Nodular Fasciitis of the Pectoralis Muscle in a 54-Year-Old Woman
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -
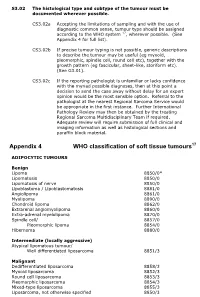
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

2016 Essentials of Dermatopathology Slide Library Handout Book
2016 Essentials of Dermatopathology Slide Library Handout Book April 8-10, 2016 JW Marriott Houston Downtown Houston, TX USA CASE #01 -- SLIDE #01 Diagnosis: Nodular fasciitis Case Summary: 12 year old male with a rapidly growing temple mass. Present for 4 weeks. Nodular fasciitis is a self-limited pseudosarcomatous proliferation that may cause clinical alarm due to its rapid growth. It is most common in young adults but occurs across a wide age range. This lesion is typically 3-5 cm and composed of bland fibroblasts and myofibroblasts without significant cytologic atypia arranged in a loose storiform pattern with areas of extravasated red blood cells. Mitoses may be numerous, but atypical mitotic figures are absent. Nodular fasciitis is a benign process, and recurrence is very rare (1%). Recent work has shown that the MYH9-USP6 gene fusion is present in approximately 90% of cases, and molecular techniques to show USP6 gene rearrangement may be a helpful ancillary tool in difficult cases or on small biopsy samples. Weiss SW, Goldblum JR. Enzinger and Weiss’s Soft Tissue Tumors, 5th edition. Mosby Elsevier. 2008. Erickson-Johnson MR, Chou MM, Evers BR, Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X, Oliveira AM. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011 Oct;91(10):1427-33. Amary MF, Ye H, Berisha F, Tirabosco R, Presneau N, Flanagan AM. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013 Jul;463(1):97-8. CONTRIBUTED BY KAREN FRITCHIE, MD 1 CASE #02 -- SLIDE #02 Diagnosis: Cellular fibrous histiocytoma Case Summary: 12 year old female with wrist mass. -

Immunohistochemistry in Diagnosis of Soft Tissue Tumours Cyril Fisher
Immunohistochemistry in Diagnosis of Soft Tissue Tumours Cyril Fisher To cite this version: Cyril Fisher. Immunohistochemistry in Diagnosis of Soft Tissue Tumours. Histopathology, Wiley, 2010, 58 (7), pp.1001. 10.1111/j.1365-2559.2010.03707.x. hal-00613811 HAL Id: hal-00613811 https://hal.archives-ouvertes.fr/hal-00613811 Submitted on 6 Aug 2011 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Histopathology Immunohistochemistry in Diagnosis of Soft Tissue Tumours ForJournal: Histopathology Peer Review Manuscript ID: HISTOP-08-10-0420 Wiley - Manuscript type: Review Date Submitted by the 01-Aug-2010 Author: Complete List of Authors: fisher, cyril; royal marsden hospital, histopathology Keywords: soft tissue tumours, immunohistochemistry, sarcoma, diagnosis Published on behalf of the British Division of the International Academy of Pathology Page 1 of 39 Histopathology Immunohistochemistry in Diagnosis of Soft Tissue Tumours For PeerCyril FisherReview Royal Marsden Hospital, London UK Correspondence to: Prof Cyril Fisher MD DSc FRCPath Dept of Histopathology The Royal Marsden Hospital 203 Fulham Road London SW3 6JJ UK Email: [email protected] Tel: +44 207 808 2631 Fax +44 207 808 2578 Running Title : Soft Tissue Tumour Immunohistochemistry Key Words Immunohistochemistry, sarcoma, diagnosis, soft tissue tumour 1 Published on behalf of the British Division of the International Academy of Pathology Histopathology Page 2 of 39 Abstract Immunohistochemistry in soft tissue tumours, and especially sarcomas, is used to identify differentiation in the neoplastic cells. -

Bone and Soft Tissue Pathology Specimens and 127 Surgicals (Biopsies and Resections)
ANNUAL MEETING ABSTRACTS 11A the morphologic spectrum and etiology of DAD encountered during adult autopsy in (non-EWSR1) NR4A3 gene fusions (TAF15, TCF12) showed distinctive plasmacytoid an inner city teaching hospital. The diagnostic utility of post mortem lung culture was / rhabdoid morphology, with increased cellularity, cytologic atypia and high mitotic also evaluated. counts. Follow-up showed that only 1 of 16 patients with EWSR1-rearranged tumors Design: A retrospective study was performed on all adult autopsies from July 2010 to died of disease, in contrast to 3 of 7 (43%) patients with TAF15–rearranged tumors. July 2013 with fi nal histopathologic diagnosis of DAD. The histopathological features Conclusions: In conclusion, EMCs with variant NR4A3 gene fusions show a higher of DAD were re-evaluated by one autopsy pathologist and one pathology resident, incidence of rhabdoid phenotype, high grade morphology and a more aggressive based on the duration (exudative or proliferative phase), severity (bilateral/unilateral; outcome compared to the more common EWSR1-NR4A3 positive tumors. Furthermore, focal/extensive) and pattern (classical vs. acute fi brinous and organizing pneumonia as EWSR1 FISH break-apart assay is the preferred ancillary test to confi rm diagnosis aka AFOP). Clinical history, pre and post mortem laboratory investigations, including of EMC, tumors with variant NR4A3 gene fusions remain under-recognized and often postmortem lung culture (for bacteria, mycobacteria, fungi and virus) were reviewed misdiagnosed. FISH assay for NR4A3 rearrangements recognizes >95% of EMCs and to elucidate etiology. should be an additional tool in EWSR1-negative tumors. Results: 36 (16.2 %) cases showed histopathologic features of DAD out of 222 adult autopsies in the three year study period. -

Transgelin Is a Novel Marker of Smooth Muscle Differentiation That Improves Diagnostic Accuracy of Leiomyosarcomas
Modern Pathology (2013) 26, 502–510 502 & 2013 USCAP, Inc All rights reserved 0893-3952/13 $32.00 Transgelin is a novel marker of smooth muscle differentiation that improves diagnostic accuracy of leiomyosarcomas: a comparative immunohistochemical reappraisal of myogenic markers in 900 soft tissue tumors Yves-Marie Robin1, Nicolas Penel2,3, Gae¨lle Pe´rot4,5, Agnes Neuville4,5,6, Vale´rie Ve´lasco4,5, Dominique Ranche`re-Vince7, Philippe Terrier8 and Jean-Michel Coindre4,5,6 1Department of Biology, Unit of Morphological and Molecular Pathology, Centre Oscar Lambret, Lille Cedex, France; 2Department of General Oncology, Centre Oscar Lambret, Lille Cedex, France; 3Research Unit (EA 2694), Medical School University, Lille-Nord-de-France University, Lille Cedex, France; 4Department of Pathology, Institut Bergonie´, Bordeaux Cedex, France; 5INSERM U916, Institut Bergonie´, Bordeaux, France; 6Laboratory of Pathology, Universite´ Victor Segalen Bordeaux 2, Bordeaux, France; 7Department of Patholoy, Centre Le´on Be´rard, Lyon, France and 8Department of Pathology, Institut Gustave Roussy, Villejuif, France Immunohistochemical use of myogenic markers serves to define smooth or skeletal muscle differentiation in soft tissue tumors. Establishing smooth muscle differentiation in malignant lesions can be challenging in some cases. We immunohistochemically examined 900 soft tissue tumors selected from the French Sarcoma Group’s archived tissue collection, which contains a large number of leiomyosarcomas. The four most widely used smooth muscle diagnostic markers were evaluated (smooth muscle actin, desmin, h-caldesmon and calponin), and compared with a novel marker, transgelin. The diagnostic performance of each marker was statistically assessed in terms of sensitivity (Se), specificity (Sp), positive predictive value (PPV), negative predictive value (NPV) and accuracy (A), in leiomyosarcomas versus all other sarcomas including gastrointestinal stromal tumors (GIST), and second in leiomyosarcomas versus specific tumor types. -

FNA/Core Biopsy of Soft Tissue: Let the Category Be Your Guide
FNA/Core Biopsy of Soft Tissue: Let the Category Be Your Guide BENJAMIN L. WITT ASSOCIATE PROFESSOR OF ANATOMIC PATHOLOGY UNIVERSITY OF UTAH/ARUP LABORATORIES Objectives Employ cytomorphology to better differentiate soft tissue lesions into diagnostic categories Implement selected immunohistochemical stains on FNA/core biopsy specimens to work within differential diagnoses of soft tissue lesions Utilize flourescence in situ hybridization (FISH) testing when appropriate on soft tissue lesions Introduction Soft tissue FNA/core biopsy evaluation is a team effort (need to incorporate clinical history, radiology) Cytomorphology can overlap between entities so often IHC and FISH testing are needed Sometimes it’s fine not to be definitive; broad categorization and low grade versus high grade distinction can help guide initial patient management Preoperative radiation typically used for high grade tumors (while it is not for low grade tumors) Some tumors are particular chemosensitive: synovial sarcoma, Ewing sarcoma, rhabdomyosarcoma, among others Cast a Wide Net Sometimes in order to place a lesion into the mesenchymal (soft tissue) category carcinoma, melanoma and lymphoma should be excluded by ancillary studies In general similar IHC/FISH panels can be used for lesions within the same morphologic category (spindle cell lesions for example) Anatomic site can also help direct an ancillary panel (paraspinal good site for nerve sheath tumor for instance) Benign Hints Superficial location Smaller size (<5 cm) Mobile (not fixed) Fluid -

Magnetic Resonance Imaging of Benign Soft Tissue Neoplasms in Adults
Magnetic Resonance Imaging of Benign Soft Tissue Neoplasms in Adults Eric A. Walker, MDa,b,*, Michael E. Fenton, MDc, Joel S. Salesky, MDc, Mark D. Murphey, MDb,c,d KEYWORDS Soft tissue tumor Benign MR imaging Soft tissue neoplasm Benign soft tissue lesions outnumber their malig- tics. Fast-spin echo sequences in place of SE nant counterparts by a factor of 100:1.1,2 Many sequences can reduce scanning time and patient of these lesions are small and superficial and do motion artifacts. Gradient echo sequences can not lead to imaging evaluation or biopsy; so be useful for demonstrating hemosiderin with precise estimates are unavailable. Magnetic reso- “blooming” and also are subject to artifact caused nance (MR) imaging is the favored modality for by metal, hemorrhage, and air. Short tau inversion evaluation of soft tissue tumors and tumorlike recovery and chemical shift–selective fat saturation conditions because of its superior soft tissue T2W images increase sensitivity to abnormal tissue contrast, multiplanar imaging capability, and lack containing increased water content. However, in of radiation exposure. MR imaging is valuable for our opinion, these techniques also reduce infor- lesion detection, diagnosis, and staging. mation concerning various tissue consistencies When planning an MR imaging study for evalua- and should be used in the secondary, not the tion of a soft tissue lesion, at least 2 orthogonal primary, plane of imaging. The smallest diagnostic planes should be obtained. In our experience, field of view is preferable when evaluating these lesions are typically best evaluated in the axial lesions. plane, and this plane is usually the most familiar The use of intravenous contrast for lesion evalu- to radiologists. -

Nodular Fasciitis in a One-Year-Old Male: 1 Lily L
CASE REPORTS PHILIPPINE JOURNAL OF OTOLARYNGOLOGY-HEAD AND NECK SURGERY VOL. 25 NO. 2 JULY – DECEMBER 2010 Adrian F. Fernando, MD1 Antonio H. Chua, MD1,2 Nodular Fasciitis in a One-Year-Old Male: 1 Lily L. Sia-Vargas, MD A Diagnostic Dilemma 1Department of Otorhinolaryngology Head and Neck Surgery ABSTRACT University of the East – Ramon Magsaysay Memorial Medical Center, Inc. Objectives: To present a rare case of nodular fasciitis presenting as a supra-auricular mass. Quezon City, Philippines 2Department of Otorhinolaryngology Methods: Head and Neck Surgery Design: Case Report Jose R. Reyes Memorial Medical Center Setting: Private Tertiary University Hospital Manila, Philippines Patient: One Results: A one-year-old boy presented with an initially painless, left supra-auricular mass that rapidly enlarged from < 1 cm to 3 cm (widest diameter) in a two-month period. Sarcoma was initially considered over an inflammatory process as the mass was non-responsive to antibiotic therapy. Fine-Needle Aspiration Cytology (FNAC) and High-Resolution Computed Tomography (HRCT) with contrast revealed benign cytologic and radiologic findings making nodular fasciitis the primary impression. The patient eventually underwent complete surgical excision of the left supra-auricular mass. Histopathologic findings then showed a stroma rich in collagen and myxoid ground substance and loose array of short S-shaped fascicle cells with scattered lymphocytes, macrophages and red blood cells consistent with nodular fasciitis. Conclusion: Nodular fasciitis is a rare benign myofibroblastic soft tissue tumor which typically presents as a rapidly progressive nodular lesion in the head and neck region of the young pediatric age group. Cytopathologic recognition with FNA is a challenge. -

Primary Pleural Epithelioid Sarcoma of the Proximal Type: a Diagnostic and Therapeutic Challenge
705 Case Report Primary pleural epithelioid sarcoma of the proximal type: a diagnostic and therapeutic challenge Zeeshan Ahmad1, Qasim Stanazai2, Staphanie Wright3, Matthew Smolkin3, Patrick C. Ma4 1Section of Hematology/Oncology, Department of Medicine, West Virginia University School of Medicine, Morgantown, WV, USA; 2Department of Medicine, West Virginia University School of Medicine, Morgantown, WV, USA; 3Section of Molecular Pathology, Department of Pathology, West Virginia University School of Medicine, Morgantown, WV, USA; 4Penn State Cancer Institute, Penn State Health Milton S. Hershey Medical Center, Pennsylvania State University, Hershey, PA, USA Correspondence to: Patrick C. Ma, MD, MSc. Professor of Medicine, Associate Director of Translational Research, Thoracic Oncology Disease Team Leader, Penn State Cancer Institute, Penn State Health Milton S. Hershey Medical Center, Pennsylvania State University, 500 University Drive, Hershey, PA 17033, USA. Email: [email protected]. Abstract: Epithelioid sarcoma (ES) is an uncommon soft tissue neoplasm first described in 1970. It is a unique soft tissue neoplasm of adolescents and younger adults which usually presents as a subcutaneous and deep dermal mass in the distal portions of the extremities. The proximal-type variant of this rare soft tissue neoplasm was only recently reported. The proximal form typically arise in proximal extremities and in the deep parts of pelvis, perineum and genital tract. The proximal type variant has distinct histological characteristics and aggressive clinical course as compared to the distal ES. Inactivation of INI1 has been reported in both distal and proximal variants and can help to make the diagnosis. Furthermore, the proximal variant has a possible association with malignant rhabdoid neoplasm. -

Site Diagnosis Cardiovascular System 659 Heart: 1 Atrial Myxoma 1 Artery
Stony Brook BioBank Specimen Collection (updated 2/11/16) Site Diagnosis Cardiovascular 659 System Heart: 1 Atrial myxoma 1 Artery: 5 Normal 5 Blood: 652 Vein: 1 Leiomyosarcoma well-differentiated (inferior vena cava) 1 Digestive System 508 Appendix: 3 Normal and benign 3 Colon: 242 Adenocarcinoma 74 Adenoma (adenomatous polyp) 14 Crohn's disease 5 Diverticulitis 2 High grade sarcoma/liposarcoma 1 Metastatic poorly differentiated carcinoma 3 Ulcerative Colitis 2 Normal and benign 141 Duodenum: 5 Adenocarcinoma (including signet-ring cell features) 3 Adenomatous polyp 1 GIST 1 Esophagus: 17 Adenocarcinoma 4 Squamous cell carcinoma 2 Normal and benign 11 Gallbladder: 2 Normal and benign 2 Adenocarcinoma (15, including 3 samples with Liver: 35 18 colorectal primary) Cirrhosis 1 Hepatoblastoma 1 Hepatocellular carcinoma 2 Metastatic leiomyosarcoma 1 Normal and benign 12 Parotid: 22 Adenocarcinoma 1 Adenoid cystic carcinoma 1 Cellular pleomorphic adenoma 1 Follicular lymphoma 1 Keratinized squamous cell carcinoma 2 Neuroendocrine carcinoma 1 Warthin's tumor 6 Normal and benign 9 Pancreas: 60 Adenocarcinoma 23 Carcinoid tumor 1 Carcinoma (NOS) 2 Chronic pancreatitis 1 Diffuse large B cell lymphoma 1 Intraductal papillary mucinous neoplasm (IPMN) 2 Microcystic adenoma 1 Mucinous cystadenoma 1 Neuroendocrine tumor 1 Tubulovillous Adenoma of Ampulla of Vater 1 Normal and benign 26 Rectum: 23 Adenocarcinoma 6 Adenoma 1 GIST 1 Invasive squamous cell carcinoma 2 Spindle cell lesion with extensive necrosis 3 Retroperitoneum 4 Fibromatosis 1 Liposarcoma -

The Best Diagnosis Is
Dermatopathology Diagnosis The best diagnosis is: a. chondroma H&E, original magnification 40. b. mixed tumor (chondroid syringoma) c. nerve sheath myxoma (neurothekeoma) CUTISd. nodular fasciitis e. solitary adult myofibroma Do Not Copy H&E, original magnification 100. PLEASE TURN TO PAGE 235 FOR DERMATOPATHOLOGY DIAGNOSIS DISCUSSION L. David Hall, MD; Tammie Ferringer, MD Dr. Hall was from and Dr. Ferringer is from the Department of Dermatology, Geisinger Medical Center, Danville, Pennsylvania. Dr. Ferringer also is from the Department of Laboratory Medicine. Dr. Hall currently is from Ackerman Academy of Dermatopathology, New York, New York. The authors report no conflict of interest. Correspondence: L. David Hall, MD, Ackerman Academy of Dermatopathology, 145 E 32nd St, Floor 10, New York, NY 10016 ([email protected]). WWW.CUTIS.COM VOLUME 93, MAY 2014 225 Copyright Cutis 2014. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. Dermatopathology Diagnosis Discussion Solitary Adult Myofibroma yofibromatosis can be classified based on its syringoma) may simulate myofibroma from low-power clinical presentation as either solitary infan- magnification, but it can be distinguished by the pres- Mtile myofibroma, congenital multiple myofi- ence of tubuloalveolar and ductal structures within the bromatosis without visceral involvement, congenital chondroid stroma (Figure 3). Nerve sheath myxoma generalized myofibromatosis with visceral involve- (neurothekeoma) displays myxoid lobules containing ment, or solitary adult myofibroma. Solitary adult spindle-shaped, stellate, or epithelioid cells (Figure 4), myofibroma is a benign proliferation of myofibroblasts and the lobules are separated by fibrous septa as opposed that most commonly presents as a firm superficial nod- to the hemangiopericytomalike vessels of myofibroma.