Occupational Health, Safety, and Hygiene
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OCCUPATIONAL MEDICINE PROGRAM HANDBOOK October 2005
U.S. DEPARTMENT OF THE INTERIOR OFFICE OF OCCUPATIONAL HEALTH AND SAFETY OCCUPATIONAL MEDICINE PROGRAM HANDBOOK October 2005 This Occupational Medicine Program Handbook was prepared by the U.S. Department of the Interior’s Office of Occupational Health and Safety, in consultation with the U.S. Office of Personnel Management and the U.S. Public Health Service’s Federal Occupational Health service. This edition of the Handbook represents the continuing efforts of the contributing agencies to improve occupational health services for DOI employees. It reflects the comments and suggestions offered by users over the years since it was first introduced, and addresses the findings, concerns, and recommendations summarized in the final report of a program review completed in 1994 by representatives of the Uniformed Services University of the Health Sciences. That report, entitled “A Review of the Occupational Health Program of the United States Department of the Interior,” was prepared by Margaret A.K. Ryan, M.D., M.P.H., Gail Gullickson, M.D., M.P.H., W. Garry Rudolph, M.D., M.P.H., and Elizabeth Odell. The report led to the establishment of the Department’s Occupational Health Reinvention Working Group, composed of representatives from the DOI bureaus and operating divisions. The recommendations from the Reinvention Working Group final report, published in May of 1996, were addressed and are reflected in what became this Handbook. First published in 1997, the Handbook underwent a major update in July, 2000. This 2005 version of the Handbook incorporates the updates and enhancements that have been made in DOI policies and occupational medicine practice since the last edition. -
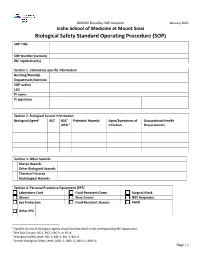
Biological Safety Standard Operating Procedure (SOP) SOP Title
IBSP005 Biosafety SOP template January 2021 Icahn School of Medicine at Mount Sinai Biological Safety Standard Operating Procedure (SOP) SOP Title SOP Number (version) IBC registration(s) Section 1. Laboratory-specific information Building/Room(s) Department/Institute SOP author LSO PI name PI signature Section 2. Biological hazard information Biological Agent1 RG2 BSL3 Potential Hazards Signs/Symptoms of Occupational Health ABSL4 Infection Requirements Section 3. Other hazards Sharps Hazards Other Biological Hazards Chemical Hazards Radiological Hazards Section 4. Personal Protective Equipment (PPE) Laboratory Coat Fluid-Resistant Gown Surgical Mask Gloves Shoe Covers N95 Respirator Eye Protection Fluid-Resistant Sleeves PAPR Other PPE 1 Specific strains of biological agents should be described in the corresponding IBC registration. 2 NIH Risk Groups: RG-1, RG-2, RG-3, or RG-4 3 Biological Safety Level: BSL-1, BSL-2, BSL-3, BSL-4 4 Animal Biological Safety Level: ABSL-1, ABSL-2, ABSL-3, ABSL-4 Page | 1 IBSP005 Biosafety SOP template January 2021 Section 5. Equipment and Engineering Controls Biological Safety Cabinet Centrifuge Aerosol-Generating Equipment Other equipment Section 6. Decontamination Disinfectant Contact Time Dilution Location Section 7. Waste Management/Disposal Steam Sterilizer Location: (Autoclave) Chemical Disinfectant(s) Location: Other Disinfectant(s) Location: Section 8. Transport Procedure(s) Page | 2 IBSP005 Biosafety SOP template January 2021 Section 9. Spill Response Procedure Section 10. Protocol Procedure Page | 3 IBSP005 Biosafety SOP template January 2021 Section 10. Protocol Procedure Continued (attach additional sheets if necessary) Page | 4 IBSP005 Biosafety SOP template January 2021 Section 11. Documentation of training and understanding. The Principal Investigator must ensure that all laboratory personnel receive training on the content of this SOP. -
Safety Data Sheets (Sdss) Information and Glossary
Safety Data Sheets (SDSs) Information and Glossary 2408 Wanda Daley Drive Ames, Iowa 50011 (515) 294-5359 | www.ehs.iastate.edu Copyright© Reviewed 2018 Safety Data Sheets (SDSs) Information Safety Data Sheets (SDSs) are informational sheets required by the Occupational Safety and Health Administration (OSHA) for hazardous substances (chemicals). The OSHA Hazard Communication Standard (29 CFR 1910.1200) and the Iowa Hazardous Chemical Risks Right to Know Standard (Iowa Administrative Code Section 875, Chapters 110-140) requires SDSs be “readily accessible” for any hazardous chemical in the workplace. Employees must be made aware of the SDS content and chemical storage location. SDSs can be obtained from manufacturers and distributors at the time of initial shipment. Each university workplace must maintain an SDS for each hazardous chemical in its inventory. SDSs that are available electronically meet the “readily accessible” criteria, as long as computer access is available to all employees whenever work is being conducted. EH&S suggests that each workspace also maintain paper copies of commonly used hazardous chemicals for ease of access. OSHA requires specific information be included on an SDS, in a 16-section format as described in the UN Globally Harmonized System of Classification and Labeling of Chemicals (GHS). The SDS must be in English and must include at least the following information: Section 1: Identification includes product identifier; manufacturer or distributor name, address, phone number; emergency phone number; recommended use; restrictions on use. Section 2: Hazard(s) Identification includes all hazards regarding the chemical; required label elements. Section 3: Composition/Information on Ingredients includes information on chemical ingredients; trade secret claims. -

Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19) and Considerations During Severe Shortages Interim Guidance 6 April 2020
Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages Interim guidance 6 April 2020 Background • avoiding touching your eyes, nose, and mouth; • practicing respiratory hygiene by coughing or This document summarizes WHO’s recommendations for the sneezing into a bent elbow or tissue and then rational use of personal protective equipment (PPE) in health immediately disposing of the tissue; care and home care settings, as well as during the handling of • wearing a medical mask if you have respiratory cargo; it also assesses the current disruption of the global symptoms and performing hand hygiene after supply chain and considerations for decision making during disposing of the mask; severe shortages of PPE. • routine cleaning and disinfection of environmental and other frequently touched surfaces. This document does not include recommendations for members of the general community. See here: for more In health care settings, the main infection prevention and information about WHO advice of use of masks in the general control (IPC) strategies to prevent or limit COVID-19 community. transmission include the following:2 In this context, PPE includes gloves, medical/surgical face 1. ensuring triage, early recognition, and source control masks - hereafter referred as “medical masks”, goggles, face (isolating suspected and confirmed COVID-19 shield, and gowns, as well as items for specific procedures- patients); 3 filtering facepiece respirators (i.e. N95 or FFP2 or 2. applying standard precautions for all patients and FFP3 standard or equivalent) - hereafter referred to as including diligent hand hygiene; “respirators" - and aprons. This document is intended for 3. -

Occupational Safety and Health Admin., Labor § 1910.145
Occupational Safety and Health Admin., Labor § 1910.145 of the workers or their families, shall (i) Fire protection equipment and appa- be provided in connection with all food ratus. [Reserved] handling facilities. There shall be no (ii) Danger. Safety cans or other port- direct opening from living or sleeping able containers of flammable liquids quarters into a kitchen or dining hall. having a flash point at or below 80° F, (3) No person with any communicable table containers of flammable liquids disease shall be employed or permitted (open cup tester), excluding shipping to work in the preparation, cooking, containers, shall be painted red with serving, or other handling of food, food- some additional clearly visible identi- stuffs, or materials used therein, in fication either in the form of a yellow any kitchen or dining room operated in band around the can or the name of the connection with a camp or regularly contents conspicuously stenciled or used by persons living in a camp. painted on the can in yellow. Red (j) Insect and rodent control. Effective lights shall be provided at barricades measures shall be taken to prevent in- and at temporary obstructions, as spec- festation by and harborage of animal ified in ANSI Safety Code for Building or insect vectors or pests. Construction, A10.2±1944, which is in- (k) First aid. (1) Adequate first aid fa- corporated by reference as specified in cilities approved by a health authority § 1910.6. Danger signs shall be painted shall be maintained and made available red. in every labor camp for the emergency (iii) Stop. -

Partnerships for Environmental Public Health (PEPH)
Partnerships for Environmental Public Health (PEPH) Environmental public health research aims to discover how the environment influences people’s health and translate research into action to address harmful environmental exposures and health risks to the public. Redefining environmental public health research The PEPH program brings together scientists, community members, educators, health care providers, public health PEPH Key Principles officials, and policymakers to coordinate environmental public health research at local, state, regional, tribal, national, and • Engage diverse communities. global levels. The multilevel partnerships fostered by PEPH help these groups discover and share vital information about the link • Promote the worthiest science. between environmental exposures and disease, which can be • Respond to current issues. used to promote health and reduce the risk of disease. • Focus on prevention. A hallmark of the PEPH program is the active engagement • Foster unified, integrated, and synergistic activities. of communities in all stages of research, dissemination, and evaluation, to help prevent, reduce, or eliminate adverse health • Support research to improve theories, methods, outcomes caused by environmental exposures. The program and practice. emphasizes both scientific advances and translation of research • Share the value of scientific advances and into practical resources, such as toolkits, brochures, and videos translational efforts. to explain research findings to stakeholders, communities, • Promote research into action. and individuals. Examples of PEPH in action Improving environmental health literacy PEPH Goals As part of an ongoing effort to increase environmental health • Coordinate and integrate new and existing literacy, the Community Outreach and Engagement Core initiatives that involve communities and scientists within the University of North Carolina at Chapel Hill Center for collaborating on environmental public health Environmental Health and Susceptibility, funded by the National research. -

Globalization and Infectious Diseases: a Review of the Linkages
TDR/STR/SEB/ST/04.2 SPECIAL TOPICS NO.3 Globalization and infectious diseases: A review of the linkages Social, Economic and Behavioural (SEB) Research UNICEF/UNDP/World Bank/WHO Special Programme for Research & Training in Tropical Diseases (TDR) The "Special Topics in Social, Economic and Behavioural (SEB) Research" series are peer-reviewed publications commissioned by the TDR Steering Committee for Social, Economic and Behavioural Research. For further information please contact: Dr Johannes Sommerfeld Manager Steering Committee for Social, Economic and Behavioural Research (SEB) UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases (TDR) World Health Organization 20, Avenue Appia CH-1211 Geneva 27 Switzerland E-mail: [email protected] TDR/STR/SEB/ST/04.2 Globalization and infectious diseases: A review of the linkages Lance Saker,1 MSc MRCP Kelley Lee,1 MPA, MA, D.Phil. Barbara Cannito,1 MSc Anna Gilmore,2 MBBS, DTM&H, MSc, MFPHM Diarmid Campbell-Lendrum,1 D.Phil. 1 Centre on Global Change and Health London School of Hygiene & Tropical Medicine Keppel Street, London WC1E 7HT, UK 2 European Centre on Health of Societies in Transition (ECOHOST) London School of Hygiene & Tropical Medicine Keppel Street, London WC1E 7HT, UK TDR/STR/SEB/ST/04.2 Copyright © World Health Organization on behalf of the Special Programme for Research and Training in Tropical Diseases 2004 All rights reserved. The use of content from this health information product for all non-commercial education, training and information purposes is encouraged, including translation, quotation and reproduction, in any medium, but the content must not be changed and full acknowledgement of the source must be clearly stated. -

Environmental Sanitation and Water Borne Diseases
ENVIRONMENTAL SANITATION AND WATER BORNE DISEASES Dr.Harpreet Singh MD, DM (Gastroenterology) COMPONENTS OF ENVIRNOMENTAL SANITATION • WATER SANITATION • FOOD AND MILK SANITATION • EXCRETA DISPOSAL • SEWAGE DISPOSAL • REFUSE DISPOSAL • VECTOR AND VERMIN CONTROL • HOUSING • AIR SANITATION WATER SANITATION WATER ANALYSIS CONSISTS OF: • PHYSICAL • CHEMICAL • RADIOLOGICAL • BIOLOGICAL • BACTERIOLOGICAL WATER SANITATION • PUBLIC WATER SUPPLY MUST BE- – SAFE – REASONABLY SOFT – PLENTIFUL – CHEAP WATER SANITATION • HOUSEHOLD TREATMENT OF WATER – BOILING, i.e., beyond 2 minutes – CHLORINATION- 1-5ppm – IODINE TREATMENT- 10 drops per gallon – FILTRATION – AERATION What is a Water-Borne Disease? • “Pathogenic microbes that can be directly spread through contaminated water.” -CDC • Humans contract waterborne infections by contact with contaminated water or food. • May result from human actions, such as improper disposal of sewage wastes, or extreme weather events like storms and hurricanes. Climate Change Promotes Water-borne Disease • Rainfall: transport and disseminates infectious agents • Flooding: sewage treatment plants overflow; water sources contaminated • Sea level rise: enhances risk of severe flooding • Higher temperatures: Increases growth and prolongs survival rates of infectious agents • Drought: increases concentrations of pathogens, impedes hygiene Water Quantity and Quality Issues IPCC, 2007a Burden of Waterborne Disease • 1.8 million deaths (4 million cases) in 2004 due to gastroenteritis (WHO) – 88% due to unsafe water and poor sanitation Prüss-Üstün et al., 2008 Burden of Diarrheal Diseases • Diarrheal diseases are vastly underestimated – 211 million cases estimated in the US annually (Mead et al., 1999) Reported cases Actual cases > 38 x reported cases Diarrheal Disease Pathways Prüss-Üstün et al., 2008 CHOLERA Cholera • Found in water or food Global Prevalence of Cholera (WHO) sources contaminated by feces from an infected person • Transmitted by contaminated food, water • Prevalence increases with increasing temperature and rainfall amounts V. -

Role and Value of the Corporate Medical Director
ACOEM GUIDANCE STATEMENT Role and Value of the Corporate Medical Director J. Brent Pawlecki, MD, MMM, Wayne N. Burton, MD, Cherryl Christensen, DO, MS, K. Andrew Crighton, MD, Richard Heron, MB, ChB, FRCP, T. Warner Hudson, MD, Pamela A. Hymel, MD, MPH, and David Roomes, FFOM, FACOEM, ACOEM Corporate Medical Directors Section Task Force accreditation in occupational medicine or the more preferred double The role of the corporate medical director (CMD) has evolved over the last certification in occupational medicine, and another board such as 300 years since Ramazzini first identified diseases of Italian workers in the 01/04/2019 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3VFjldD2uL9p7SMbj5XQFggscApMlmW/UgXNoK/5MD7Gq31Q2YQqh0A== by https://journals.lww.com/joem from Downloaded Downloaded internal medicine or family medicine. Further qualifications such as a early 1700s. Since then, there has been a gradual blurring of the boundaries master of public health or masters-level degree in environmental between private and workplace health concerns. Today’s CMD must have health, business administration, or law are highly desirable, including from intimate knowledge of their corporation’s industry and the businesses that knowledge of epidemiology, biostatistics, population health manage- https://journals.lww.com/joem they support, particularly the occupational and environmental programs that ment, business management, and regulatory aspects of employee comply with all local, state, and/or national standards and regulations. health. CMDs should also remain active in their relevant professional Leading companies not only measure compliance with such standards but health organizations to demonstrate that they are remaining current in also may hold programs to their own internal corporate global standards even medicine. -

TIN CAS Number
Common Name: TIN CAS Number: 7440-31-5 RTK Substance number: 1858 DOT Number: None Date: January 1986 Revision: April 2001 ------------------------------------------------------------------------- ------------------------------------------------------------------------- HAZARD SUMMARY WORKPLACE EXPOSURE LIMITS * Tin can affect you when breathed in. OSHA: The legal airborne permissible exposure limit * Contact can irritate the skin and eyes. (PEL) is 2 mg/m3 averaged over an 8-hour * Breathing Tin can irritate the nose, throat and lungs workshift. causing coughing, wheezing and/or shortness of breath. * Tin can cause nausea, vomiting, diarrhea and abdominal NIOSH: The recommended airborne exposure limit is pain, headache, fatigue and tremors. 2 mg/m3 averaged over a 10-hour workshift. * Tin can cause "spots" to appear on chest x-ray with normal lung function (stannosis). ACGIH: The recommended airborne exposure limit is 3 * Tin may damage the liver and kidneys. 2 mg/m averaged over an 8-hour workshift. * High exposure can affect the nervous system. WAYS OF REDUCING EXPOSURE IDENTIFICATION * Where possible, enclose operations and use local exhaust Tin is a soft, white, silvery metal or a grey-green powder. It ventilation at the site of chemical release. If local exhaust is found in alloys, Babbitt and similar metal types, and is used ventilation or enclosure is not used, respirators should be as a protective coating and in glass bottle and can worn. manufacturing. * Wear protective work clothing. * Wash thoroughly immediately after exposure to Tin. REASON FOR CITATION * Post hazard and warning information in the work area. In * Tin is on the Hazardous Substance List because it is addition, as part of an ongoing education and training regulated by OSHA and cited by ACGIH and NIOSH. -

DEPARTMENT of ENVIRONMENTAL HEALTH SCIENCES Programs Interim Chair: Charles Miller, III, Phd
2021-2022 1 DEPARTMENT OF ENVIRONMENTAL HEALTH SCIENCES Programs Interim Chair: Charles Miller, III, PhD Mission The Department of Environmental Health Sciences conducts research and educates culturally competent scientists and leaders to address the impact of the environment on the health of populations through scholarly research and hands-on practice experiences in public, private, not-for-profit and academic sectors around the world. About EHS The Department of Environmental Health Sciences (EHS) engages in multi-faceted research and prepares culturally competent professionals to address all aspects of our environment: physical, chemical, biological, social, and policy. The health of communities is inextricably linked to the environment and pollutants disproportionally impact minority populations. Safe air, water, soil, and food are prerequisites for health. EHS graduates are leaders in public, private, not-for-profit and academic sectors globally. The EHS transdisciplinary research portfolio spans basic toxicology to clinical biomarker science and community-engaged environmental health studies. We place priority on countering environmental health disparities locally, in the Gulf Coast region, across our nation, and around the world. EHS faculty have expertise in environmental health, toxicology, water quality, industrial hygiene, environmental health policy, community-based studies and resiliency. Graduate Degrees • Disaster Management, MPH (https://catalog.tulane.edu/public-health-tropical-medicine/environmental-health-sciences/disaster-management- -
CONFINED SPACE ENTRY PROGRAM University of Wisconsin-Superior Revised June 2014
University of Wisconsin - Superior Confined Space Program Revised June, 2014 CONFINED SPACE ENTRY PROGRAM University of Wisconsin-Superior Revised June 2014 Section 1 INTRODUCTION A confined space is, by definition, a space that is large enough and so configured that an employee can enter and perform work, has a limited or restricted means for entry or exit and is not intended for continuous human occupancy. Examples of confined spaces include boilers, hoppers, underground vaults, tanks, sewers, storage bins, crawl spaces, pits, ducts, tunnels, diked areas, vessels, and silos. The entry procedures to be used to enter a confined space are determined based on the space classification as either a non-permit or permit-required confined space. A non-permit confined space is a confined space has a safe atmosphere to work in and no other hazards capable of causing death or serious physical harm. A permit-required confined space is a confined space with existing or potential hazards that significantly increase the risk to the employee. These hazards include hazardous atmospheres, electrical hazards, unguarded moving parts, a severely restricted exit from the space, engulfment hazards, converging walls, sloping floors, falls from heights exceeding 6 feet, or any other recognized serious safety or health hazard. Often, work like welding or painting within a non- permit confined space, might introduce significant hazards, and the normal classification of the space would be upgraded to a permit-confined space. The general entry procedure involves a team of individuals, including the employee’s supervisor, the entrant, an attendant and entry supervisor. The classification of the space as a permit or non- permit space determines what steps and personnel are needed to make the entry.