For Their Own Good
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Appendix 5 Fylde
FYLDE DISTRICT - APPENDIX 5 SUBSIDISED LOCAL BUS SERVICE EVENING AND SUNDAY JOURNEYS PROPOSED TO BE WITHDRAWN FROM 18 MAY 2014 LANCASTER - GARSTANG - POULTON - BLACKPOOL 42 via Galgate - Great Eccleston MONDAY TO SATURDAY Service Number 42 42 42 $ $ $ LANCASTER Bus Station 1900 2015 2130 SCOTFORTH Boot and Shoe 1909 2024 2139 LANCASTER University Gates 1912 2027 2142 GALGATE Crossroads 1915 2030 2145 CABUS Hamilton Arms 1921 2036 2151 GARSTANG Bridge Street 1926 2041 2156 CHURCHTOWN Horns Inn 1935 2050 2205 ST MICHAELS Grapes Hotel 1939 2054 2209 GREAT ECCLESTON Square 1943 2058 2213 POULTON St Chads Church 1953 2108 2223 BLACKPOOL Layton Square 1958 2113 2228 BLACKPOOL Abingdon Street 2010 2125 2240 $ - Operated on behalf of Lancashire County Council BLACKPOOL - POULTON - GARSTANG - LANCASTER 42 via Great Eccleston - Galgate MONDAY TO SATURDAY Service Number 42 42 42 $ $ $ BLACKPOOL Abingdon Street 2015 2130 2245 BLACKPOOL Layton Square 2020 2135 2250 POULTON Teanlowe Centre 2032 2147 2302 GREAT ECCLESTON Square 2042 2157 2312 ST MICHAELS Grapes Hotel 2047 2202 2317 CHURCHTOWN Horns Inn 2051 2206 2321 GARSTANG Park Hill Road 2059 2214 2329 CABUS Hamilton Arms 2106 2221 2336 GALGATE Crossroads 2112 2227 2342 LANCASTER University Gates 2115 2230 2345 SCOTFORTH Boot and Shoe 2118 2233 2348 LANCASTER Bus Station 2127 2242 2357 $ - Operated on behalf of Lancashire County Council LIST OF ALTERNATIVE TRANSPORT SERVICES AVAILABLE – Stagecoach in Lancaster Service 2 between Lancaster and University Stagecoach in Lancaster Service 40 between Lancaster and Garstang (limited) Blackpool Transport Service 2 between Poulton and Blackpool FYLDE DISTRICT - APPENDIX 5 SUBSIDISED LOCAL BUS SERVICE EVENING AND SUNDAY JOURNEYS PROPOSED TO BE WITHDRAWN FROM 18 MAY 2014 PRESTON - LYTHAM - ST. -

Lancaster Archaeological and Historical Society Research Group Newsletter
Lancaster Archaeological and Multum in parvo Historical Society http://lahs.archaeologyuk.org/ Research Group Newsletter orem ipsum dolor sit amet, consectetuer adipisci No. 2: August 2020 Welcome to the Research Group e-newsletter We received encouraging feedback from Society amount of research now being conducted online, members following the first issue of the e-newsletter news that the National Archives are allowing people in May 2020 which was much appreciated. The e- to download their digital resources free during the newsletter is open to all Society members and guest pandemic has been very welcome. If you have a authors should they be interested in publishing a brief Lancashire County Library ticket it is possible to letter, or a short article of 500-750 words on an access information online such as the Oxford archaeological or historical subject related to Dictionary of National Biography and several local Lancaster and surrounding areas. Longer articles are papers from the nineteenth century (with thanks to Dr published in Contrebis Michael Winstanley). As lockdown restrictions begin to ease, do not delay in taking advantage when The last five months have been a difficult time for research facilities re-open because with social researchers with the Covid-19 lockdown making distancing measures still in force, there are likely to face-to-face meetings impossible; archive, museum be appointment systems or time-limited visits and library services closed, and employees in many introduced. organisations working from home. Research can be a lonely occupation at the best of times so the surge in If you would like to join the Research Group or online virtual meetings has offered some welcome contribute to the e-newsletter, contact details are relief from social isolation. -

2005 No. 170 LOCAL GOVERNMENT, ENGLAND The
STATUTORY INSTRUMENTS 2005 No. 170 LOCAL GOVERNMENT, ENGLAND The County of Lancashire (Electoral Changes) Order 2005 Made - - - - 1st February 2005 Coming into force in accordance with article 1(2) Whereas the Boundary Committee for England(a), acting pursuant to section 15(4) of the Local Government Act 1992(b), has submitted to the Electoral Commission(c) recommendations dated October 2004 on its review of the county of Lancashire: And whereas the Electoral Commission have decided to give effect, with modifications, to those recommendations: And whereas a period of not less than six weeks has expired since the receipt of those recommendations: Now, therefore, the Electoral Commission, in exercise of the powers conferred on them by sections 17(d) and 26(e) of the Local Government Act 1992, and of all other powers enabling them in that behalf, hereby make the following Order: Citation and commencement 1.—(1) This Order may be cited as the County of Lancashire (Electoral Changes) Order 2005. (2) This Order shall come into force – (a) for the purpose of proceedings preliminary or relating to any election to be held on the ordinary day of election of councillors in 2005, on the day after that on which it is made; (b) for all other purposes, on the ordinary day of election of councillors in 2005. Interpretation 2. In this Order – (a) The Boundary Committee for England is a committee of the Electoral Commission, established by the Electoral Commission in accordance with section 14 of the Political Parties, Elections and Referendums Act 2000 (c.41). The Local Government Commission for England (Transfer of Functions) Order 2001 (S.I. -
Initial Template Document
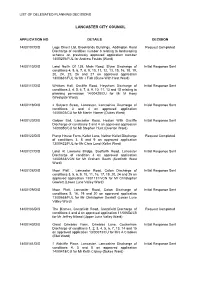
LIST OF DELEGATED PLANNING DECISIONS LANCASTER CITY COUNCIL APPLICATION NO DETAILS DECISION 14/00107/DIS Logs Direct Ltd, Brooklands Buildings, Addington Road Request Completed Discharge of condition number 6 relating to landscaping scheme on previously approved application number 14/00276/FUL for Andrew Foulds (Ward) 14/00110/DIS Land North Of 138, Main Road, Slyne Discharge of Initial Response Sent conditions 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 15, 16, 18, 19, 20, 24, 25, 26 and 27 on approved application 13/00831/FUL for Mr J Fish (Slyne With Hest Ward) 14/00117/DIS Whittam Hall, Oxcliffe Road, Heysham Discharge of Initial Response Sent conditions 3, 4, 5, 6, 7, 8, 9, 10, 11, 13 and 15 relating to planning permission 14/00428/CU for Mr M Hoey (Westgate Ward) 14/00119/DIS 2 Sulyard Street, Lancaster, Lancashire Discharge of Initial Response Sent conditions 3 and 4 on approved application 14/00403/CU for Mr Martin Horner (Dukes Ward) 14/00120/DIS Golden Ball, Lancaster Road, Heaton With Oxcliffe Initial Response Sent Discharge of conditions 3 and 4 on approved application 14/00050/CU for Mr Stephen Hunt (Overton Ward) 14/00122/DIS Pump House Farm, Kellet Lane, Nether Kellet Discharge Request Completed of conditions 3, 8 and 9 on approved application 13/00422/FUL for Mr Chris Lund (Kellet Ward) 14/00127/DIS Land At Lawsons Bridge, Scotforth Road, Lancaster Initial Response Sent Discharge of condition 4 on approved application 14/00633/VCN for Mr Graham Booth (Scotforth West Ward) 14/00128/DIS Moor Platt , Lancaster Road, Caton Discharge -

Der Europäischen Gemeinschaften Nr
26 . 3 . 84 Amtsblatt der Europäischen Gemeinschaften Nr . L 82 / 67 RICHTLINIE DES RATES vom 28 . Februar 1984 betreffend das Gemeinschaftsverzeichnis der benachteiligten landwirtschaftlichen Gebiete im Sinne der Richtlinie 75 /268 / EWG ( Vereinigtes Königreich ) ( 84 / 169 / EWG ) DER RAT DER EUROPAISCHEN GEMEINSCHAFTEN — Folgende Indexzahlen über schwach ertragsfähige Böden gemäß Artikel 3 Absatz 4 Buchstabe a ) der Richtlinie 75 / 268 / EWG wurden bei der Bestimmung gestützt auf den Vertrag zur Gründung der Euro jeder der betreffenden Zonen zugrunde gelegt : über päischen Wirtschaftsgemeinschaft , 70 % liegender Anteil des Grünlandes an der landwirt schaftlichen Nutzfläche , Besatzdichte unter 1 Groß vieheinheit ( GVE ) je Hektar Futterfläche und nicht über gestützt auf die Richtlinie 75 / 268 / EWG des Rates vom 65 % des nationalen Durchschnitts liegende Pachten . 28 . April 1975 über die Landwirtschaft in Berggebieten und in bestimmten benachteiligten Gebieten ( J ), zuletzt geändert durch die Richtlinie 82 / 786 / EWG ( 2 ), insbe Die deutlich hinter dem Durchschnitt zurückbleibenden sondere auf Artikel 2 Absatz 2 , Wirtschaftsergebnisse der Betriebe im Sinne von Arti kel 3 Absatz 4 Buchstabe b ) der Richtlinie 75 / 268 / EWG wurden durch die Tatsache belegt , daß das auf Vorschlag der Kommission , Arbeitseinkommen 80 % des nationalen Durchschnitts nicht übersteigt . nach Stellungnahme des Europäischen Parlaments ( 3 ), Zur Feststellung der in Artikel 3 Absatz 4 Buchstabe c ) der Richtlinie 75 / 268 / EWG genannten geringen Bevöl in Erwägung nachstehender Gründe : kerungsdichte wurde die Tatsache zugrunde gelegt, daß die Bevölkerungsdichte unter Ausschluß der Bevölke In der Richtlinie 75 / 276 / EWG ( 4 ) werden die Gebiete rung von Städten und Industriegebieten nicht über 55 Einwohner je qkm liegt ; die entsprechenden Durch des Vereinigten Königreichs bezeichnet , die in dem schnittszahlen für das Vereinigte Königreich und die Gemeinschaftsverzeichnis der benachteiligten Gebiete Gemeinschaft liegen bei 229 beziehungsweise 163 . -

The First 40 Years
A HISTORY OF LANCASTER CIVIC SOCIETY THE FIRST 40 YEARS 1967 – 2007 By Malcolm B Taylor 2009 Serialization – part 7 Territorial Boundaries This may seem a superfluous title for an eponymous society, so a few words of explanation are thought necessary. The Society’s sometime reluctance to expand its interests beyond the city boundary has not prevented a more elastic approach when the situation demands it. Indeed it is not true that the Society has never been prepared to look beyond the City boundary. As early as 1971 the committee expressed a wish that the Society might be a pivotal player in the formation of amenity bodies in the surrounding districts. It was resolved to ask Sir Frank Pearson to address the Society on the issue, although there is no record that he did so. When the Society was formed, and, even before that for its predecessor, there would have been no reason to doubt that the then City boundary would also be the Society’s boundary. It was to be an urban society with urban values about an urban environment. However, such an obvious logic cannot entirely define the part of the city which over the years has dominated the Society’s attentions. This, in simple terms might be described as the city’s historic centre – comprising largely the present Conservation Areas. But the boundaries of this area must be more fluid than a simple local government boundary or the Civic Amenities Act. We may perhaps start to come to terms with definitions by mentioning some buildings of great importance to Lancaster both visually and strategically which have largely escaped the Society’s attentions. -

St. Paul's Church, Scotforth
St. Paul’s Church, Scotforth Contents Summary 2 Our Vision 3 Who Is God Calling? 3 The Parish and Wider Community 4 Church Organization 7 The Church Community 8 Together we are stronger 10 Our Buildings 11 The Church 12 The Hala Centre 13 The Parish Hall 14 The Vicarage 15 The Church Finances 16 Our Schools 17 Our Links into the Wider Community 20 1 Summary St Paul’s Church Scotforth is a vibrant and accepting community in Lancaster. The church building is a landmark on the A6 south of the city centre, and the vicarage is adjacent in its own private grounds. Living here has many attractive features. We have our own outstanding C of E primary school nearby with which we have strong links. And very close to the parish we also find outstanding secondary schools, Ripley C of E academy and two top-rated grammar schools. In addition Lancaster’s two universities bring lively people and facilities to the area. Traveling to and from Scotforth has many possibilities. We rapidly connect to the M6 and to the west coast main train line. Our proximity to beautiful countryside keeps many residents happy to remain. We are close to the Lake District, the Yorkshire Dales, Bowland forest, Morecambe Bay, to mention just a few such attractions. Our Church is a welcoming and friendly place. Our central churchmanship is consistent with the lack of a central aisle in our unusual “pot” church building! Our regular services (BCP or traditional, in church or in the Hala Centre) use the Bible lectionary to encourage understanding and action, but we also are keen to develop innovative forms of worship. -

History of the Manchester Ship Canal, from Its Inception to Its Completion
HISTORY OF THE MANCHESTER SHIP CANAL SIR BOSDIN LEECH to of tbe of Toronto lo. C . -CT : HISTORY OF THE MANCHESTER SHIP CANAL " Floreat Semper Mancunium DANIEL ADAMSON, FIRST CHAIRMAN OF THE MANCHESTER SHIP CANAL COMPANY. Elliott & Fry. Frontispiece. HISTORY OF THE MANCHESTER SHIP CANAL FROM ITS INCEPTION TO ITS COMPLETION WITH PERSONAL REMINISCENCES BY SIR BOSDIN LEECH NUMEROUS PLANS, PORTRAITS AND ILLUSTRATIONS IN TWO VOLUMES VOL I. 1*1 a s MANCHESTER AND LONDON: SHERRATT & HUGHES 1907 THE ABERDEEN UNIVERSITY PRESS LIMITED THESE VOLUMES ARE DEDICATED TO THE LORD MAYOR AND CORPORATION OF THE CITY OF MANCHESTER IN COMMEMORATION OF THE PUBLIC SPIRIT DISPLAYED BY THAT CITY IN COMING TO THE ASSISTANCE OF THE MANCHESTER SHIP CANAL AT A CRITICAL STATE OF ITS AFFAIRS, AND IN THE HOPE THAT THEIR EXAMPLE MAY STIMULATE FUTURE GENERATIONS TO SIMILAR LOCAL PATRIOTISM PREFACE. early struggles and ultimate triumph of the Manchester Ship Canal consti- THEtute a subject of absorbing interest. In the history of Manchester, and indeed of South Lancashire as a whole, no other event or enterprise can compare with it in its far-reaching effects. The story, too, in many respects contains all the elements of a romance. It is the relation of a desperate and almost hopeless fight against opposi- tion of the most powerful and uncompromising character, and it is meet that the names and qualities of the men engaged in the strife, and the nature of the difficulties which they encountered and overcame, should find a permanent record. To rescue both individuals and incidents from oblivion, and to give a connected narrative of the course of events from the conception to the completion of the canal, is the object of the present work. -
X FINAL ISLANDS of BARROW MAP PHOTO SIDE COLOURWAY 2 Copy
Prehistoric Islands An Industrial Revolution Barrow Airships Key Dates Prehistoric nds inc. axe heads have been discovered around the Islands of The expansion of Barrow-in-Furness was due to three men: Lord Cavendish, 7th 1911 Britains rst rigid airship HMA 1 ‘Mayy’, built in Barrow’s Cavendish 1127 Furness Abbey is established; The First Savignac Monastery in England The Islands of Barrow Barrow, many on Walney Island and Sandscale Haws. The coast oered stone age Duke of Devonshire (the nancier), Henry Schneider (local iron ore magnate) & Dock. 1134-1342 Furness Abbey becomes 2nd most powerful Cistercian Abbey in England communities, a wide range of foods and materials, often gathered during the James Ramsden (managing director of the Furness Railway Company). 1487 Lambert Simnal Lands on Piel Island & Claims English Throne hard winter months. It also oered opportunities for trade & communication via HMA 1 Mayy (named as such because “she may y” famously broke in two 1839 Henry Schneider a speculator & dealer in iron arrives during a test ight over Cavendish Dock but important lessons were learnt. sea-borne trac. Indeed, for much of prehistory, the sea was a link to the wider Ramsden built a ne house (now demolished) in Abbots wood above Furness Abbey. 1843 Only 32 dwellings & two pubs in the Hamlet of Barrow Later designs for rigid & non rigid airships were built by H.B. Pratt & Barnes world, rather than a barrier to it. Perhaps it is no surprise that the earliest cereal Some of Ramsden’s possessions & furniture were given to the Town Hall. Ramsden’s 1846 Furness Railway built by Schneider & James Ramsden to transport iron ore & slate Pictorial Wallis for the Vickers Airship Dept. -

Tootal Recall Tscarves and Pocket Squares Inspired Once Championed by Raffish Mods in the 1960S, by Its Own Impeccably Stylish Herit- Age—Underwent a ‘Quiet Relaunch’
HREE years ago, a vene- rable British company called Tootal—its stock in trade vintage-look men’s Tootal recall Tscarves and pocket squares inspired Once championed by raffish Mods in the 1960s, by its own impeccably stylish herit- age—underwent a ‘quiet relaunch’. Tootal’s paisley-print and polka-dot scarves are making Throughout the second quarter of the last century, Tootal sold quantities quite a comeback, reports Matthew Dennison of such scarves, alongside Tootal ties, which it promoted vigorously with the advertising slogan ‘Every Man Needs… Tootal Ties’. At a time when tie-wearing is in decline, and increasingly informal men’s dress nullifies Tootal’s one- time claim that it produced a tie ‘to suit every occasion from a board meeting to a boxing match’ and ‘every activity from banking to bird watching’, the current renaissance of the Tootal scarf and the company’s fortunes is partly attributable to cele- brity endorsement. Musicians such as Liam Gallagher and Paul Weller have been photographed wearing Tootal scarves as has actor Benedict Cumberbatch. Tootal itself claims that its ties and scarves, manufactured at affordable prices—and, in the case of Tootal ties, in washable, uncreasable fabrics, often striped or with small-scale geometric patterns—had a particu- lar appeal for working-class shoppers. Today, Tootal’s polka-dot and pais- ley-print scarves in traditionally masculine colours are made from fringed silk and aim at a classless Benedict Since 1991, the Tootal brand has as ‘Tootal Cloth’ and striped men’s demographic. They Cumberbatch formed part of Coats Viyella. -

Download Tootal Sustainable Collection Book
Tootal goes sustainable Introduction Tootal Fabrics (Holland) B.V. as one of the leading European suppliers of shirt & blouse fabrics has expanded its sustainable fabric collection and will continue doing so! We believe that this is a necessary step to contribute to a more sustainable approach in the textile industry and to increase the awareness of customers and consumers about ecological influences. Reducing microfibers which are polluting the world’s oceans and using materials with less environmental impact: sustainability should be front and centre in the textile- and apparel industry! Our approach The production and manufacturing of textile is a water and chemical intensive process, which has a negative impact on our planet. The world turns a blind eye towards the textile industry being one of the biggest polluters. Tootal Fabrics (Holland) B.V. takes responsibility by offering a sustainable fabric collection and helps reducing this impact. We made first steps towards sustainability years ago already by certifying our entire fabric collection by Oekotex Standards and covering the European Union REACH regulation, which is adopted to improve the protection to human health and the environment that can be posed by chemicals. We are certified by and comply with the worldwide recognized standards such as: GOTS, GRS, OCS and BCI. Our whole supply chain is monitored by these organisations to ensure that highest standards are kept year after year by Tootal Fabrics (Holland) B.V.. At present we offer sustainable fabrics with organic cotton and recycled polyester as well as eco-friendly fabrics such as Tencel ®, viscose, linen and bamboo as part of our standard collection. -

Friday Remnant Savincs
Girls' Dance Dresses Beach sl'95 Boys' Robes, ^ Originally $5.95 Were $3 and $4 |-55 WOODWARD & LOTHROP 13, in ootton organdy and mar* 13 Summer cotton robes in woven checks lightweight quisette, in pastels and white. 11th F and G district and cloth. Sizes 12 to 16. 10th Terry ’Teen-age and ehubtoee sises 12 Streets__Phone 8300_ 9 Lightweight Sleeveless Sweaters of all-wool. White and to 16. shades. Sizes medium, Were $2. Now f I.1S jfaatel small, large. 34 Girls’ and Teerf-agers’ Presses 82 Neckties for boys and, youths. Rayons and silks In light ; in cotton prints and organdy. Sises colors. 50c and 73c. Now..l8e and 25e Summery Originally 7 to 16. Were $3. Now-(1.95 27 pairs Socks in striped ribbed cotton. Sizes 10 and 10 H. and Were 39c pair. Now...8 pairs 81 12 Wool Coats, fitted straight- line 133 Boys’ Union Suits, one-piece, open seat, lightweight cot- styles. Brown, tan, navy, aqua, sises 14 and 16. ton mesh. No buttons, sizes 10 to 18. each_55c rose. Teen-age REMNANT Special, FRIDAY Originally 919.95 and $22.95. Thz Boys’ Store, Fourth Floor, Now 919.95 Invalids' Girls’ Apparel, Fourth Floor. Week-End Candy Trays Juniors' Pajamas, 95e SAVINCS 95 S2 Licorice Caramels, Originally $7.50 Originally pound—35c Merchandise is not returnable or not $2 20 pairs of juniors’ two-piece cot- Foiled Mint Squares, Remnant Day exchangeable; 6 wooden trays for serving or comfortable reading. ton pajamas, assorted stripes. Sises pounds -35c sent C. O. D. or on approval; telephone or mail orders not accepted.