View Article
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

A Case Report1 양측 흉막에 발생한 결합조직형성 소원형세포종양의 증례 보고1
Case Report pISSN 1738-2637 / eISSN 2288-2928 J Korean Soc Radiol 2015;72(4):295-299 http://dx.doi.org/10.3348/jksr.2015.72.4.295 Bilateral Presentation of Pleural Desmoplastic Small Round Cell Tumors: A Case Report1 양측 흉막에 발생한 결합조직형성 소원형세포종양의 증례 보고1 You Sun Won, MD1, Jai Soung Park, MD1, Sun Hye Jeong, MD1, Sang Hyun Paik, MD1, Heon Lee, MD1, Jang Gyu Cha, MD1, Eun Suk Koh, MD2 Departments of 1Radiology, 2Pathology, Soonchunhyang University College of Medicine, Bucheon Hospital, Bucheon, Korea Desmoplastic small round cell tumor (DSRCT) is a highly aggressive malignant small cell neoplasm occurring mainly in the abdominal cavity, but it is extremely rare in Received October 13, 2014; Accepted December 21, the pleura. In this case, a 15-year-old male presented with a 1-month history of left 2014 chest pain. Chest radiographs revealed pleural thickening in the left hemithorax and Corresponding author: Jai Soung Park, MD Department of Radiology, Soonchunhyang University chest computed tomography showed multifocal pleural thickening with enhance- College of Medicine, Bucheon Hospital, 170 Jomaru-ro, ment in both hemithoraces. A needle biopsy of the left pleural lesion was performed Wonmi-gu, Bucheon 420-767, Korea. and the final diagnosis was DSRCT of the pleura. We report this unusual case aris- Tel. 82-32-621-5851 Fax. 82-32-621-5874 E-mail: [email protected] ing from the pleura bilaterally. The pleural involvement of this tumor supports the hypothesis that it typically occurs in mesothelial-lined surfaces. This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) Index terms which permits unrestricted non-commercial use, distri- Pleura bution, and reproduction in any medium, provided the Thickened Pleura original work is properly cited. -

Nodular Fasciitis of the Pectoralis Muscle in a 54-Year-Old Woman
ACS Case Reviews in Surgery Vol. 2, No. 3 Nodular Fasciitis of the Pectoralis Muscle in a 54-Year-Old Woman AUTHORS: CORRESPONDENCE AUTHOR: AUTHOR AFFILIATIONS: Christopher D. Kannera; Divya Sharma, MDb; Dr. Jaime D Lewis a. Medical Student, University of Cincinnati College Jaime D Lewis, MD, FACSc UC Health Women’s Center of Medicine, Cincinnati, Ohio 7675 Wellness Way b. Department of Pathology and Laboratory West Chester, Ohio 45069 Medicine, University of Cincinnati College of Phone: (513) 584-8900 Medicine, Cincinnati, Ohio Email: [email protected] c. Department of Surgery, University of Cincinnati College of Medicine, Cincinnati, Ohio Background A 54-year-old woman presented with a breast mass found to be nodular fasciitis of the right pectoralis muscle. Summary A 54-year-old woman presented to a breast surgeon for evaluation of a painful right breast mass. Initial mammography was unrevealing. Ultrasound revealed a right pectoral mass extending into the soft tissue of the breast. Core needle biopsy specimen revealed features suggestive of low grade sarcoma. Findings on computed tomography (CT) and magnetic resonance imaging (MRI) were nonspecific and wide local excision was subsequently performed. Pathologic characteristics were consistent with nodular fasciitis. This benign proliferation of fibroblasts and myofibroblasts frequently raises concern for malignant neoplasms due to its rapid, infiltrative growth, and nonspecific imaging characteristics. Thus, it is often identified by its characteristic features on surgical pathology following excision. On rare occasions when it is managed with surveillance, nodular fasciitis frequently demonstrates spontaneous regression. Conclusion Nodular fasciitis is a benign growth with a tendency for spontaneous regression, which exhibits clinical features that often invoke suspicion of malignancy. -

Soft Tissue Cytopathology: a Practical Approach Liron Pantanowitz, MD
4/1/2020 Soft Tissue Cytopathology: A Practical Approach Liron Pantanowitz, MD Department of Pathology University of Pittsburgh Medical Center [email protected] What does the clinician want to know? • Is the lesion of mesenchymal origin or not? • Is it begin or malignant? • If it is malignant: – Is it a small round cell tumor & if so what type? – Is this soft tissue neoplasm of low or high‐grade? Practical diagnostic categories used in soft tissue cytopathology 1 4/1/2020 Practical approach to interpret FNA of soft tissue lesions involves: 1. Predominant cell type present 2. Background pattern recognition Cell Type Stroma • Lipomatous • Myxoid • Spindle cells • Other • Giant cells • Round cells • Epithelioid • Pleomorphic Lipomatous Spindle cell Small round cell Fibrolipoma Leiomyosarcoma Ewing sarcoma Myxoid Epithelioid Pleomorphic Myxoid sarcoma Clear cell sarcoma Pleomorphic sarcoma 2 4/1/2020 CASE #1 • 45yr Man • Thigh mass (fatty) • CNB with TP (DQ stain) DQ Mag 20x ALT –Floret cells 3 4/1/2020 Adipocytic Lesions • Lipoma ‐ most common soft tissue neoplasm • Liposarcoma ‐ most common adult soft tissue sarcoma • Benign features: – Large, univacuolated adipocytes of uniform size – Small, bland nuclei without atypia • Malignant features: – Lipoblasts, pleomorphic giant cells or round cells – Vascular myxoid stroma • Pitfalls: Lipophages & pseudo‐lipoblasts • Fat easily destroyed (oil globules) & lost with preparation Lipoma & Variants . Angiolipoma (prominent vessels) . Myolipoma (smooth muscle) . Angiomyolipoma (vessels + smooth muscle) . Myelolipoma (hematopoietic elements) . Chondroid lipoma (chondromyxoid matrix) . Spindle cell lipoma (CD34+ spindle cells) . Pleomorphic lipoma . Intramuscular lipoma Lipoma 4 4/1/2020 Angiolipoma Myelolipoma Lipoblasts • Typically multivacuolated • Can be monovacuolated • Hyperchromatic nuclei • Irregular (scalloped) nuclei • Nucleoli not typically seen 5 4/1/2020 WD liposarcoma Layfield et al. -

The Health-Related Quality of Life of Sarcoma Patients and Survivors In
Cancers 2020, 12 S1 of S7 Supplementary Materials The Health-Related Quality of Life of Sarcoma Patients and Survivors in Germany—Cross-Sectional Results of A Nationwide Observational Study (PROSa) Martin Eichler, Leopold Hentschel, Stephan Richter, Peter Hohenberger, Bernd Kasper, Dimosthenis Andreou, Daniel Pink, Jens Jakob, Susanne Singer, Robert Grützmann, Stephen Fung, Eva Wardelmann, Karin Arndt, Vitali Heidt, Christine Hofbauer, Marius Fried, Verena I. Gaidzik, Karl Verpoort, Marit Ahrens, Jürgen Weitz, Klaus-Dieter Schaser, Martin Bornhäuser, Jochen Schmitt, Markus K. Schuler and the PROSa study group Includes Entities We included sarcomas according to the following WHO classification. - Fletcher CDM, World Health Organization, International Agency for Research on Cancer, editors. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013. 468 p. (World Health Organization classification of tumours). - Kurman RJ, International Agency for Research on Cancer, World Health Organization, editors. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: International Agency for Research on Cancer; 2014. 307 p. (World Health Organization classification of tumours). - Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur Urol. 2016 Jul;70(1):106–19. - World Health Organization, Swerdlow SH, International Agency for Research on Cancer, editors. WHO classification of tumours of haematopoietic and lymphoid tissues: [... reflects the views of a working group that convened for an Editorial and Consensus Conference at the International Agency for Research on Cancer (IARC), Lyon, October 25 - 27, 2007]. 4. ed. -

A Comparison of Imaging Modalities for the Diagnosis of Osteomyelitis
A comparison of imaging modalities for the diagnosis of osteomyelitis Brandon J. Smith1, Grant S. Buchanan2, Franklin D. Shuler2 Author Affiliations: 1. Joan C Edwards School of Medicine, Marshall University, Huntington, West Virginia 2. Marshall University The authors have no financial disclosures to declare and no conflicts of interest to report. Corresponding Author: Brandon J. Smith Marshall University Joan C. Edwards School of Medicine Huntington, West Virginia Email: [email protected] Abstract Osteomyelitis is an increasingly common pathology that often poses a diagnostic challenge to clinicians. Accurate and timely diagnosis is critical to preventing complications that can result in the loss of life or limb. In addition to history, physical exam, and laboratory studies, diagnostic imaging plays an essential role in the diagnostic process. This narrative review article discusses various imaging modalities employed to diagnose osteomyelitis: plain films, computed tomography (CT), magnetic resonance imaging (MRI), ultrasound, bone scintigraphy, and positron emission tomography (PET). Articles were obtained from PubMed and screened for relevance to the topic of diagnostic imaging for osteomyelitis. The authors conclude that plain films are an appropriate first step, as they may reveal osteolytic changes and can help rule out alternative pathology. MRI is often the most appropriate second study, as it is highly sensitive and can detect bone marrow changes within days of an infection. Other studies such as CT, ultrasound, and bone scintigraphy may be useful in patients who cannot undergo MRI. CT is useful for identifying necrotic bone in chronic infections. Ultrasound may be useful in children or those with sickle-cell disease. Bone scintigraphy is particularly useful for vertebral osteomyelitis. -
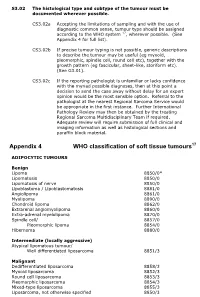
Appendix 4 WHO Classification of Soft Tissue Tumours17
S3.02 The histological type and subtype of the tumour must be documented wherever possible. CS3.02a Accepting the limitations of sampling and with the use of diagnostic common sense, tumour type should be assigned according to the WHO system 17, wherever possible. (See Appendix 4 for full list). CS3.02b If precise tumour typing is not possible, generic descriptions to describe the tumour may be useful (eg myxoid, pleomorphic, spindle cell, round cell etc), together with the growth pattern (eg fascicular, sheet-like, storiform etc). (See G3.01). CS3.02c If the reporting pathologist is unfamiliar or lacks confidence with the myriad possible diagnoses, then at this point a decision to send the case away without delay for an expert opinion would be the most sensible option. Referral to the pathologist at the nearest Regional Sarcoma Service would be appropriate in the first instance. Further International Pathology Review may then be obtained by the treating Regional Sarcoma Multidisciplinary Team if required. Adequate review will require submission of full clinical and imaging information as well as histological sections and paraffin block material. Appendix 4 WHO classification of soft tissue tumours17 ADIPOCYTIC TUMOURS Benign Lipoma 8850/0* Lipomatosis 8850/0 Lipomatosis of nerve 8850/0 Lipoblastoma / Lipoblastomatosis 8881/0 Angiolipoma 8861/0 Myolipoma 8890/0 Chondroid lipoma 8862/0 Extrarenal angiomyolipoma 8860/0 Extra-adrenal myelolipoma 8870/0 Spindle cell/ 8857/0 Pleomorphic lipoma 8854/0 Hibernoma 8880/0 Intermediate (locally -

Soft Tissue Tumor Pathology: New Diagnostic Immunohistochemical Markers Leona A
S EMINARS IN D IAGNOSTIC P ATHOLOGY ] (2015) ]]]– ]]] Available online at www.sciencedirect.com www.elsevier.com/locate/semdp Soft tissue tumor pathology: New diagnostic immunohistochemical markers Leona A. Doyle, MD Department of Pathology, Brigham and Women's Hospital and Harvard Medical School, 75 Francis St, Boston, Massachusetts article info abstract Keywords: Recent insights into the pathogenesis of various soft tissue tumors, along with the Soft tissue identification of recurrent molecular alterations characteristic of specific tumor types, Tumor have resulted in the development of many diagnostically useful immunohistochemical Sarcoma markers. In some cases, expression of these markers is significantly associated with Immunohistochemistry distinctive clinical and histologic features, which may impart prognostic or predictive Molecular genetics information. This review outlines new diagnostic immunohistochemical markers in soft tissue tumor pathology, emphasizing their utility in clinical practice and potential pitfalls, molecular correlates and clinical associations. & 2015 Elsevier Inc. All rights reserved. Introduction shows MYC amplification. Finally, so-called lineage specific markers, which tend to show nuclear staining and in general fi Over the last 10 years, many novel immunohistochemical are not strictly speci c to a given lineage, have also emerged markers for use in the evaluation of soft tissue tumors have as useful markers, not only in soft tissue pathology but also been described. This has largely been due to new insights -

The Best Diagnosis Is
Dermatopathology Diagnosis Superficial Plantar Fibromatosis The best diagnosis is: H&E, original magnification 40. a. dermatofibroma b. keloid CUTISc. neurofibroma d. nodular fasciitis Do Note. superficialCopy plantar fibromatosis H&E, original magnification 400. PLEASE TURN TO PAGE 225 FOR DERMATOPATHOLOGY DIAGNOSIS DISCUSSION Luke Lennox, BA; Anna Li, BS; Thomas N. Helm, MD Mr. Lennox and Dr. Helm are from the Department of Dermatology, University at Buffalo, The State University of New York. Ms. Li is from the Department of Dermatology, Ross University, Dominica, West Indies. The authors report no conflict of interest. Correspondence: Thomas N. Helm, MD, Dermatopathology Laboratory, 6255 Sheridan Dr, Building B, Ste 208, Williamsville, NY 14221 ([email protected]). 220 CUTIS® WWW.CUTIS.COM Copyright Cutis 2013. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. Dermatopathology Diagnosis Discussion Superficial Plantar Fibromatosis lantar fibromatosis typically presents as firm represents a reactive proliferation of spindle cells most plaques or nodules on the plantar surface of the often encountered on the extremities of young adults. Pfoot.1 The process is caused by a proliferation of Spindle cells are loosely arranged in a mucinous fibroblasts and collagen and has been associated with stroma and are not circumscribed (tissue culture ap- trauma, liver disease, diabetes mellitus, epilepsy, and pearance). Vesicular nuclei are encountered, but there alcoholism.2 Unlike the fibromatoses associated with is no remarkable nuclear pleomorphism. Extravasated Gardner syndrome, superficial plantar fibromatosis has not been associated with abnormalities in the ade- nomatous polyposis coli gene or with the -catenin gene.3,4 Lesions typically present in middle-aged or elderly individuals and involve the medial plantar fas- cia. -

Bone & Soft Tissue Pathology Fellowship
Bone & Soft Tissue Pathology Fellowship The Department of Pathology at Memorial Availability: July 2023 Sloan Kettering Cancer Center offers a one- year fellowship training program in bone and Number of Positions: One soft tissue pathology. The fellowship begins on Length of Program: One Year July 1st and ends on June 30th the following year. All fellows should have completed Deadline: August 1, for appoint- residency training in anatomic pathology and ments beginning 2 years later (ie. be certified (or eligible for certification) by 8/1/2021 for start date 7/1/2023). the American Board of Pathology. Early application is acceptable because completed applications may be During the sub-specialty fellowship year, the considered on a rolling basis. fellow will have the opportunity to study our large volume of quality in-house and submitted How to Apply: Apply Online material, departmental consultation case Only complete applications will material, as well as recommended reading of be reviewed. Once applicants have literature to achieve adequate competence submitted their applications, they will in the pathologic diagnosis, staging, and need to send the following documents: prognostication of a wide variety of bone and • Three letters of recommendation from soft tissue tumors. In addition, the fellow an institution in which the applicant will have the opportunity to perform clinico- has trained. Letters should be pathologic and molecular correlations. addressed to Dr. Ronald Ghossein, the The fellow will serve as a consultant to the program director. Please request letter oncologic pathology fellows in the orientation, writers add the following line after gross dissection and morphologic evaluation the heading (RE: Candidate’s Name, of bone and soft tissue specimens. -

About Soft Tissue Sarcoma Overview and Types
cancer.org | 1.800.227.2345 About Soft Tissue Sarcoma Overview and Types If you've been diagnosed with soft tissue sarcoma or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Soft Tissue Sarcoma? Research and Statistics See the latest estimates for new cases of soft tissue sarcoma and deaths in the US and what research is currently being done. ● Key Statistics for Soft Tissue Sarcomas ● What's New in Soft Tissue Sarcoma Research? What Is a Soft Tissue Sarcoma? Cancer starts when cells start to grow out of control. Cells in nearly any part of the body can become cancer and can spread to other areas. To learn more about how cancers start and spread, see What Is Cancer?1 There are many types of soft tissue tumors, and not all of them are cancerous. Many benign tumors are found in soft tissues. The word benign means they're not cancer. These tumors can't spread to other parts of the body. Some soft tissue tumors behave 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 in ways between a cancer and a non-cancer. These are called intermediate soft tissue tumors. When the word sarcoma is part of the name of a disease, it means the tumor is malignant (cancer).A sarcoma is a type of cancer that starts in tissues like bone or muscle. Bone and soft tissue sarcomas are the main types of sarcoma. Soft tissue sarcomas can develop in soft tissues like fat, muscle, nerves, fibrous tissues, blood vessels, or deep skin tissues. -
The Role of Cytogenetics and Molecular Diagnostics in the Diagnosis of Soft-Tissue Tumors Julia a Bridge
Modern Pathology (2014) 27, S80–S97 S80 & 2014 USCAP, Inc All rights reserved 0893-3952/14 $32.00 The role of cytogenetics and molecular diagnostics in the diagnosis of soft-tissue tumors Julia A Bridge Department of Pathology and Microbiology, University of Nebraska Medical Center, Omaha, NE, USA Soft-tissue sarcomas are rare, comprising o1% of all cancer diagnoses. Yet the diversity of histological subtypes is impressive with 4100 benign and malignant soft-tissue tumor entities defined. Not infrequently, these neoplasms exhibit overlapping clinicopathologic features posing significant challenges in rendering a definitive diagnosis and optimal therapy. Advances in cytogenetic and molecular science have led to the discovery of genetic events in soft- tissue tumors that have not only enriched our understanding of the underlying biology of these neoplasms but have also proven to be powerful diagnostic adjuncts and/or indicators of molecular targeted therapy. In particular, many soft-tissue tumors are characterized by recurrent chromosomal rearrangements that produce specific gene fusions. For pathologists, identification of these fusions as well as other characteristic mutational alterations aids in precise subclassification. This review will address known recurrent or tumor-specific genetic events in soft-tissue tumors and discuss the molecular approaches commonly used in clinical practice to identify them. Emphasis is placed on the role of molecular pathology in the management of soft-tissue tumors. Familiarity with these genetic events -
Pathology and Genetics of Tumours of Soft Tissue and Bone
bb5_1.qxd 13.9.2006 14:05 Page 3 World Health Organization Classification of Tumours WHO OMS International Agency for Research on Cancer (IARC) Pathology and Genetics of Tumours of Soft Tissue and Bone Edited by Christopher D.M. Fletcher K. Krishnan Unni Fredrik Mertens IARCPress Lyon, 2002 bb5_1.qxd 13.9.2006 14:05 Page 4 World Health Organization Classification of Tumours Series Editors Paul Kleihues, M.D. Leslie H. Sobin, M.D. Pathology and Genetics of Tumours of Soft Tissue and Bone Editors Christopher D.M. Fletcher, M.D. K. Krishnan Unni, M.D. Fredrik Mertens, M.D. Coordinating Editor Wojciech Biernat, M.D. Layout Lauren A. Hunter Illustrations Lauren A. Hunter Georges Mollon Printed by LIPS 69009 Lyon, France Publisher IARCPress International Agency for Research on Cancer (IARC) 69008 Lyon, France bb5_1.qxd 13.9.2006 14:05 Page 5 This volume was produced in collaboration with the International Academy of Pathology (IAP) The WHO Classification of Tumours of Soft Tissue and Bone presented in this book reflects the views of a Working Group that convened for an Editorial and Consensus Conference in Lyon, France, April 24-28, 2002. Members of the Working Group are indicated in the List of Contributors on page 369. bb5_1.qxd 22.9.2006 9:03 Page 6 Published by IARC Press, International Agency for Research on Cancer, 150 cours Albert Thomas, F-69008 Lyon, France © International Agency for Research on Cancer, 2002, reprinted 2006 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention.