Report1 양측 흉막에 발생한 결합조직형성 소원형세포종양의 증례 보고1 You Sun Won, MD1, Jai Soung Park, MD1, Sun Hye Jeong, MD1, Sang Hyun Paik, MD1, Heon Lee, MD1, Jang Gyu Cha, MD1, Eun Suk Koh, MD2 Departments of 1Radiology, 2Pathology, Soonchunhyang University College of Medicine, Bucheon Hospital, Bucheon, Korea Desmoplastic small round cell tumor (DSRCT) is a highly aggressive malignant small cell neoplasm occurring mainly in the abdominal cavity, but it is extremely rare in Received October 13, 2014; Accepted December 21, the pleura. In this case, a 15-year-old male presented with a 1-month history of left 2014 chest pain. Chest radiographs revealed pleural thickening in the left hemithorax and Corresponding author: Jai Soung Park, MD Department of Radiology, Soonchunhyang University chest computed tomography showed multifocal pleural thickening with enhance- College of Medicine, Bucheon Hospital, 170 Jomaru-ro, ment in both hemithoraces. A needle biopsy of the left pleural lesion was performed Wonmi-gu, Bucheon 420-767, Korea. and the final diagnosis was DSRCT of the pleura. We report this unusual case aris- Tel. 82-32-621-5851 Fax. 82-32-621-5874 E-mail: [email protected] ing from the pleura bilaterally. The pleural involvement of this tumor supports the hypothesis that it typically occurs in mesothelial-lined surfaces. This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) Index terms which permits unrestricted non-commercial use, distri- Pleura bution, and reproduction in any medium, provided the Thickened Pleura original work is properly cited. -

Nodular Fasciitis of the Pectoralis Muscle in a 54-Year-Old Woman
ACS Case Reviews in Surgery Vol. 2, No. 3 Nodular Fasciitis of the Pectoralis Muscle in a 54-Year-Old Woman AUTHORS: CORRESPONDENCE AUTHOR: AUTHOR AFFILIATIONS: Christopher D. Kannera; Divya Sharma, MDb; Dr. Jaime D Lewis a. Medical Student, University of Cincinnati College Jaime D Lewis, MD, FACSc UC Health Women’s Center of Medicine, Cincinnati, Ohio 7675 Wellness Way b. Department of Pathology and Laboratory West Chester, Ohio 45069 Medicine, University of Cincinnati College of Phone: (513) 584-8900 Medicine, Cincinnati, Ohio Email: [email protected] c. Department of Surgery, University of Cincinnati College of Medicine, Cincinnati, Ohio Background A 54-year-old woman presented with a breast mass found to be nodular fasciitis of the right pectoralis muscle. Summary A 54-year-old woman presented to a breast surgeon for evaluation of a painful right breast mass. Initial mammography was unrevealing. Ultrasound revealed a right pectoral mass extending into the soft tissue of the breast. Core needle biopsy specimen revealed features suggestive of low grade sarcoma. Findings on computed tomography (CT) and magnetic resonance imaging (MRI) were nonspecific and wide local excision was subsequently performed. Pathologic characteristics were consistent with nodular fasciitis. This benign proliferation of fibroblasts and myofibroblasts frequently raises concern for malignant neoplasms due to its rapid, infiltrative growth, and nonspecific imaging characteristics. Thus, it is often identified by its characteristic features on surgical pathology following excision. On rare occasions when it is managed with surveillance, nodular fasciitis frequently demonstrates spontaneous regression. Conclusion Nodular fasciitis is a benign growth with a tendency for spontaneous regression, which exhibits clinical features that often invoke suspicion of malignancy. -

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -

The Use of High Tumescent Power Assisted Liposuction in the Treatment of Madelung’S Collar
Letter to the Editor The use of high tumescent power assisted liposuction in the treatment of Madelung’s collar Henryk Witmanowski1,2, Łukasz Banasiak1, Grzegorz Kierzynka1, Jarosław Markowicz1, Jerzy Kolasiński1, Katarzyna Błochowiak3, Paweł Szychta1,4 1Department of Plastic, Reconstructive and Aesthetic Surgery, Medical College in Bydgoszcz, Nicolaus Copernicus University in Torun, Poland 2Department of Physiology, Poznan University of Medical Sciences, Poznan, Poland 3Department of the Oral Surgery, Poznan University of Medical Sciences, Poznan, Poland 4Department of Oncological Surgery and Breast Diseases, Polish Mother’s Memorial Hospital-Research Institute, Lodz, Poland Adv Dermatol Allergol 2017; XXXIV (4): 366–371 DOI: https://doi.org/10.5114/ada.2017.69319 Mild symmetrical lipomatosis (plural symmetrical The disease most commonly takes a proximal form lipomatosis, multiple symmetric lipomatosis – MSL), which takes the following areas of the body with the fol- also known as Madelung’s disease or Launois-Bensaude lowing frequency: the genial area 92.3%, cervical region syndrome is a rare disease of unknown etiology, first de- 67.7%, shoulder region 54.8%, abdominal 45.2%, chest scribed by Brodie in 1846, Madelung in 1888, and Launois 41.9%, thigh and pelvic rim 32.3% [11, 12]. The periph- with Bensaude in 1898 [1–3]. eral type mainly locates on both sides at the level of the Madelung’s disease incidence is 1 : 250000 [4]. Mul- hands, feet and knees, this is definitely a rarer form of tiple symmetric lipomatosis occurs mainly in the inhabit- the disease. The mixed form is described very rarely. The ants of the Mediterranean area and Eastern Europe, in specified central type is also engaged primarily around males (male to female ratio is 20 : 1), aged 30–70 years, the lower torso, and intermediate parts of the legs. -

Well-Differentiated Spindle Cell Liposarcoma
Modern Pathology (2010) 23, 729–736 & 2010 USCAP, Inc. All rights reserved 0893-3952/10 $32.00 729 Well-differentiated spindle cell liposarcoma (‘atypical spindle cell lipomatous tumor’) does not belong to the spectrum of atypical lipomatous tumor but has a close relationship to spindle cell lipoma: clinicopathologic, immunohistochemical, and molecular analysis of six cases Thomas Mentzel1, Gabriele Palmedo1 and Cornelius Kuhnen2 1Dermatopathologie, Friedrichshafen, Germany and 2Institute of Pathology, Medical Center, Mu¨nster, Germany Well-differentiated spindle cell liposarcoma represents a rare atypical/low-grade malignant lipogenic neoplasm that has been regarded as a variant of atypical lipomatous tumor. However, well-differentiated spindle cell liposarcoma tends to occur in subcutaneous tissue of the extremities, the trunk, and the head and neck region, contains slightly atypical spindled tumor cells often staining positively for CD34, and lacks an amplification of MDM2 and/or CDK4 in most of the cases analyzed. We studied a series of well-differentiated spindle cell liposarcomas arising in two female and four male patients (age of the patients ranged from 59 to 85 years). The neoplasms arose on the shoulder, the chest wall, the thigh, the lower leg, the back of the hand, and in paratesticular location. The size of the neoplasms ranged from 1.5 to 10 cm (mean: 6.0 cm). All neoplasms were completely excised. The neoplasms were confined to the subcutis in three cases, and in three cases, an infiltration of skeletal muscle was seen. Histologically, the variably cellular neoplasms were composed of atypical lipogenic cells showing variations in size and shape, and spindled tumor cells with slightly enlarged, often hyperchromatic nuclei. -

The Health-Related Quality of Life of Sarcoma Patients and Survivors In
Cancers 2020, 12 S1 of S7 Supplementary Materials The Health-Related Quality of Life of Sarcoma Patients and Survivors in Germany—Cross-Sectional Results of A Nationwide Observational Study (PROSa) Martin Eichler, Leopold Hentschel, Stephan Richter, Peter Hohenberger, Bernd Kasper, Dimosthenis Andreou, Daniel Pink, Jens Jakob, Susanne Singer, Robert Grützmann, Stephen Fung, Eva Wardelmann, Karin Arndt, Vitali Heidt, Christine Hofbauer, Marius Fried, Verena I. Gaidzik, Karl Verpoort, Marit Ahrens, Jürgen Weitz, Klaus-Dieter Schaser, Martin Bornhäuser, Jochen Schmitt, Markus K. Schuler and the PROSa study group Includes Entities We included sarcomas according to the following WHO classification. - Fletcher CDM, World Health Organization, International Agency for Research on Cancer, editors. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013. 468 p. (World Health Organization classification of tumours). - Kurman RJ, International Agency for Research on Cancer, World Health Organization, editors. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: International Agency for Research on Cancer; 2014. 307 p. (World Health Organization classification of tumours). - Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur Urol. 2016 Jul;70(1):106–19. - World Health Organization, Swerdlow SH, International Agency for Research on Cancer, editors. WHO classification of tumours of haematopoietic and lymphoid tissues: [... reflects the views of a working group that convened for an Editorial and Consensus Conference at the International Agency for Research on Cancer (IARC), Lyon, October 25 - 27, 2007]. 4. ed. -

A Comparison of Imaging Modalities for the Diagnosis of Osteomyelitis
A comparison of imaging modalities for the diagnosis of osteomyelitis Brandon J. Smith1, Grant S. Buchanan2, Franklin D. Shuler2 Author Affiliations: 1. Joan C Edwards School of Medicine, Marshall University, Huntington, West Virginia 2. Marshall University The authors have no financial disclosures to declare and no conflicts of interest to report. Corresponding Author: Brandon J. Smith Marshall University Joan C. Edwards School of Medicine Huntington, West Virginia Email: [email protected] Abstract Osteomyelitis is an increasingly common pathology that often poses a diagnostic challenge to clinicians. Accurate and timely diagnosis is critical to preventing complications that can result in the loss of life or limb. In addition to history, physical exam, and laboratory studies, diagnostic imaging plays an essential role in the diagnostic process. This narrative review article discusses various imaging modalities employed to diagnose osteomyelitis: plain films, computed tomography (CT), magnetic resonance imaging (MRI), ultrasound, bone scintigraphy, and positron emission tomography (PET). Articles were obtained from PubMed and screened for relevance to the topic of diagnostic imaging for osteomyelitis. The authors conclude that plain films are an appropriate first step, as they may reveal osteolytic changes and can help rule out alternative pathology. MRI is often the most appropriate second study, as it is highly sensitive and can detect bone marrow changes within days of an infection. Other studies such as CT, ultrasound, and bone scintigraphy may be useful in patients who cannot undergo MRI. CT is useful for identifying necrotic bone in chronic infections. Ultrasound may be useful in children or those with sickle-cell disease. Bone scintigraphy is particularly useful for vertebral osteomyelitis. -
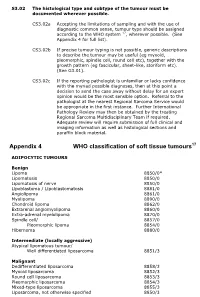
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

Soft Tissue Tumor Pathology: New Diagnostic Immunohistochemical Markers Leona A
S EMINARS IN D IAGNOSTIC P ATHOLOGY ] (2015) ]]]– ]]] Available online at www.sciencedirect.com www.elsevier.com/locate/semdp Soft tissue tumor pathology: New diagnostic immunohistochemical markers Leona A. Doyle, MD Department of Pathology, Brigham and Women's Hospital and Harvard Medical School, 75 Francis St, Boston, Massachusetts article info abstract Keywords: Recent insights into the pathogenesis of various soft tissue tumors, along with the Soft tissue identification of recurrent molecular alterations characteristic of specific tumor types, Tumor have resulted in the development of many diagnostically useful immunohistochemical Sarcoma markers. In some cases, expression of these markers is significantly associated with Immunohistochemistry distinctive clinical and histologic features, which may impart prognostic or predictive Molecular genetics information. This review outlines new diagnostic immunohistochemical markers in soft tissue tumor pathology, emphasizing their utility in clinical practice and potential pitfalls, molecular correlates and clinical associations. & 2015 Elsevier Inc. All rights reserved. Introduction shows MYC amplification. Finally, so-called lineage specific markers, which tend to show nuclear staining and in general fi Over the last 10 years, many novel immunohistochemical are not strictly speci c to a given lineage, have also emerged markers for use in the evaluation of soft tissue tumors have as useful markers, not only in soft tissue pathology but also been described. This has largely been due to new insights